Editorial, J Trauma Stress Disor Treat Vol: 5 Issue: 1
The Relationship between Persistent Post Concussive Symptoms and Post Traumatic Stress Disorder in Children–A Call for an Integrative View
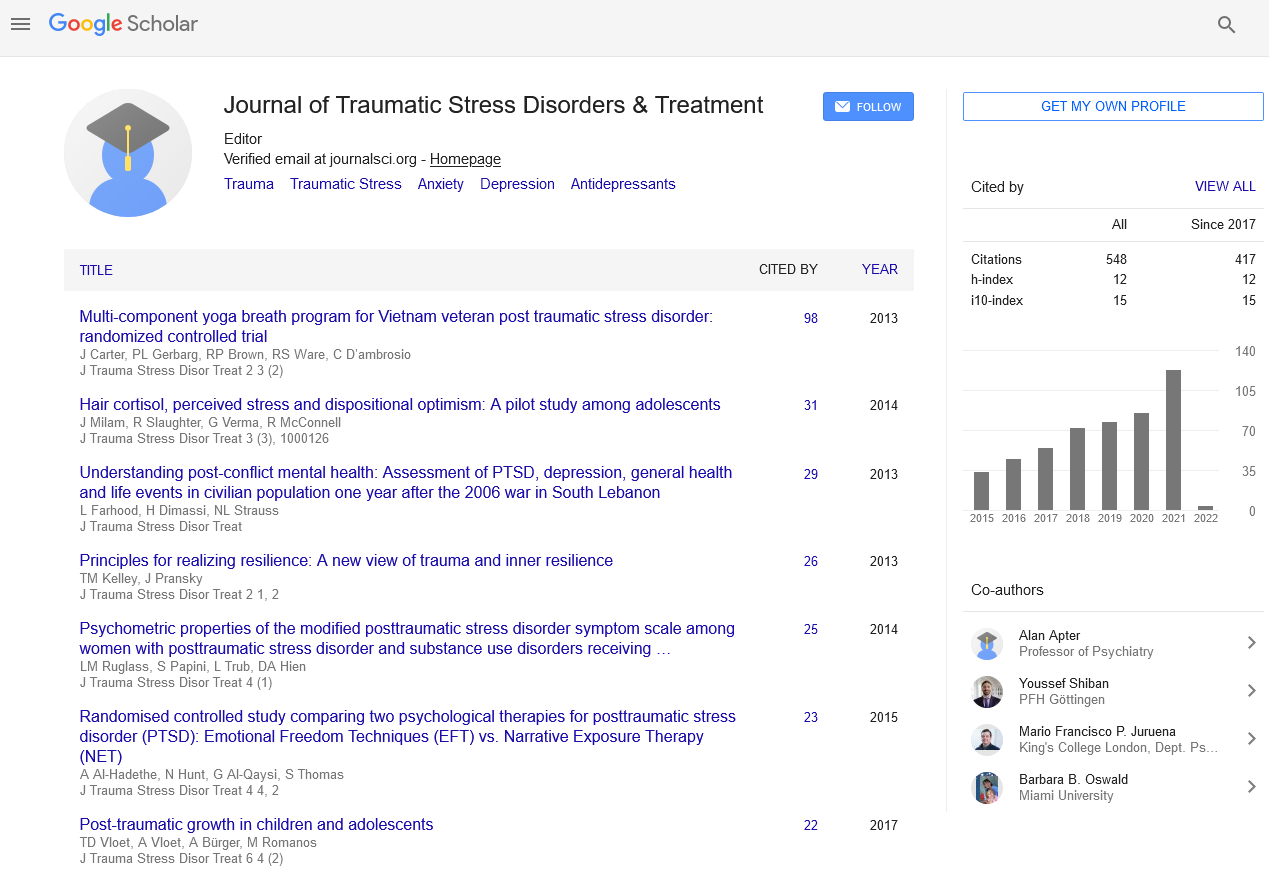
| Maayan Shorer* and Alan Apter |
| Psychological Medicine Department, Schneider Children’s Medical Center of Israel Petach Tikvah, Israel |
| Corresponding author : Dr. Maayan Shorer Psychological Medicine Department, Schneider Children’s Medical Center of Israel, 14 Kaplan St., Petach Tikvah, Israel E-mail: maayans@clalit.org.il |
| Received: March 06, 2015 Accepted: March 07, 2016 Published: March 10, 2016 |
| Citation: Shorer M, Apter A (2016) The Relationship between Persistent Post Concussive Symptoms and Post Traumatic Stress Disorder in Children–A Call for an Integrative View. J Trauma Stress Disor Treat 5:1. doi:10.4172/2324-8947.1000e107 |
Abstract
The Relationship between Persistent Post Concussive Symptoms and Post Traumatic Stress Disorder in Children–A Call for an Integrative View
Children suffering from Traumatic Brain Injury (TBI), often present significant diagnostic and therapeutic challenges. TBI may occur during a motor vehicle accident, a fall, a violent assault, sports injuries, etc. It results from a blunt impact or other mechanical force applied to the head [1], involving one or more of the following: loss of consciousness, loss of memory for events immediately before or after the accident, alternation in mental state at the time of the injury, or focal neurological deficits [2]. The vast majority of TBIs in children are of mild severity [3], which account for 80-90 % of all brain injuries [4].
Keywords: Traumatic brain injury, Violent assault, Post Traumatic Stress Disorder, Post Concussive, Traumatic Stress
| Children suffering from Traumatic Brain Injury (TBI), often present significant diagnostic and therapeutic challenges. TBI may occur during a motor vehicle accident, a fall, a violent assault, sports injuries, etc. It results from a blunt impact or other mechanical force applied to the head [1], involving one or more of the following: loss of consciousness, loss of memory for events immediately before or after the accident, alternation in mental state at the time of the injury, or focal neurological deficits [2]. The vast majority of TBIs in children are of mild severity [3], which account for 80-90 % of all brain injuries [4]. |
| One of the most common acute outcomes of mild TBI (mTBI) is a set of physical, emotional and cognitive symptoms, known as Post Concussive Syndrome (PCS). Typically PCS includes physical or somatic symptoms, such as headache, dizziness, and visual disturbances; cognitive impairments, such as attention, memory, and executive dysfunction; and emotional or behavioral problems such as irritability, anxiety, depression, affective lability, apathy, and/ or impulsivity [5]. In the DSM-5 PCS is now subsumed under the heading of “minor neurocognitive disorder”. |
| In the majority of cases, PCS fully resolves over the 4 to 12 weeks following the head injury [5-7]. However, 5-30% of children with mTBI, depending on its definition, do not exhibit the typical recovery and develop persistent post concussive symptoms (PPCS), which might linger on for months and even years after the injury [6,8-13]. As presently defined, PPCS represents symptoms enduring for longer than three months [14]. |
| Clinicians who encounter children presenting PPCS may find themselves confused over whether these symptoms are the result of a head injury or the manifestation of an emotional reaction to the traumatic event. The most obvious reason for this confusion lies in the fact that both PPCS and Post Traumatic Stress Disorder (PTSD) share many similar features. For example, both conditions may involve irritability, insomnia, restlessness, affective disturbances (e.g. anxiety and depression), and cognitive difficulties, such as attention difficulties, impaired concentration, memory, executive function and learning skills [15-20]. |
| Another major cause for the confusion is that PPCS are not specific to mTBI and may occur in the absence of a head injury, and are indeed frequently endorsed by healthy individuals [21-23]. |
| The effort to decide as to whether PPCS are the result of mTBI or PTSD may reflect a discriminative approach, attempting to differentiate between the “body” and the “mind”. In contrast, adopting an integrative approach will lead one to look for the reciprocal influences this two conditions may have on each other. Indeed, in the last few years, a growing body of research efforts (mainly on adult population) has adopted this view. |
| One line of investigating the reciprocity between mTBI and PTSD is asking whether the existence of one condition affects the risk or the intensity of the other condition. For example, Hovland and Raskin [24] found that following mTBI, the emergence of PTSD symptoms elevates the risk for presenting Post Concussive Symptoms and cognitive deficits |
| Other studies have focused on investigating the relative contribution of both mTBI and PTSD to PPCS. For example, Schneiderman, Braver, and Kang [25] found that among veterans population, PTSD was a stronger predictor of PPCS than a history of mTBI, even after controlling for overlapping symptoms. Another example is a pediatric study [26] that examined the correlation between PCS and PTSD symptoms among mTBI and an orthopedic injury control group. Significant positive correlations were found between PCS and PTSD immediately after the injury as well as one year after in both groups. However, the correlations were higher in the orthopedic group than the mTBI group, suggesting a closer link between PCS and neurological dysfunction in the mTBI group. A recent pediatric study examined the relative contribution of injury vs. non-injury characteristics, as predictors of PCS and PPCS following mTBI [27]. In this study, injury characteristics predicted PCS in the first month following mTBI but showed a decreasing contribution over time. In contrast, non-injury factors (i.e., demographic variables, child premorbid symptomology, and family factors) consistently predicted PPCS at 3 and 12 months post-injury. It seems, that both injury related and non-injury related (i.e. psychosocial) factors should be taken in consideration in understanding the formation of chronic PCS. |
| A third route of investigating the reciprocal influences of PTSD and PPCS is inquiring through which mechanisms these two conditions interact. One good example is the comprehensive model, suggested in a recent paper by Donlon and Jones [28]. Their model includes neurobiological and cognitive factors as potential pathways through which post-traumatic stress reaction may serve as the mechanism for the expression and maintenance of PPCS after mTBI. According to this model, children with pre-morbid anxious tendency are more likely to respond to stressors, such as a head injury, with fear and distress. These children may also be more attentive to information perceived as threatening and more likely to cope with their stress using maladaptive cognitive strategies. Consequently, these children are more likely to experience post-traumatic stress symptoms and to attribute their physical, cognitive, and emotional responses to the TBI. They are more attuned to the potential threat that the symptoms pose to well-being, and they tend to catastrophize the meaning of the symptoms (e.g. “The damage will never heal”), thereby resulting in greater reports of chronic PCS. Indeed, illness maladaptive appraisals and expectations were found to be important predictors of outcomes in adults following mTBI [29,30]. |
| Although comprehensive, one aspect that is missing from Donlon and Jones’s model is the parents’ role in their child’s reaction to the trauma. Parental traumatic stress response, parental maladaptive appraisals of their child’s health state (e.g. catastrophizing appraisals), as well as parental practices (e.g. overprotecting the child) may serve as important mechanisms in the interplay between mTBI, PTSD and PPCS. |
| In our opinion, the movement toward an integrative view on the relationship between PTSD and PPCS is compelling not only in research, but also in clinical practice. This statement may be actualized through the cooperation of neurologists, psychiatrists, psychologists and neuropsychologists in the evaluation and treatment of children following mTBI, particularly when PCS becomes chronic. These clinicians should attempt to view the patient not via a categorical point of view (i.e. “Does the symptoms are the result of the head injury or not?”, “is it PTSD or PPCS?”), but rather by looking for reciprocal influences between the brain injury and the emotional reaction (i.e. “How does this child and his parent appraise the consequences of the head injury?”, “Is the child’s/child parent’s emotional reaction to the traumatic event more intense since it involves a head injury?” “Does the parent overprotect his child after the injury, thereby inhibiting him from healing?”). The evaluation process of children presenting PPCS should include physiological aspects (neurological evaluation, neuro-imaging techniques) along emotional, cognitive and behavioral aspects (psychiatric and psychological evaluation, neuropsychological tests, etc.). |
| In addition, treatment plans should be inclusive, taking into account both physiological and psychological factors. Psychological intervention should be considered, and this intervention should include elements focusing on the child’s emotional reaction both in relation to the traumatic event (e.g. processing the traumatic memory), and in relation to the brain injury (e.g. maladaptive appraisals regarding healing from the injury, maladaptive coping with the symptoms, etc.). Parents stress reaction following the child’s injury seems to be an important component of the treatment as well. |
| Thus far, research concerning the efficacy of psychological interventions in PPCS is particularly scarce [31]. One evidence from an uncontrolled study in adult population suggested that PPCS decreased following Cognitive Behavioral Therapy (CBT) that was focused on patient’s expectations, stress management and behavioral activation [32]. Other treatment studies focused on a psychoeducation intervention during the acute phase immediately following the injury and found this intervention as effective in reducing the risk for later PPCS [33]. This state of affairs calls for more research on the efficacy of psychological intervention in reducing PPCS. Such an effort would serve as a model for the integrative view. |
References |
|