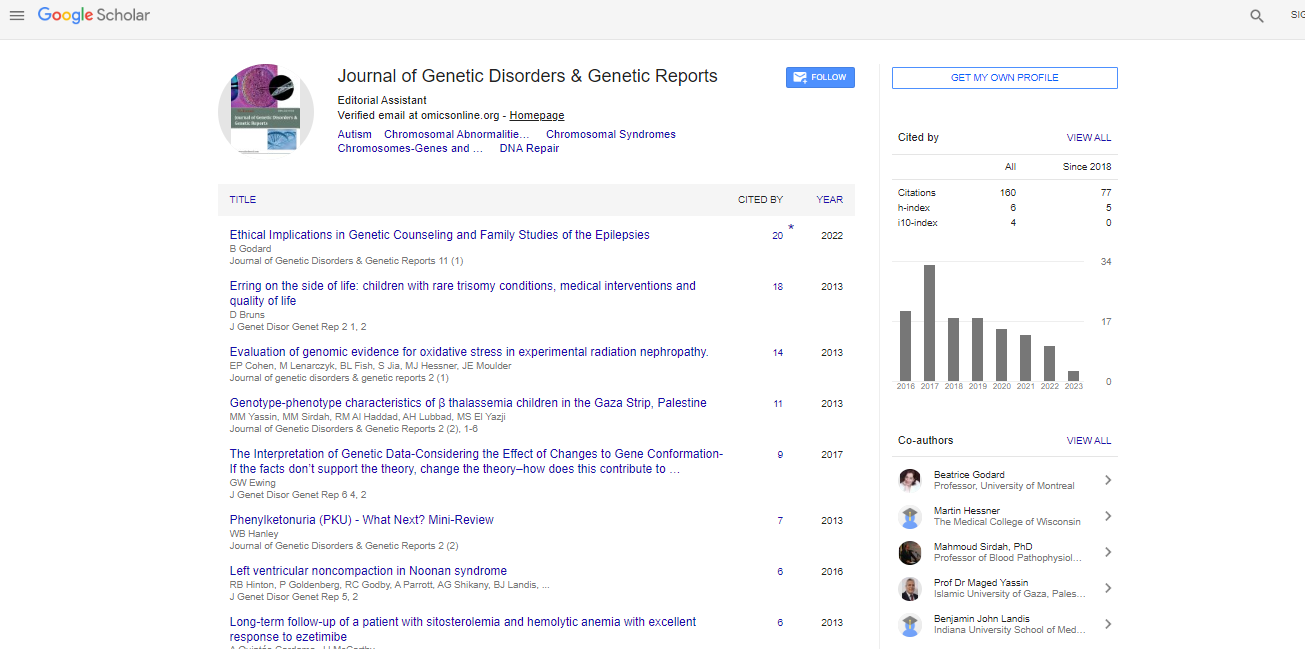
Review Article, J Genet Disor Genet Rep Vol: 2 Issue: 2
Phenylketonuria (PKU) - What Next? Mini-Review
| WB Hanley* |
| Division of Clinical & Metabolic Genetics, The Hospital for Sick Children at the University of Toronto, Canada |
| Corresponding author : Dr. WB Hanley Professor Emeritus & Honorary Physician, Division of Clinical & Metabolic Genetics, the Hospital for Sick Children at the University of Toronto, 555 University Ave, Toronto, Ontario, M5G 1X8, Canada Tel: 416-425-7846; Fax: 416-781-8515 E-mail: whanley@pathcom.com |
| Received: June 29, 2013 Accepted: November 26, 2013 Published: December 03, 2013 |
| Citation: Hanley WB (2013) Phenylketonuria (PKU) - What Next? Mini-Review. J Genet Disor Genet Rep 2:2. doi:10.4172/2327-5790.1000108 |
Abstract
Phenylketonuria (PKU) - What Next? Mini-Review
treatment of PKU is presented. This includes: 1. Worldwide expansion of newborn screening. 2. Uniform classification of the phenotypes. 3. Exploring the frequency of normal intellectual function in untreated patients. 4. Defining the reasons for suboptimal intellectual function in early treated PKU. 5. Developing centers of excellence for the treatment of adults with PKU. 6. Exploring new adjunct/alternative treatments/cures.
Keywords: PKU: Phenylketonuria; BH4: Tetrahydrobiopterin; NBS: Newborn Screening; PAH: Phenylalanine Hydroxylase; MS/MS: Tandem Mass Spectrometry; Phe: Phenylalanine; MRS: Magnetic Resonance Spectroscopy; MPKUS: Maternal PKU Syndrome; MRI: Magnetic Resonance Imaging; LNAA: Large Neutral Amino Acids
Abbreviations |
|
| PKU: Phenylketonuria; BH4: Tetrahydrobiopterin; NBS: Newborn Screening; PAH: Phenylalanine Hydroxylase; MS/MS: Tandem Mass Spectrometry; Phe: Phenylalanine; MRS: Magnetic Resonance Spectroscopy; MPKUS: Maternal PKU Syndrome; MRI: Magnetic Resonance Imaging; LNAA: Large Neutral Amino Acids | |
Introduction |
|
| Phenylketonuria (PKU) is one of the most common of the 300 or so known inherited metabolic diseases [1] with an incidence of 1:8,700 births in Europe and 1:15,000 in North America [2]. This extrapolates to a yearly total of 250 new patients in North America and 500 in Europe. It is present in all continents and nations. The known prevalence varies, country to country, from 1:1,700 to 1:200,000 births, for example: Latin America 1:20,996 [3], China/ Taiwan 1:11,000 to 1:19,412 [4,5] - but, overall, there is a significant worldwide occurrence. Over 500 alleles have been described [1]. The gene is located on chromosome 12q23.2 [1]. Untreated, the severe (“Classical”) form of PKU (about 50%-60% of cases) usually causes profound, permanent, intellectual disability in affected individuals. The disorder is caused by defective function of the enzyme phenylalanine hydroxylase (PAH) or, rarely, absence of a cofactor, Tetrahydrobiopterin (BH4). The enzyme/cofactor combination converts the amino-acid phenylalanine to tyrosine [1]. The subsequent excess tissue accumulation of phenylalanine results in permanent damage to the developing infant brain. Since the initial discovery of PKU in 1934 [6], the demonstration of its autosomal recessive nature in 1937 [7], the finding of the deficiency of phenylalanine hydroxylase activity in 1953 [8], the development of semi-synthetic phenylalanine-restricted diet therapy in 1954 [9] and the initiation of mass newborn PKU screening in 1963 [10] major steps have been made in the successful management of this disease. | |
| The results of early diagnosis and treatment have been spectacular but somewhat less than perfect. Even with early and adequate treatment, intellectual function falls short of unaffected sibs and parents, though basic IQ’s are usually “within the normal range” (90- 110) [11]. The major component of treatment is a rather onerous, expensive, semi-synthetic (“vegan-vegetarian” type), restrictedphenylalanine diet which requires frequent monitoring by specially trained genetic-metabolic dietician-nutritionists [12]. There is a high degree of dietary non-compliance, or poor compliance, in school age children, adolescents and adults [13] and lack of adult follow-up, leading to a significant incidence of adverse intellectual, neurological, neuropsychological and psychiatric consequences [14,15], some reversible, some not. This has led clinicians and researchers to explore other/adjunct modes of therapy. | |
| The purpose of this treatise is to review this author’s views on some of the most important projects and public health initiatives, for this disease, to be considered in the near future. | |
Proposed Projects |
|
| Universal newborn PKU screening | |
| PKU must be diagnosed and treated in the early days of life, before any clinical symptoms and signs appear, to prevent permanent damage to the very vulnerable neonatal brain. Universal neonatal PKU screening in North America (USA & Canada – 4 million and 479,000 neonates per year respectively) began, with a very few exceptions, between 1963 and 1975 [16], with close to 100% coverage, and in Europe (47 countries), for the most part, between 1966 and 1976 [17], but as late as 1993 (e.g. Estonia). Some European countries do not yet screen their neonates for PKU e.g. Armenia, Malta & Finland. The incidence of PKU in Finland is 1:100,000 to 1:200,000 births - one case every 2-3 years [18]. Screening is in place but no data is available from Albania, Azerbaijan, Georgia & Montenegro [19]. In other European countries Screening is incomplete e.g. Boznia, Serbia [19]. In Latin America (20 countries – including Mexico, The Caribbean, Central America and South America) newborn universal PKU screening is variable [3], beginning in the mid seventies in some countries, just recently in others and not at all in a few. Overall less than ¼ of the 11.2 million neonates born annually in Latin America are tested for PKU [3] even though the disease incidence is 1:21,000 births. In many of these countries economic and more pressing health problems supersede. In the Middle East & North Africa (21 countries, 10 million births per year) five countries have national programs and eight have limited programs. Israel has had a national program for many years but most other countries have just started in the last decade [20]. Because of high rates of consanguinity in this area (20- 50% of all marriages) genetic disorders are common. No estimates of the incidence or the actual percentage of newborns screened for PKU in this area are available. The Asia-Pacific Region (24 countries and ½ the births in the world) has PKU screening in just nine countries [21]. Australia, New Zealand (1965), Japan (1977), Taiwan (1993), South Korea (1997) & The Philippines (2000) have well established programs. The most populous countries: i) China (17million births per year, PKU incidence 1:11,000 to 1:22,000 [4,5,22]) – although newborn PKU screening is “mandatory” there is no reliable recent data. In 2007 [4], just 1-2% of all neonates in China were tested. Surprisingly, PKU screening has not yet been initiated in the Special Administrative Region (Hong Kong) [23]. ii) India/Pakistan/ Bangladesh/Indonesia (26 million births per year, PKU incidence 1:29,000 to 1:50,000 births [24,25]) – have no universal programs. Recent information [26] claims that “half of the newborn population in China has access to PKU newborn screening” and ½ the Philippine newborns are now screened, In Sub- Saharan Africa, “Black Africa” (population 800 million, the average woman has 5.4 children) no universal screening programs are in operation. In South Africa a pilot study (1979-86) found one case of PKU in 59,600 screened [27]. It was decided that a universal program would “not be cost-effective” and there were “more pressing health priorities”. The purported incidence of PKU in Blacks varies from 1:50,000 [24] to 1:100,000 [27]. Major economic and health problems - for example: i) 5% of the population (22.5 million people) has HIV, ii) The neonatal mortality rate is 91/1,000 births - might preclude the introduction of newborn PKU screening in the near future. | |
| It would appear, therefore, that less than 15% of the world’s newborns are tested for PKU. It would behoove the medical and public health communities in the developed world to come forth with policies to increase this total by providing economic, personnel and logistical support for the less fortunate countries and follow the examples of Germany & Japan. For the state of Qatar (population 800,000), the University of Heidelberg, Germany, has initiated a cooperative project whereby neonatal dried blood spots are analyzed for a broad range of inherited metabolic diseases, including PKU, by tandem mass spectrometry (MS/MS) with a very short turnaround time [28]. Costa Rica introduced expanded neonatal screening in 2004 thanks to the gift of a tandem mass spectrometer by the Japan Agency of International Cooperation [29]. Liaison with the University of Hamburg, Germany enabled Lebanon to start a newborn screening program with MS/MS in 2008 [30]. | |
| Develop an internationally agreed upon classification of the PKU phenotypes and decide if the mildest phenotype (“non- PKU mild hyperphenylalaninemia”-MHP) needs treatment | |
| Since universal newborn screening began milder phenotypes of PKU have been discovered. In the earlier days profoundly intellectually challenged, late diagnosed individuals with PKU usually had blood phenylalanine levels of >1200 μmol/L (normal range 70- 90 μmol/L). These patients have been labeled as “Classical PKU” and have been shown to have little or nil phenylalanine hydroxylase (PAH) activity. The most commonly used PKU phenotype classification [31] is shown in Table 1. | |
| Table 1: A Classification of the PKU Phenotypes [31]. | |
| Unfortunately there are a number of other classifications in the literature, causing confusion for the uninitiated reader and inability to compare individual studies or to carry out meta-analyses. These include variations by Gulberg [32], Lindner [33], Singh [34], Gassio [35], Moyle [36] and others. This paragraph is a plea for the international bodies overseeing the diagnosis and treatment of PKU to join forces and decide on a simplified and uniform phenotype classification. In addition the dilemma of the need to treat or not treat MHP should be further explored [37]. To date reports of detailed neuropsychological studies [38,39] have suggested that no treatment is necessary. However, recent publications have thrown doubt on these claims [2,40]. Larger, multicenter studies are indicated. | |
| Explore the presently unknown frequency of normal intellectual function in untreated PKU | |
| It is well known that some patients with untreated Classical & Mild/Atypical PKU have normal intellectual function. The numbers who have escaped intellectual disability in these two phenotypes are unknown. The epidemiologists and bioethicists vehemently remind us that no statistically valid studies have ever been carried out on PKU newborn screening [41] or on treatment [42]: i.e. no “control” (unscreened or untreated) jurisdictions or patients. The mantra that 98% of individuals with untreated (or late treated) PKU are profoundly retarded is deeply ingrained in the medical literature – e.g. McKusick’s textbook [43] states that “normal mentality is very rare among patients who have not received treatment”. This was based on very early (1957-1971) selection biased surveys of institutions for the retarded [44-47]. Later studies to verify or deny this [48-50] were burdened with epidemiological deficits or incorrect assumptions and came up with estimates from “very few” to 20%, of untreated PKU individuals having normal IQ’s. Of course, there is, usually, no reason to test unscreened adults with normal intelligence for PKU. Some diverse observations, however, have suggested a significant cohort of undiagnosed, untreated, intellectually normal individuals with PKU. The first report to tweak interest was that of Weglage and associates [51] describing 4 never treated adults with Classical PKU (phenylalanine blood levels > 1200 μmol/L), two intellectually handicapped and two with normal IQ’s. Magnetic resonance spectroscopy (MRS) revealed high brain Phe levels in the intellectually handicapped and low levels in the normally functioning individuals. Moats et al. [52] described similar findings. In retrospect two little-noted reports in the early days of newborn PKU screening were suggestive. Koch [53] and Berman [54] tested all the older, unscreened, sibs of their PKU patients diagnosed by newborn screening. Each found 15 with previously undiagnosed PKU. Three (20%) and four (27%) respectively, had normal IQ’s. | |
| How can we determine this? One possibility is to study the intellectual function of women with PKU who were undiagnosed/ untreated during their pregnancy and produced neonates with the maternal PKU syndrome (MPKUS) - maternal PKU embryopathy [55]. These fetuses are almost inevitably damaged in-utero by the high tissue levels of Phe (in fact there is a positive phenylalanine transplacental gradient – higher in the fetus [56]). They present with microcephaly, intrauterine growth reduction, congenital heart disease, facial dysmorphism and intellectual disability. In 1971-1981 Waisbren et al. [49] tested 453,118 umbilical cord blood samples for PKU and found 22 previously undiagnosed, untreated women with PKU. Two had Classical PKU (IQ’s 45 & 94), 11 had Mild/Atypical PKU (mean IQ 97.3) and 9 had MHP (Mean IQ 105.7). Hanley [17] reviewed the literature since 1990 and found reports of 60 women with previously undiagnosed PKU, most with relatively normal IQ’s, who produced 119 offspring, all profoundly damaged. This may represent, of course, a reverse bias of ascertainment, but it does suggest a significant incidence of normal intellectual function in untreated PKU. Hanley et al. [57] and Yi-Yung Hsai [58] have summarized a number of earlier single case reports of untreated individual with Classical PKU and normal intelligence. What is the reason for this heterogeneity? MRS might provide some answers. It is possible that a “modifier gene” may protect the brain by blocking/reducing the transport of Phe across the blood-brain barrier in some individuals with PKU. The current problem with MRS technology is that many centers have difficulty replicating the results of the German & Italian investigators [51,59]. Bik-Mutanowski et al. [60] (Poland), for example, articulated their frustrations in 2007 –“Brain phenylalanine measurements in patients with phenylketonuria; a serious diagnostic method or just reading tea leaves?”. A recent publication from the same authors suggests that they may have solved their puzzle [61]. They examined 30 PKU adults – 28 had abnormal neuropsychological tests. Two (6.6%) had normal testing and low brain Phe by MRS. If the kinks can be ironed out for this technology, it would seem that it should be part of the routine work-up and follow-up of all individuals with PKU. The proviso should be repeated testing of all who have initial low brain Phe levels as they reach adulthood – in view of the late onset of neurological and neuropsychological effects described in a few previously normally functioning adults [62] - the aging brain may become more permeable to Phe. | |
| Explore reasons for the less than optimal intellectual function in early diagnosed and “successfully” treated PKU subjects | |
| It is well known that early, continuous and successfully treated individuals with PKU have IQ’s within the normal range but 5-15 points below their unaffected sibs and parents [63]. These studies were done prior to 1984. Results may be better more recently with improved taste and variability of phenylalanine free “synthetic medical foods” and special low protein products plus improved skills of the treatment teams. Some of these less than optimal outcomes may be due to late initiation of diet (beyond 1-2 weeks of age) [58], “too high” recommended treatment levels or variability (“spiking”) of blood Phe levels during childhood [64]. Individuals with “well treated” PKU have been shown to display neuropsychological, neurological and mental health difficulties [14,15], beginning with the publication by Welch et al in 1990 [65]. These problems are worse if dietary treatment has been discontinued, or is in poor control but are not entirely absent in “well controlled” individuals. Since Welch’s paper a plethora of manuscripts (at least 75) have been published of studies on neuropsychological, neurological and psychiatric deficits in early treated PKU children, adolescents and adults whose standard IQ tests (WISC-R, WAIS-R etc) are within the “normal” range [14,15,66,67]. Many, but not all, of these deficits may be reversible if good dietary control is re-initiated. The consistent problem is that, after age 10 or 12, many/most PKU patients have Phe blood levels over the “recommended” range [68,69] or have discontinued diet therapy altogether, in fact, as many as 50% of adults are lost to followup [70]. Furthermore 50-90% of adults with Classical PKU are now not following their phenylalanine restricted diet [71-74] and 70% on treatment have levels above recommended values [68,69,75,76]. Are these “less than optimal results” due to late initiation of treatment, “spiking”, too high “recommended treatment levels”, individual brain susceptibility or inadequate dietary control? It is fine for the clinicians, psychologists, genetic counselors, biostatisticians et al. to recommend “tighter” control but the “in the trenches” dietician/ nutritionists (those who do all the work) are painfully aware of the extreme difficulty of accomplishing (unnecessarily tight?, impossible?) guidelines. The problem of “treatment fatigue” might enter into the equation and cause the patients/families to “give up”. It is inevitable for some “spikes” in Phe levels due, to catabolic episodes (usually a viral infection) despite super-vigilant patients and their families. | |
| Develop clinics (“Centers of Excellence”) with appropriate personnel and facilities in adult sites for treatment and follow-up of “Adult PKU” and “Maternal PKU”, including those lost to follow-up or “never treated” | |
| As outlined in the paragraph above, management and followup of adults with PKU, in most centers, is unsatisfactory – with the possible exception of maternal PKU. More adults than not are either lost to follow up or are in poor dietary control. Many of the adults who are still being followed are seen in pediatric units. The current consensus is that PKU treatment must be lifelong [77]. It is important that adults be cared for in adult centers [78]. There is now little doubt that high Phe levels are deleterious to brain function in adults with PKU [79]. Many, but not all, of these adverse effects may be reversible with return to dietary or biochemical control. The great majority of offspring from women with untreated classical or mild/ atypical PKU are profoundly neurologically compromised [17,80]. There is evidence that standard IQ measurements do not drop after the age or 12 years even if dietary control is suboptimal [72]. These observations, however, only hold ‘till early adulthood. No reports have surfaced for older PKU adults in this category but anecdotal reports of untreated PKU adult’s sudden neurological and behavioral changes in their 30’s and 40’s and published reports of similar deterioration in previously undiagnosed, normally functioning middle aged adults [62] are cause for concern. There is now little doubt that adults with poorly controlled PKU suffer neuropsychological, neurological and psychiatric difficulties (including adverse effects on mood) – many reversible, with return to good dietary control [15,81-83]. Treatment of never-treated, profoundly retarded adults, with PKU continues to be a challenge [84]. As an aside, a survey in the UK [85] (PKU prevalence 1:10,000) searching for undiagnosed adults with PKU expected to find 2,000 people, but only found 98. This may have been a fault in their survey method or perhaps large numbers of intellectually challenged individuals who have never been tested for PKU, but the other possibility remains that more than expected untreated adults with PKU might have relatively normal intellectual function. | |
| This is a plea for all PKU treatment centers to initiate facilities to investigate and treat adults fashioned after the clinic at the Charles Dent Metabolic Unit, The National Hospital for Neurology and Neurosurgery, London, UK [86]. | |
| Continue to explore alternative/adjunct treatments/“cure” for PKU | |
| Low phenylalanine diet therapy for PKU is onerous – consisting of a strict, basically, “vegan-vegetarian” diet with no high quality protein plus a semi-synthetic phenylalanine-free formula/medical food which contains essential amino-acids, carbohydrates, vitamins and critical trace elements, as well as special (expensive) low protein foods. Palatability used to be an issue but this has gradually improved. One problem is the social stigma of PKU individuals being unable to eat the same foods as their peers. It is a labor intensive process with constant oversight by metabolic dietician/nutritionists and regular blood tests. | |
| Promising new modalities of therapy have recently been introduced. These can be split into 2 groups: A. Adjunct/Alternative treatments and B. “Cures”. | |
| Adjunct/Alternative therapies | |
| Tetrahydrobiopterin ( BH4) - Kuvan™, Sapropterin™: BH4 is a cofactor for Phe metabolism. In those patients with some residual phenyalanine lhydroxylase activity it can act as a “chaperone” and boost the activity thereby lowering the blood Phe levels – first described by Kure et al. [87]. This is effective for the most part, but not exclusively [88], in the milder cases of PKU [89]. A large number of clinical trials have been completed [90,91] or are currently ongoing [92]. There is evidence that, aside from lowering the Phe levels, it is possible to allow more “natural” (high quality protein) foods [93]. There is even some evidence of benefit without effect on blood Phe levels [94]. | |
| Large Neutral Amino-acids (LNAA) – histidine, isoleucine, leucine, lysine, methionine, threonine, tryptophan, tyrosine, valine, phenylalanine: LNAA’s compete for transport across the blood-brain barrier via the L-type amino-acid carrier and high levels of one may inhibit the transport of others. Some of these alleged depleted brain LNAAs are precursors to certain neurotransmitters. It has been postulated that providing high concentrations of the other LNAAs might block the entry of Phe as well as enhancing brain levels of these critical precursors. Some earlier studies (animal and human) support this hypothesis: Anderson and Avins [95], Vorhees and Berry [96], Banos et al. [97] in rats and later, Knudsen et al. [98], Matalon et al. [99], Pietz et al. [100] and Schindeler et al. [101] in humans. Since the early 90’s adult PKU patients in Denmark have been routinely treated with LNAA supplements in the form of PreKUnit™ (Nilab, Dk) but no controlled studies of efficacy have been carried out. A new LNAA supplement PheBLOC™ (Applied Nutrition Corp, Cedar Falls, NJ, USA) has become available. Clinical trials are currently ongoing. | |
| “Cures” | |
| Enzyme Substitution Therapy – Phenylalanine ammonia lyase (Peg-Pal™ Biomarin, Inc): Phenylalanine ammonia lyase is a biological (plant) enzyme which metabolizes Phe to transcinnamic acid and a trace of ammonia – harmless metabolites. It has been shown to lower blood Phe by 36% to 96% (mean of 62%) [102,103]. Clinical trials, Phase 1 & Phase 2, are now ongoing in eight treatment centers in the USA [103]. The important advantage is that it should be effective in all phenotypes. Disadvantages include the development of immunogenicity and the fact that it must (so far) be given subcutaneously. | |
| Gene replacement therapy: To date, this approach has not been studied in humans but has shown encouraging results in the PAH emu2/emu2 mouse involving the use of the adeno-associated virus, causing prolonged lowering of blood Phe [104]. | |
| Liver cell transplantation/repopulation: A report of a child with PKU and unrelated cirrhosis, who underwent liver transplantation and was cured of his PKU [105] led to this focus of research [106]. Normally functioning liver cells can be introduced to the PKU liver and, if 10-20% of the liver activity is provided by these cells, the disease would be cured. The problem is that, if healthy cells are introduced, the native hepatocytes eventually replace the donor cells unless there is a selective growth disadvantage devised for the native cells (e.g. “partial” damage by radiation). Successful treatment with this method has been developed for several other inborn errors of metabolism – notably lysosomal and peroxysomal storage diseases [107]. A Clinical Trial is now ongoing in Pittsburgh, USA [108]. | |
Conclusion |
|
| Since the first description of PKU 78 years ago [6] spectacular advances in the diagnosis and treatment of have been made. As outlined above, however, there remain many exciting new prospects for improved therapy including permanent cure. | |
Acknowledgement |
|
| Supported by a Grant from the Maranatha Foundation, Toronto, Ontario, Canada. | |
References |
|
|
|