Review Article, Cell Biol Henderson Nv Vol: 5 Issue: 1
The Role of MicroRNA in Adipose-derived Stem Cells for Skin Wound Healing
| Jianlan Liu1,2, Hongjun Zhai3, Tianyi Liu4, Fazhi Qi5, Jonathon Pleat6 and Ningwen Zhu1,2* | |
| 1Department of Dermatology, Reconstructive and Burns Surgery, Huashan Hospital, Fudan University, Shanghai-200040, China | |
| 2Department of Plastic, Reconstructive and Burns Surgery, Huashan Hospital, Fudan University, Shanghai-200040, China | |
| 3Department of Burns Surgery, AnGang Hospital, China Medical University, Anshan, China | |
| 4Department of Plastic Surgery, Huadong Hospital, Shanghai, China | |
| 5Department of Plastic Surgery, Zhongshan Hospital, Shanghai, China | |
| 6Department of Plastic, Reconstructive and Burns Surgery, Southmead Hospital, University of Bristol, Bristol, UK | |
| Corresponding author : Ningwen Zhu Department of Dermatology and Department of Plastic, Reconstructive and Burns Surgery, Huashan Hospital, Fudan University, Shanghai-200040, China Tel: 021-52888132 E-mail: drnwzhu@126.com |
|
| Received: January 03, 2016 Accepted: April 12, 2016 Published: April 18, 2016 | |
| Citation: Liu J, Zhai H, Liu T, Qi F, Pleat J, et al. (2016) The Role of MicroRNA in Adipose-derived Stem Cells for Skin Wound Healing. Cell Biol: Res Ther 5:1. doi:10.4172/2324-9293.1000122 |
Abstract
Wound healing is an intricate process whereby the skin, or similar tissues, repairs itself after injury. Impaired wound healing with loss of temporospatial orchestration of processes remains challenging and can be highly debilitating to patients. Recently, the novel strategy of administering mesenchymal stem cells (MSCs) derived from bone marrow, adipose tissues and other sources, has achieved high therapeutic efficiency in healing wounds. Adipose-derived stem cells (ASCs) are pluripotent stem cells with the ability to differentiate into different lineages and to secrete paracrine factors to initiate tissue regeneration. However, the exact molecular mechanism by which ASCs exert their function is not well characterized. MicroRNAs (MiRNAs) are important regulators of diverse cell functions and the cytokine network is necessary for endothelial cell migration, capillary formation, matrix metalloproteinase production, collagen synthesis and degradation. This review will focus on the significant role of MicroRNA within ASCs and how these are interlinked to the pathogenesis of wound healing.
Keywords: MicroRNA; Pluripotent stem cells; Mesenchymal stem cells
Keywords |
|
| MicroRNA; Pluripotent stem cells; Mesenchymal stem cells | |
Introduction |
|
| Acute wounds heal and regenerate according to a specific, sequenced process with overlapping phases: 1) hemostasis; 2) inflammation (usually within the first 24 hours post-injury); 3) proliferation (7 days after injury); and 4) remodeling [1,2]. However, the complexity of wound healing is modulated by the influence of local factors (such as ischemia, edema and infection) and systemic factors (for example, diabetes, age, hypothyroidism, malnutrition and obesity) [3]. Occasionally, some injuries evolve into aggressive, life-threatening wounds that are refractory to treatment. When both direct and indirect costs are accounted for, the cost of treating non-healing wounds has been estimated to be $5 billion annually in the USA alone [4]. Therefore, promoting wound healing is highly desirable since morbidity and quality of life are likely to improve in tandem with a reduction in the economic burden to the healthcare system. | |
| In the normal sequence of wound repair, haemostasis is the first process. It starts immediately with vasoconstriction of vessels driven by the contraction of vascular smooth muscle cells (VSMC). Vessels are sealed by fibrin clot. There is a localized release of cytokines, growth factors, and proteases from the environment of the clot; these are intimately involved in directing wound repair and include platelet-derived growth factor (PDGF), transforming growth factor-β (TGF-β), epidermal growth factor (EGF) and vascular endothelial cell growth factor (VEGF) [5]. Subsequently, there is an inflammatory phase that is vital to counter the risk of infection. Polymorphonuclear neutrophils phagocytose invading microbes and devitalized tissue debris which concentrates at the site of injury [6]. Later, monocytes infiltrate and differentiate into macrophages. These remove tissue debris and apoptotic cells. The third phase, re-epithelialization, is characterized by migration and proliferation of several types of cells within the wound including fibroblasts, keratinocytes and endothelial cells. Some of the fibroblasts differentiate into myofibroblasts [7,8]. In tandem with the generation of the new tissue, the fourth and final stage, remodeling occurs with re-differentiation of keratinocytes and fibroblasts to re-constitute the epidermal barrier. There is apoptosis of myofibroblasts, endothelial cells and macrophages [9]. The residual tissue is composed mainly of extracellular matrix (ECM) proteins, - essentially collagen type III - that will be degraded with time by the metalloproteinase produced by a variety of cell types; it is replaced by collagen type I [1]. Hypertrophic scar or keloid formation depends upon the proliferation and differentiation to muscle fiber cells, which can produce ECM, as well as epithelial-mesenchymal transition (EMT) which can be explained that the loss of epithelial functions is coupled to the gain of deleterious mesenchymal functions resulting in excessive matrix deposition during scar formation [10-12]. This process involves a disassembly of cell-cell junction including downregulation and relocation of E-cadherin as well as down-regulation and translocation of β-catenin from the cell membrane to the nucleus, actin cytoskeleton reorganization and up-regulation of mesenchymal molecular markers such as vimentin, α-smooth muscle actin (α-SMA), fibronectin and N-cadherin [13,14]. | |
| Adipose-derived stem cells (ASCs) are pluripotent stem cells that possess the ability to differentiate into different lineages. They can secrete paracrine factors that initiate tissue regeneration. Several studies have confirmed the beneficial clinical effect of ASCs in the treatment of musculoskeletal disorders due to their immunomodulatory actions, self-renewal and potential differentiation into chondrocyte, osteoblast, neurogenic or myogenic lineages [15,16]. As ASCs can be differentiated into adipocytes and endothelial cells in vitro, they represent a promising cell source for the setup of vascularized fatty tissue constructs [17]. Additionally, they have been successfully applied in the field of plastic and reconstructive surgery with diverse benefits including the epithelialization of skin defects, healing of chronic cutaneous wounds and breast reconstruction [18-21]. An abundant resource of adipose tissue in most patients, its ease of isolation and extensive proliferative capacities ex vivo make it an ideal cell type for the therapeutic targeting of non-healing wounds [22]. ASCs can exhibit very similar phenotypic features to bonederived mesenchymal stem cells (BMSCs) including the expression of cell surface CD markers that are classically associated with MSCs, together with the absence of other equivalent markers that are associated with cells of hematopoietic origin such as CD106 [23,24]. As a corollary, the overlap in markers that permit identification has led to a complex nomenclature as to very similar subsets of cells eg PLA cells, pre-adipocytes, SVF cells, adipose-derived adult stem cells, adipose stromal cells (also previously termed ASCs), adipose mesenchymal stem cells and adipose tissue-derived stromal cells, amongst others. For the purposes of this review, the term ASC will be used very specifically to identify a subpopulation of cells that have been defined by the consensus of the International Fat Applied Technology Society [25]. | |
| To establish ASCs therapy as a standard treatment, there needs to be a far greater delineation of the molecular mechanism by which they exert a wound healing effect. MicroRNAs (MiRNAs) are a class of small (approximately 22 nucleotide), non-coding, endogenous RNAs that play a role in gene regulation by pairing with messenger RNA transcripts of protein-coding genes to direct their post-transcriptional repression [26,27]. MiRNAs are important regulators of diverse cell functions as a result of cytokine signaling which can direct endothelial cell migration, capillary formation, matrix metalloproteinases production and collagen turnover. These miRNA molecules also control proliferation and differentiation of wound-specific cells and can determine extracellular matrix composition [28]. However, the role of microRNAs in ASCs during healing wound remains relatively unclear. This review focuses on the role of miRNAs, ASCs and their combined role from a therapeutic perspective during wound healing. | |
MiRNAs in Wound Healing |
|
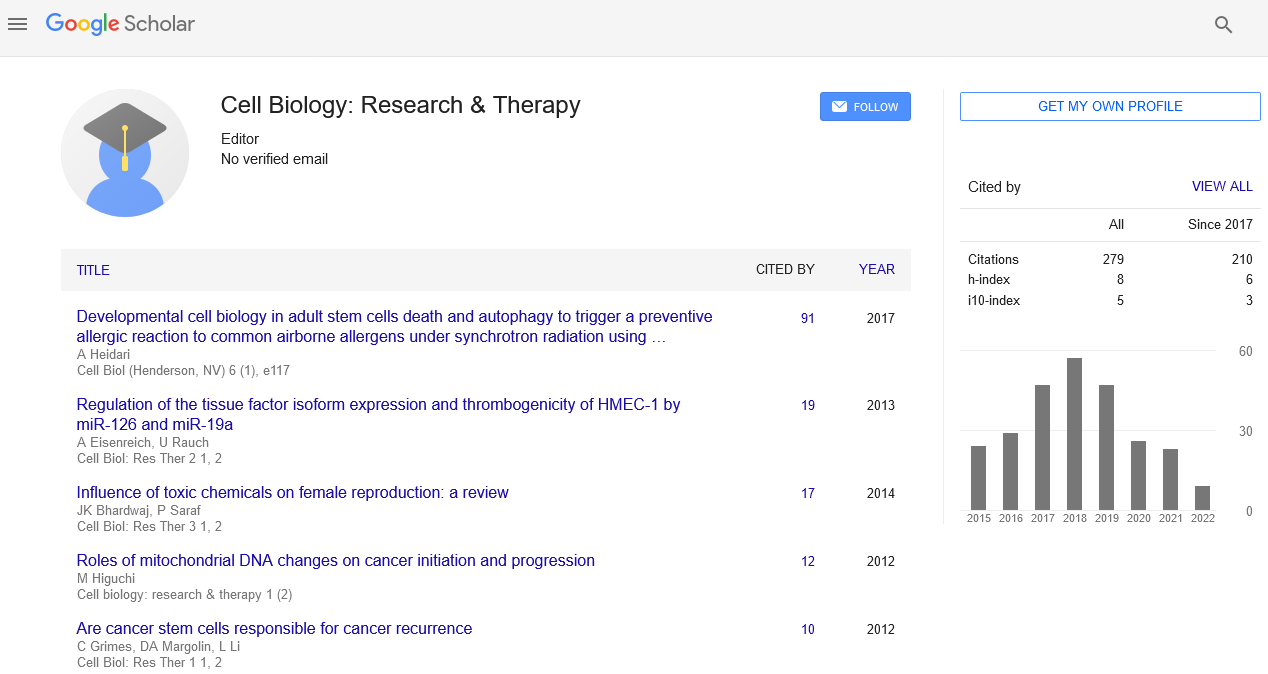
| Hemostasis: Hemostasis in the acute wound stereotypically is associated with vasoconstriction, fibrin clot and platelet degranulation. During this process, a number of mediators are released including PDGF, EGF, TGF-β, and VEGF [5]. In contrast, chronic wounds often fail to progress through the normal phases of healing and insidiously enter a prolonged, pathological state of inflammation [29]. One potential contributory microRNA defect that potentiates retarded healing is miR143-145 deficiency during haemostasis. It is associated with altered vasocontraction and impaired vasodilation of the microcirculation and this is likely to be a sequel to an abnormality of VSMC differentiation [30]. Another potential contributory factor at this early stages after injury is miR-15b induced by PDGF signaling; vascular smooth muscle growth is dependent upon this factor [31] (Figure 1). | |
| Figure 1: A diagrammatic representation of the phases of wound healing with the respective microRNA that has been implicated at each stage. | |
| Inflammatory phase: Following haemostasis, inflammatory cells are recruited to the injury site. A disordered inflammatory response is associated with excessive late fibrosis as a result of wound healing. Macrophages are known to affect different cells in wound healing, favoring keratinocyte proliferation and migration and promoting fibrocytes’ differentiation into myofibroblasts resulting from them in scars [32]. Depletion of monocyte-derived macrophages (MDMs) can reduce the production of growth factors that are essential to tissue repair [33]. And successful efferocytosis of apoptotic cells by MDMs can effectively resolve inflammation at a site of injury. The microRNA moiety, miR-21, is induced by efferocytosis and silences several downstream genes. These include PTEN and glycogen synthase kinase-3β (GSK3β) or tumor suppressor PDCD4 and Jun N-terminal kinase (JNK); in so doing, it ameliorates the inflammatory response triggered by lipopolysaccharide (LPS) [34]. Additionally, human monocyte/macrophage differentiation can be regulated by miR-424 as a result of an interplay with the transcription factors PU.1 and NFI-A as part of a regulatory circuit [35]. Toll-like receptors (TLRs) allow inflammatory cells to recognize pathogenic agents and are important components of the human innate immune response. Upon stimulation of multiple TLRs, the intermediary miR-147 functioned as a negative regulator of TLR-associated signaling events in murine macrophages [36]. Moreover, recent work demonstrated that an absence of expression of miR-155 produced an increased rate of wound closure. This was associated with the targeting of a diverse array of genes including BCL6, RhoA, SHIP1 and the inflammatory zone-1 (FIZZ1) gene that is associated with deposition of type-1 collagen [37]. | |
| Proliferation and granulation phase: Re-epithelialization can be achieved by the proliferation of keratinocytes and activation of epidermal stem cells to divide and migrate. The latter reside in the hair follicle bulge region and in the basal layer of epidermis. They are mobilized during the inflammatory phase [38-40]. Keratinocyte migration and re-epithelialization can also be regulated by miR- 21, which is one of the few microRNAs that have been relatively well studied in wound healing [41]. Aberrant expression of miR-21 and another microRNA, miR-130a, leads to inhibition of the EGF pathway through early growth response protein 3 (EGR3). In this manner, wound healing is retarded and it may be an underlying factor contributing to the failure of extrinsic EGF to accelerate healing in chronic wounds [42]. From the inflammatory through to the proliferative phase, recent evidence suggests that miR-31 is up regulated in keratinocytes at the wound edge in comparison with intact skin [43]. Epithelial membrane protein 1 (EMP-1) is a direct target of miR-31 in keratinocytes, which promotes skin wound healing by enhancing keratinocyte proliferation and migration [43]. Granulation tissue formation is vital in wound healing and angiogenesis, the formation of new blood vessels from pre-existing vessels, is one of the pivotal mechanisms driving it. Oxygen and nutrients are supplied by a network of new capillaries [44]. The cellular redox environment in human microvascular endothelial cells (HMECs) could be modulated by miRNAs via an NADPH oxidasedependent mechanism [45]. Hypoxia-sensitive miR-200b induces angiogenesis by directly targeting the transcription factor Ets-1 in HMECs [45]. In keeping with the fundamental requirement for angiogenesis to drive wound healing, a spectrum of other microRNA molecules have been implicated in this process by their modulation of the molecule vascular endothelial growth factor (VEGF); these include miR-15a [46], miR-16 [46], miR- 20b [47], miR-101 [48], miR-205 [49] and miR-206 [50]. | |
| Remodeling or scar formation phase: The remodeling or ‘scar formation’ phase is the last in the temporal sequence of wound healing. It is characterized by the re-differentiation of keratinocytes, the apoptosis of cells forming granulation tissue, fibroblast proliferation, and the synthesis of a variety of ECM components including proteoglycans, collagen and glycosaminoglycans. However, a dysfunction of this stage may lead to excessive scarring [51,52]. A prolonged or excessive inflammatory phase is believed to be the driver of excessive fibro proliferative scarring as exemplified by the clinical, pathological states of hypertrophic and keloidal scarring [53]. When an antagomir – a synthetic antagonist to a microRNA molecule – to miR-155 was applied to wound sites, pro-inflammatory factors IL-1β and TNF-α was reduced while anti-inflammatory factor IL-10 increased. Consequently, there was a reduction of skin fibrosis suggesting an important role for this intermediary [54]. A pilot study demonstrated that miR-149, miR-203a, miR-222, miR-122 were also relatively concentrated in hypertrophic scar [55]. It has been reported that increased miR-203, induces the differentiation of keratinocytes and acts as a switch between keratinocyte proliferation and differentiation by targeting p63 [56]. Another study indicated that TGF-β1 induces miR-145 expression in fibroblasts, which in turn inhibits KLF4, a known inhibitor of α-SMA [57]. There was subsequent up-regulation of α-SMA expression in hypertrophic scar, known to be associated with a contractile fibroblast phenotype and scar activity [57]. | |
| Many other miRNAs moieties have been implicated in wound repair. A representative sample is documented in Table 1. MicroRNAs are differentially expressed spatially across a wound and notably with a different distribution in stem cell niches. This altered expression would benefit from further investigation given the primacy of stem cell division as a means of reconstitution of the epidermis. | |
| Table 1: The different microRNA species associated with the phases of wound healing. | |
| ASCs promoting wound healing: Studies have shown that ASCs can promote wound healing in a variety of different ways. One approach has been to investigate the effect of ASCs on the vascularization of tissue-engineered constructs. In vitro co-cultures of ASCs with outgrowth endothelial cells (OEC) in fibrin gels seem to enhance vasculogenesis [58]. There is an angiogenic protein interaction between the two cell types [58]. It also demonstrates that close proximity of endothelial cells and ASC is required for network formation; specifically, ASCs stabilize EC networks by establishing characteristics similar to pericytes. By induction of activin an expression, other work has identified that in vivo, OECs probably initiate a differentiation program into smooth muscle cell in adjacent ASCs and then propagate this differentiation to more distant ASCs [59]. | |
| With a focus on the inflammatory phase, clinical trials have looked at the therapeutic value of ASCs for fistula and other chronic wounds. They have shown to be very effective in controlling inflammation and improving the healing process [60-62]. During this phase, one potential molecule that that is released by ASCs is macrophage-stimulating protein (MSP) [63]. It is highly expressed in adipose-derived stem cells-conditioned medium (ASCs-CM). It not only works as an immunomodulatory and anti-inflammatory mediator but also promotes the migration of fibroblasts, enhances collagen synthesis and remodeling, and effectively improves wound healing [63]. | |
| During the subsequent proliferation and granulation phase, ASCs were shown to enhance neovascularization and to accelerate wound closure via the secretion of VEGF-A, hepatic growth factor (HGF), and FGF-2 in a full thickness excisional injury model in rats [64]. Advancing this work in clinical studies, ASCs were reported to improve tissue hydration and new vessel formation during the treatment of radiation-induced tissue damage [65,66]. The trophic functions of ASCs could also contribute to cutaneous healing independent to new vessel growth. For instance, in a streptozotocin-induced rat model, local administration of ASCs accelerated the closure of full-thickness excisional wounds and this did not require enhanced vasculogenesis [64]. Other studies have probed the differentiation potential of ASCs into endothelial and epithelial cell types, supporting their utility with or without a substrate (a silk fibrin-chitosam scaffold) to regenerate tissues [67,68]. | |
| In the final, remodeling phase of wound healing, a study by Kim et al. showed that application of ASCs significantly accelerated the re-epithelialization of cutaneous wounds by promoting human dermal fibroblast proliferation through direct cell–cell contact or via paracrine secretion of a variety of growth factors, including PGDF, basic fibroblast growth factor (bFGF) and TGFβ [69]. Some studies show that ASCs transplantation can suppress EMT by down regulating epithelial-mesenchymal transition (EMT) markers such as Snail gene and α-SMA [14]. | |
| Taken together, these studies indicate that ASCs contribute to wound repair and tissue regeneration by actively secreting growth factors, such as VEGF. In turn, these promote subsequent angiogenesis by the differentiation of ASCs into endothelial cells, epithelialization by the proliferation of keratinocytes, and the stimulation of dermal fibroblasts to ensure a mature scaffold in which all the processes can flourish. Though the exact mechanism by which ASCs participate in wound healing has not been completely delineated, a wealth of new data indicates that microRNA molecules may be instrumental as intermediaries. | |
MicroRNAs as the Effectors of ASC in the Treatment for Wound Healing |
|
| MicroRNAs are inextricably linked to ASC function in wound healing. Consequently, it is possible to target therapeutically certain miRNA moieties to more effectively heal wounds and this is achieved by manipulating the function of ASCs including the homing, proliferation and differentiation of different cells types as well as epithelial-mesenchymal transition (EMT). | |
| During hemostasis, the presence of soluble factors (growth factors, hormones, and small signaling molecules) regulate the migration and localization of ASCs through direct cell–cell interaction or indirectly, or through ASCs paracrine secretion [70]. TGF-β, a key growth factor elevated in the wound site in the early stages, stimulates an increase of miR-21 and promotes ASCs proliferation and differentiation in vitro [75]. Correspondingly, knockdown of miR-21 in wound bed delays the healing process [71,72]. A range of inflammatory cells releases VEGF during wound healing. It is a potent factor for both angiogenesis as well as ASCs proliferation. Recent studies suggest that it accelerates ASCs proliferation while retaining the multipotency of differentiation of these cells. The negation or enhancement of miR-199a-5p has demonstrated that it differentially regulates the expression of VEGF in ASCs [73]. | |
| The proliferation and inflammatory phase of wound healing is associated with migration and proliferation of a range of cell types. ASCs have also been shown to regulate miRNAs expression in wound healing by accelerating epithelialization and increasing granulation tissue and angiogenesis [74]. In diabetic mice models, the correction of the diabetic wound healing impairment with MSC treatment was associated with a significant increase in miR-146a expression [74-76]. Subsequently, there was decreased expression of pro-inflammatory genes IRAK1, TRAF6, and NF-kB and increased IL-6 and MIP-2 gene expression associated with granulation tissue [74-76]. In addition, miR-15b is a candidate as a key negative modulator in angiogenesis. It is repressed under hypoxia and results in an increased level of vascular endothelial growth factor (VEGF) [77]. An MSC-treated diabetic wound model exhibited significantly decreased miR-15b expression and also a significant increase in the gene expression levels of its proangiogenic target genes, B-cell lymphoma 2(BCL-2), hypoxia-inducible factor-1α (HIF-1α) and VEGFα [78]. | |
| In the final remodeling phase of wound healing, recent evidence suggests that ASC-conditioned medium can accelerate the differentiation of spiny layer keratinocytes (K10-positive cells) into granular layer keratinocytes (involucrin-positive cells) via the upregulation of miR-24 [79]. Overexpression of miR-24 repressed the production of cytoskeletal modulators such as PAK4 and Tks5. This suggests that miR-24 induces keratinocyte differentiation by means of controlling intercellular gap junction formation and cell migration [79,80]. | |
| ASCs can modulate microRNAs to improve wound healing and a range of studies has shown beneficial effects (Table 2). However, there is limited evidence to show the effect of miRNAs within ASCs on late vasocontraction and remodeling of pathological scars such as keloids and hypertrophic forms; this is despite ASCs treatment having been widely applied in scar treatment [20,81-83]. One general conclusion was that ASCs globally could correct dysregulation of aberrant miRNA expression in the early stages of wound healing. | |
| Table 2: MicroRNA and their effect on ASCs during wound healing. | |
| MicroRNAs from ASCs as enhancers of wound healing | |
| The more exact elucidation of the molecular mechanisms by which miRNAs function within ASCs could improve ASC-based cell therapy in wound healing. The localized microenvironment is important. Upon injury to the skin, stem cell homing - the mobilization and guidance of haemopoietic and other stem cells to the site of damage - has a key role in repair. However, the exact steps by which mesenchymal stem cells (MSCs) are liberated into peripheral blood before targeting ischemic tissues are not fully elaborated [84]. One problem is that in ex vivo culture for therapeutic usage, MSCs have a very labile cell surface receptor complement, which might influence their viability and efficacy to home on reinfusion. Consequently, the efficiency of exogenously delivered MSCs in their ability to localize to ischemic tissues or sites of inflammation from peripheral blood is currently problematic. Interactions between stromal cell-derived factor-1 (SDF-1α) that is expressed at the site of injury, and its cognate receptor CXCR4 on MSCs, are crucial for the recruitment of the latter to damaged tissues and for repair during inflammation [85]. MiR- 27b is a microRNA molecule that seems to modulate this process. It has unique concentration within the stem cell niche and probably suppresses MSC directional migration by down regulating of SDF-1α expression in the early post-burn stages of wound repair [86]. | |
| A large body of work underlines the importance of the interaction of cells with the extracellular matrix including: cell spreading [87]; the determination of cell shape [87,88]; matrix stiffness [88,89]; and integrin cell surface receptor engagement [90] and clustering regulating which cell lineages can be induced by a differentiation medium [91]. MiR-125b expression by MSCs in a culture medium was up-regulated by limiting cell-matrix adhesion by reduction of ERK phosphorylation within the integrin signaling pathway; this protected hMSCs from anoikis [92]. Of note, miR-125b is reportedly concentrated in several stem cells, most notably those of the skin [93]. MiR-125b inhibits the differentiation of skin stem cells without affecting their maintenance or activation [93]. However, whether miR-125b would affect ASCs in wound remains unknown. Moreover, microRNA-302 induces human ASC proliferation and inhibits oxidation-induced cell death through several targets; this particular miRNA can be used to enhance the therapeutic efficacy of ASCs transplantation in vivo [94]. Further, overexpression of miR-137 inhibited both ASC proliferation and adipogenic differentiation directly by targeting cell division control protein 42 homolog (CDC42) [95]. Sonic hedgehog (shh) is a widely expressed and potent gene affecting cells in an Autocrine/ paracrine manner and the division of stem cells [96,97]. It has been shown that mouse embryonic stem cells (ESCs) accelerated skin wound healing by shh-signaling through the down-regulation of E-cadherin, an effect dependent on mmu-miR-141 and -200b [98]. However, there is still limited evidence about whether ASCs applied to wounds regulate shh pathways van microRNA intermediaries. | |
| New work suggests that EMT what it actually means ‘the interaction between epithelium and mesenchyme during scar formation’ can be triggered by various growth factors, such as transforming growth factor beta (TGF-β) and platelet-derived growth factor-D (PDGF-D) [13]. During this late phase, EMT-related genes within ASCs may be elevated along with inflammatory cytokines; it suggests an intimate relationship with similarities to EMT in hypertrophic scar induced by tumor necrosis factor-α through intermediaries such as bone morphogenic protein-2 [99]. The microRNA miR-34a, a p53 tumor suppressor, mediates repression of the Krüppel-type zincfinger transcription factor (ZNF281). In turn, this interacts with the transcription factors NANOG, OCT4, SOX2, and c-MYC that have been implicated in the regulation of pluripotency and stemness [100]. ZNF281 can be induced by the EMT-inducing transcription factor (EMT-TF) SNAIL [100]. So, SNAIL, miR-34a and ZNF281 form a feed-forward regulatory loop, which is one means by which EMT may be controlled both temporally and spatially [100]. Therefore, there is a clear pathway by which microRNA may play a role in wound healing by regulating EMT within ASCs. However, there is yet to be direct evidence of about the therapeutic effect of modifying miR-34a in ASCs during the treatment of human skin wounds. Optimistically, microRNA regulation is a seemingly worthwhile strategy for controlling the behavior of ASCs in wound healing. Recent work demonstrated that the conjugate PC-miR-148b-SNP, a mimic of miRNA-148b, added to ASCs bound to silver nanoparticles (SNPs), could successfully modulate gene expression for improved closure of a critical size bone defect [101]. | |
| ASCs micro vesicles contain microRNAs and mediate wound healing | |
| Micro particles are cell-derived, membrane-encapsulated structures that are believed to shuttle proteins, mRNA and miRNA to specific targets, both local and remote from the originating cell. They are thought to play a role in the adaptive response to injury by transferring gene information [102]. Recent studies have shown that MSCs secrete RNA-containing micro particles, also termed microvesicles (MVs) [103,104]. MVs are lipid microparticles that are <1 mm in diameter and are released from most cell types including as cancer, blood, endothelial and stem cells such as MSCs. They facilitate miRNA-mediated intercellular communication by conveying pre-miRNA [105,106]. As an example of the remote signaling role that these molecules can achieve, microRNAs increased in BMSC exosomes that overexpressed miR-23b were taken up by metastatic breast cancer cells in BM-MSC-conditioned medium or from exosomes isolated from BM-MSC cultures. For both, the MV constituents were able to induce a dormant phenotype through the suppression of a target gene, MARCKS, which encodes a protein that normally promotes cell cycling and motility [107]. As another example, MVs from ASCs - and specifically from endothelial differentiation medium (EDM)-preconditioned ASCs - promoted angiogenesis and the delivery of miR-31. This was thought to contribute to the proangiogenic effect of targeting factor-inhibiting HIF-1, an antiangiogenic gene [108]. Therefore, early work is starting to suggest that MSCs, besides their better known roles in secreting growth factors, cytokines and extracellular matrix components, have a key role in the transfer of genetic information between MSCs and injured cells such as keratinocytes, fibroblasts and vascular endothelial cells; this may be an important mechanism responsible for MSCs protective effect in in wound healing (Figure 2). | |
| Figure 2: A schematic representation of the role of microRNAs and their interplay with ASCs during wound healing. | |
Perspectives and Concluding Remarks |
|
| Fat grafting has been widely adopted in the clinical setting owing to the suggested benefit of ASCs for regenerative healing and their ability of differentiate into a wide variety of cells. However, the molecular mechanisms by which they exert their effects remain relatively unknown [20]. MicroRNAs are generally expressed in the different stages of wound healing at stem cell niches; this colocalization has supported the theory that they are inextricably linked to MSC response to injury. Although all the phenomena of MSCs in wound healing cannot be explained alone by the secretion of growth factors and cytokines, microRNAs at the wound site seem to have a stimulating effect on ASCs by several signal transduction pathways with a consequent improvement in wound healing. Furthermore, the global effect of ASCs including the homing of stem cells, proliferation, differentiation and EMT, can also be mediated by microRNAs expressed in normal wound healing. As a corollary, microRNAs can be administered exogenously to promote wound repair by the modulation of the microenvironment at the injury site. Some of the function of microRNAs in wound healing appears to be the result of information exchange between MSCs and tissue-injured cells such as keratinocytes, fibroblasts and vascular endothelial cells [109,110]. A unifying theme may now be to therapeutically attempt to mimic the action of ASCs by harnessing microRNA molecules instead [111]; this will require a more thorough elucidation of their natural expression, molecular targets and clinical effects. | |
References |
|
|
|