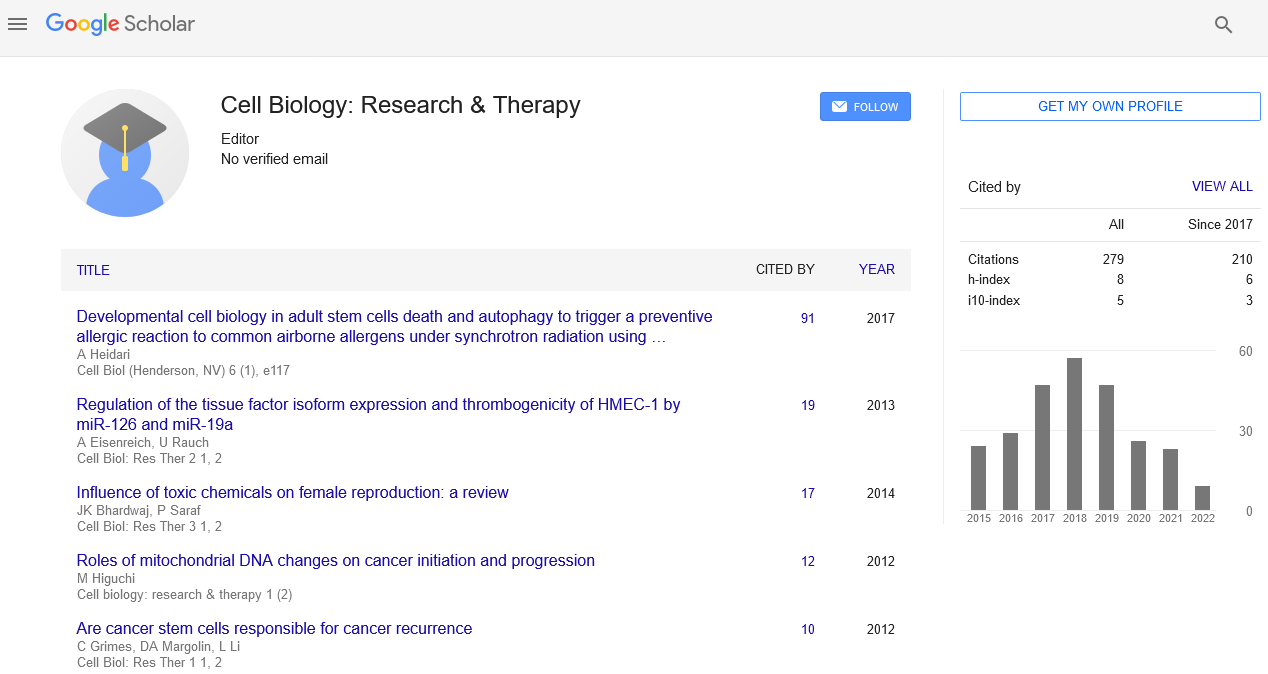
Research Article, Cell Biol Res Ther Vol: 2 Issue: 1
Regulation of the Tissue Factor Isoform Expression and Thrombogenicity of HMEC-1 by miR-126 and miR-19a
| Andreas Eisenreich* and Ursula Rauch |
| Charité – Universitätsmedizin Berlin, Campus Benjamin Franklin, Centrum für Herz- und Kreislaufmedizin, Berlin, Germany |
| Corresponding author : Andreas Eisenreich, PhD Charité – Universitätsmedizin Berlin, Campus Benjamin Franklin, Centrum für Herz- und Kreislaufmedizin, Berlin, Germany Tel: 0049 30 8445 2362 E-mail: andreas.eisenreich@charite.de |
| Received: January 29, 2013 Accepted: June 12, 2013 Published: June 17, 2013 |
| Citation: Eisenreich A, Rauch U (2013) Regulation of the Tissue Factor Isoform Expression and Thrombogenicity of HMEC-1 by miR-126 and miR-19a. Cell Biol: Res Ther 2:1. doi:10.4172/2324-9293.1000101 |
Abstract
Regulation of the Tissue Factor Isoform Expression and Thrombogenicity of HMEC-1 by miR-126 and miR-19a
Endothelial cells modulate the vascular wall homeostasis and blood thrombogenicity. Inflammatory conditions induce the Tissue Factor (TF) isoform expression and cellular thrombogenicity in endothelial cells. MicroRNAs (miRNAs) posttranscriptionally regulate gene expression. MiRNA-19 (miR-19) was shown to downregulate the TF expression in breast cancer cells. The role of miRNAs, such as miR-19a or the endothelial cellspecific miR-126 in the modulation of the endothelial TF expression and activity is unknown.
Keywords: microRNA; Tissue factor; HMEC-1; Thrombogenicity
Keywords |
|
| microRNA; Tissue factor; HMEC-1; Thrombogenicity | |
Introduction |
|
| Endothelial cells play an important role in the regulation of vascular wall homeostasis and blood thrombogenicity [1-3]. Inflammatory mediators, such as the cytokine tumor necrosis factoralpha (TNF-α) activate endothelial cells [4,5]. This lead to a switch from an anti- toward a pro-thrombogenic endothelial phenotype [6,7]. | |
| Tissue factor (TF), the primary initiator of blood coagulation, is expressed in two isoforms, membrane-bound full-length (fl) TF and soluble alternatively spliced (as) TF [3,6]. We recently demonstrated TNF-α to induce the expression of both TF isoforms [6,8]. FlTF was shown to be the major source of blood thrombogenicity [9]. It has been indicated that asTF participates in thrombogenesis in vivo, although the pro-coagulant activity of asTF is much lower than that of flTF [3,9,10]. Recently, it was suggested that asTF may be linked more closely to cell survival and pro-angiogenic processes [11-13]. | |
| MicroRNAs (miRNAs) are endogenous 20-25 nucleotides long RNAs, which regulate gene expression on post-transcriptional level by binding to the regulatory 3’-untranslated region (3’UTR) of a target messenger (m)RNA [14,15]. This consequently leads to inhibition of mRNA translation or promotes mRNA degradation [15]. MiRNA-mediated expression regulation was shown to play important roles in various physiologic and pathologic processes, such as metabolism, inflammation, immune response, oncogenesis, and thrombosis [16-21]. Recently, miRNAs have emerged as important modulators of TF-mediated (patho-) physiologic processes in the vasculature as well as in cancer settings [21,22]. Zhang et al. showed that miRNA-19 (miR-19) directly binds to the 3’UTR of the TF gene (F3) and negatively regulates the TF expression of breast cancer cells [23]. Moreover, other miRNAs, such as members of the miR-17 ~ 92 clusters or miR-106b were also suggested to be involved in TF expression regulation [22]. Furthermore, other miRNAs, such as miR-126 were known to play an important role for the endothelial function, especially under inflammatory conditions [24]. However, despite extensive literature on endothelial biology, it is unknown which miRNAs are involved in the regulation of endothelial TF expression and function under (patho-) physiologic conditions. Therefore, we set out to characterize the impact of inflammatory conditions on the expression of the endothelial miRNAs miR-19a and miR-126 [25]. Moreover, we analyzed the impact of these miRNAs on the TF expression and activity in resting as well as in inflammatory activated human microvascular endothelial cells (HMEC-1). | |
Materials and Methods |
|
| Cell culture | |
| Human microvascular endothelial cells (HMEC-1) were cultured in endothelial cell growth medium (PAA Laboratories GmbH, Colbe, Germany; # U15-002) containing 10% fetal calf serum at 37°C in a humidified incubator (5% CO2, 95% air). For transfection or stimulation experiments, HMEC-1 were switched to endothelial cell basal medium (containing 1% fetal calf serum) for 1 h and then treated as described below. For miR-19a and miR-126 inhibition 200 nM of anti-miR-19a (miRIDIAN hairpin inhibitor, Thermo Fisher Scientific, Waltham, MA, USA, # IH-300488-05) or anti-miR-126 (miRIDIAN hairpin inhibitor, Thermo Fisher Scientific, Waltham, MA, USA; # IH-300626-08) were transfected using Lipofectamine™ 2000 (Invitrogen GmbH, Karlsruhe, Germany; # 11668-027). As control a miRIDIAN microRNA hairpin inhibitor negative control (Thermo Fisher Scientific, Waltham, MA, USA; # IN-001005-01-05) was used. After 24 h the cells were stimulated with 10 ng/mL TNF-α (Sigma-Aldrich Chemie GmbH, Munich, Germany; # T6674) for 2 h for MiRNA expression analyses or 8 h for assessment of the TF protein expression and the cellular TF activity. | |
| TF Isoform-specific Real-time PCR (TaqMan®): Real-time PCR employing flTF, asTF, and GAPDH-specific primers and probes was performed as described [6]. In brief, total RNA was isolated and 1 μg RNA was reverse transcribed. After that Real-time PCR was performed using ABI Prism 7000 Sequence Detection System (Applied Biosystems, Carlsbad, CA, USA) under the following conditions: 50°C, 2 min; 95°C, 10 min; 40 cycles 95°C, 15 s; 60°C, 1 min. Results were quantified using double strand DNA standards. | |
| MiRNA expression analyses | |
| The miRNA expression was analysed via Real-time PCR (TaqMan®, Applied Biosystems, Carlsbad, CA, USA). HMEC-1 cells were stimulated with 10 ng/mL TNF-α for 2 h or 24 h, respectively. After that, total RNA was isolated using peqGOLD Trifast (# 302010, PEQLAB Biotechnologie GMBH, Erlangen, Germany). Both miRNAs miR-19a and miR-126 were reverse transcribed using the TaqMan® MicroRNA RT Kit (# 4366597; Life Technologies GmbH, Darmstadt, Germany). For Real-Time PCR analyses of miR-19a and miRNA-126 expression TaqMan® MicroRNA Assay Inv SM Kits (# 4427975; Life Technologies GmbH, Darmstadt, Germany) used were used following the manufacturer’s protocol. | |
| Western blot | |
| Western blot analyses were performed as previously described [6]. For detection specific monoclonal antibodies against flTF (anti-human Tissue Factor #4508; American Diagnostica GmbH, Pfungstadt, Germany) and GAPDH (anti-GAPDH clone 6C5; Calbiochem, Darmstadt, Germany) as well as polyclonal antibodies against asTF (anti-asTF C30; Pineda Antikorper-Service; Berlin, Germany) were used. Western blots were quantified using Gel-Pro Analyzer™ v4.0.00.001 (Media cybernetics, Maryland USA). | |
| TF activity assay | |
| Determination of total pro-coagulant activity of HMEC-1 cells was performed as described earlier [6]. | |
| Dual luciferase reporter assay | |
| Dual luciferase reporter assays were performed using the miTargetTM miRNA 3’UTR target clone pEZX-MT01, containing the 3’UTR of F3 (GeneCopoeia, Rockville, MD, USA; # HmiT054276- MT01) or the negative control vector (# CmiT000001-MT01). 2x104 HMEC-1 per well were co-transfected with 200 nM anti-miR-19a or anti-miR-126, respectively, and 200 ng of the luciferase reporter vector or the empty control vector in 96-well plates and a total volume of 100 μL endothelial cell basal medium per well. After 24 h the luciferase reporter assay (Luc-PairTM miR Luciferase Assay, Gene Copoeia, Rockville, MD, USA; # LPFR-M010) was performed, following the manufacturer’s instructions. Renilla luciferase activity was normalized to firefly luciferase activity. | |
| Statistical analysis | |
| All data were expressed as mean ± SEM. Data were analyzed by Student’s t-test or one-way ANOVA as appropriate. Statistical analyses were performed using GraphPad Prism v4.03 (GraphPad Software, Inc., La Jolla, CA, USA). A probability value ≤ 0.05 was regarded as significant. | |
Results |
|
| The impact of TNF-α on the expression of miR-19a, miR- 126, flTF and asTF in HMEC-1 | |
| The expression of TF isoforms as well as the cellular thrombogenicity was shown to be induced by TNF-α in endothelial cells [6]. Therefore, we first analyzed the impact of TNF-α treatment on the expression of the miRNAs miR-19a and miR-126 in HMEC- 1. MiRNA expression analyses showed that HMEC-1 express both miRNAs under normal conditions (Figure 1A, 1D). Activation of HMEC-1 with 10 ng/mL TNF-α significantly reduced the expression of miR-19a (Figure 1A, 1B) and miR-126 (Figure 1C, 1D). Next, we verified the effect of TNF-α on the TF isoform expression (Figure 1E, 1F). Treatment of HMEC-1 with TNF-α induced the expression of flTF (Figure 1E) as well as of asTF (Figure 1F) 2 h post stimulation. | |
| Figure 1: Expression of miR-19a and miR-126 in HMEC-1. Real-time PCR analyses of miR-19a (A, B), miR-126 (C, D), flTF (E) and asTF (F) mRNA expression in HMEC-1 2 h (A, C, E, F) and 24 h (C, D) post stimulation with 10 ng/mL TNF-α. (E, F) Non-stimulated cells (control) were compared to HMEC-1 stimulated with TNF-α (TNF-α). The expression of miR-19a or miR- 126, respectively, was normalized against RNU48 expression. The mRNA expression of flTF and asTF was normalized against GAPDH. The data were presented as relative (x-fold) change of mRNA expression. (+) p<0.001; (#) p<0.01; (*) p<0.05; (n.s.) no significant difference compared to control; n≥3. | |
| Interaction of miR-19a and miR-126 with the 3’UTR of F3 | |
| To determine whether miR-19a and/or miR-126 were able to regulate the TF isoform expression we performed in silico analyses regarding the interaction of these miRNAs with the 3’UTR of the TF gene (F3). First we checked whether the 3’UTR of F3 contains binding motifs for miR19a and miR-126. | |
| Using the Online micro RNA prediction tool of the Segal lab of computational biology (http://genie.weizmann.ac.il/%20pubs/mir07/mir07_prediction.html), we found that miR-19a and miR-126 were potentially able to bind to the regulatory 3’UTR of F3. Further structural analyses regarding the possible miRNA/Target mRNAa interaction were done using the RNA hybrid 2.2 data base (http://bibiserv.techfak.uni-ielefeld.de/rnahybrid/) and showed that miR- 19a as well as miR-126 were able to interact with the 3’UTR of F3 (Figure 2A, 2B). Moreover, the structure of this interaction complex fulfilled important needs for an adequate miRNA/target mRNA interaction, such a perfect base pairing between the nucleotides 2-8 (“seed region”) and the formation of a bulge in the central region of the miRNA/target mRNA duplexes [26]. | |
| Figure 2: Structural in silico analyses of the miRNA/target mRNA interaction. Shown are the results of in silico analyses regarding the possible structural interaction of miR-126 (A) or miR- 19a with the 3’UTR of the TF gene F3. The miRNA sequence (green) of miR-126 (A) is numbered continuously from nucleotide 1 to 22 and the sequence of miR-19a (B) is numbered from nucleotide 1 to 23. The sequence of the target mRNA is depicted in red. Additionally indicated is the “seed region” (nucleotides 2-8) and the “central bulge” of miR-126 or miR19a, respectively as two important criteria for an efficient miRNA/target mRNA interaction. Analyses were performed using the RNA hybrid 2.2 data base (http://bibiserv.techfak.uni-bielefeld.de/rnahybrid/). | |
| To characterize whether these miRNAs functionally interact with the 3’UTR of F3 we performed dual luciferase reporter assays | |
| Co-transfection of HMEC-1 with the miTargetTM miRNA 3’UTR target clone pEZX-MT01, containing the 3’UTR of F3 (3’UTR F3), and the miR-19a hairpin inhibitor (anti-miR-19a) significantly increased the luciferase activity in HMEC-1 after 24 h, compared to cells treated with a non-inhibitory negative control (anti-miR-control; Figure 3A). Co-Transfection of HMEC-1 with a negative control vector (3’UTR control) and anti-miR-19a or antimiR- control, respectively, had no impact on the luciferase activity. Treatment of cells with anti-miR-126 led to comparable results (Figure 3B). Compared to controls, co-transfection of endothelial cells with the 3’UTR of F3-containing vector and the miR-126 hairpin inhibitor (anti-miR-126) increased the luciferase activity in these cells post 24 h. | |
| Figure 3: Binding analyses of miR-19a and miR-126 to the 3’UTR of F3. Depicted are the results of the dual luciferase reporter assay. In (A) the influence of the miR-19a hairpin inhibitor (anti-miR-19a) on the relative luciferase activity of the miTargetTM miRNA 3’UTR target clone pEZXMT01, containing the 3’UTR of F3 (3’UTR F3) is shown in HMEC-1 24 h post transfection. As controls, cells were co-transfected with a negative control vector (3’UTR control) and anti-miR-19a or a non-inhibitory negative hairpin miRNA (anti-miR-control), respectively. In (B) the impact of the miR- 126 hairpin inhibitor (anti-miR-126) on the luciferase activity was analyzed in analogous experimental settings. Renilla luciferase activity was normalized to firefly luciferase activity. (*) p<0.05; (n.s.) no significant difference compared to control; n=4. | |
| The effect of miR-19a and miR-126 inhibition of the TF isoform mRNA expression | |
| To characterize the impact of miR-19a and miR-126 on the TF isoform expression in endothelial cells, HMEC-1 was transfected with hairpin inhibitors against miR-19a or miR-126, respectively. The impact of these inhibitors was analyzed in resting as well as in TNF-α- stimulated HMEC-1 (Figure 4). Transfection of these cells with anti-miR-19a or anti-miR-126, respectively, significantly increased the mRNA expression of flTF (Figure 4A) as well as of asTF (Figure 4B). In TNF-α-treated HMEC-1 inhibition of miR-19a as well as of miR- 126 also increased the expression of both; flTF (Figure 4C) and as TF (Figure 4D). The impact of anti-miR-19a on the mRNA expression of both TF isoforms in resting as well as in pro-inflammatory stimulated HMEC-1 was more intensive than that of anti-miR-126 (Figure 4A, D). | |
| Figure 4: The impact of miR-19a and miR-126 on the TF isoform expression. Shown is the mRNA expression of (A) flTF and (B) asTF in resting HMEC as well as (C) flTF and (D) asTF in TNF-7α-stimulated cells, normalized against GAPDH. The expression is depicted as x-fold induction. Compared are non-stimulated cells (A, B) and HMEC-1 stimulated for 2 h with 10 ng/mL TNF-α (C, D). Controls were transfected for 24 h with a non-inhibitory negative hairpin miRNA (black bar). These controls were compared to HMEC- 1 transfected for 24 with hairpin inhibitors against miR-19a (anti-miR-19a, white bar) or miR-126 (anti-miR-126, grey bar). (#) p<0.01; (*) p<0.05; n≥3. | |
| MiRNA-mediated modulation of the protein expression and activity of TF | |
| We next studied the influence of hairpin inhibitors against miR-19a or miR-126, respectively, on the endothelial TF isoform expression on protein level. The impact of these inhibitors (anti-miR- 19a and anti-miR-126) was determined in resting cells (Figure 5) as well as in TNF-α-stimulated HMEC-1 (Figure 6). | |
| Figure 5: Modulation of the TF protein expression and TF activity in resting HMEC-1. Analysed were the protein expression of flTF (A) and asTF (B) as well as the TF activity (C) in resting HMEC-1. Controls were transfected for 24 h with a non-inhibitory negative hairpin miRNA (black bar) and compared to HMEC-1 transfected with hairpin inhibitors against miR-19a (anti-miR-19a, white bar) or miR-126 (anti-miR-126, grey bar), respectively. In (A) and (B) the relative change of the protein expression normalized against GAPDH was shown. In (C) the results were presented as x-fold induction of the cellular TF activity in 1 x 106 HMEC-1. (*) p<0.05; (i.t.) p<0.15 (in trend) compared to controls; (n.s.) no significant difference compared to control; (A, B) n≥3; (C) n≥5. | |
| Figure 6: Alteration of the protein expression and activity of TF in TNF- a-treated HMEC-1. Depicted is the protein expression of flTF (A) and asTF (B) as well as the TF activity (C) in HMEC-1 stimulated for 8 h with 10 ng/ mL TNF-a. Controls were transfected for 24 h with a non-inhibitory negative hairpin miRNA (black bar) and compared to HMEC-1 transfected with hairpin inhibitors against miR-19a (anti-miR-19a, white bar) or miR-126 (anti-miR-126, grey bar), respectively. (A, B) Shown is the relative modulation of the protein expression normalized against GAPDH. In (C) the results were depicted as relative induction of the cellular TF activity in 1 x 106 HMEC-1. (§) p<0.0001; (#) p<0.01; (*) p<0.05; (n.s.) no significant difference compared to control; (A, B) n=3; (C) n=5. | |
| Under normal conditions transfection of HMEC-1 with hairpin inhibitors against miR-19a or miR-126, respectively, slightly induced the flTF protein expression compared to controls (Figure 5A). The expression of asTF was significantly increased by anti-miR-19a, but not by transfection of resting HMEC-1 with anti-miR-126 (Figure 5B). Since flTF is the main-trigger of pro-thrombogenic activity we next characterized the influence of anti-miR-19a and anti-miR-126 on the cellular TF activity in resting HMEC-1 (Figure 5C). Compared to control cells, transfection of HMEC-1 with anti-miR-19a or antimiR- 126, respectively, significantly increased the cellular TF activity under normal conditions (Figure 5C) corresponding to the increased flTF expression in these cells (Figure 5A). | |
| Under pro-inflammatory conditions transfection of HMEC- 1 with anti-miR-19a or anti-miR-126, respectively, significantly increased the protein expression of flTF (Figure 6A) as well as of asTF (Figure 6B) 8 h post TNF-α stimulation. In TNF-α-induced HMEC-1 the TF activity was also elevated post pre-treatment of cells with antimiR- 19a or anti-miR-126, compared to TNF-α-stimulated controls (Figure 6C). | |
Discussion |
|
| Our results demonstrate that human MiRNAs MiR-19a and miR- 126 are involved in the TF isoform expression regulation in resting as well as in inflammatory-stimulated human microvascular endothelial cells. Furthermore, the modulation of the TF isoform expression directly affected the flTF-mediated cellular thrombogenicity of endothelial cells under normal as well as under inflammatory conditions. Our data further suggest that these effects were mediated via binding of miR-19a and miR-126 to the 3’UTR of the TF gene (F3). Therefore, we show for the first time that TF expression and activity is modulated on the post-transcriptional level via miR-19a and miR-126 in human endothelial cells. | |
| The Impact of inflammation on the expression of miR-19a and miR-126 in HMEC1 | |
| Endothelial cells control the vascular wall homeostasis as well as the blood thrombogenicity [1,3]. Inflammatory conditions, as mediated by TNF-α switch the endothelial phenotype from an anti- toward a pro-thrombogenic [4-6]. Inflammatory conditions were also known to alter the regulatory impact of miRNA in several experimental settings [17,27,28]. Here, we found that TNF-α treatment reduced the expression of miR-19a and miR-126. This is in line with the results of other groups [19-21]. These groups demonstrated that miR-126 as well as miR-19a plays important regulatory roles in inflammation [19-21]. Moreover, Zhang et al. showed that miR-19 directly regulated the TF expression in breast cancer cells [23]. Therefore, we set out to characterize the influence of miR-19a and miR-126 on TF isoform expression regulation in resting as well as in pro-inflammatory-activated endothelial cells. | |
| The Effect of miR-19a and miR-126 on the Endothelial TF Isoform Expression | |
| Zhang et al, found miR-19 to regulated the TF expression in breast cancer cells via directly binding to the 3’UTR of the TF gene F3 [23]. In line with these data, we found that treatment of HMEC-1 with hairpin inhibitors of miR-19a led to an increased luciferase activity in HMEC-1 by blocking of endogenous miR-19a. Moreover, we showed inhibition of miR-126 also to induce the luciferase activity in these cells. This indicated a negative regulatory role of both, miR-19a and miR-126 on the 3’UTR of F3 in endothelial cells. This is substantiated by the results of Teruel et al. indicating that other miRNA, such as different members of the miR-17-92 cluster could also be modulators of TF expression [22]. | |
| Expression analyses of asTF and flTF validated that miR19a and miR-126 affect the expression of these TF isoforms on mRNA as well as on protein level. We found inhibition of these miRNAs to induce the expression of asTF as well as of flTF in resting HMEC-1. In line with these data, treatment of MDA-MB-231 breast cancer cells with miR-19 mimics was demonstrated to suppress the expression of total TF [23]. The effect of the hairpin inhibitors on the luciferase expression was lower than on the impact on the expression of as TF and flTF. This may be due to the differences in experimental setting of the luciferase assay. In this assay, cells were first transfected with the expression plasmid. After 24 h an additional transfection was performed using the hairpin inhibitors. For TF isoform expression analyses the cells were transfected only with the inhibitors. This additional stress could affect the outcome of the luciferase assay. | |
| MiR-19a and mir-126 Modulate the TF-Mediated Thrombogenicity in HMEC-1 | |
| Since endothelial cells play an important role in the regulation of blood thrombogenicity, we focused on the impact of miR-19a and miR-126 on the endothelial pro-thrombogenic TF activity [3]. FlTF is the main trigger of cellular thrombogenicity [9]. And it is well accepted that an increased level of flTF leads to increased thrombogenicity [6,9,10,29,30]. As mentioned above, blocking of miR-19a as well as of miR-126 increased the expression of pro-thrombogenic flTF in microvascular endothelial cells. This was associated with an increased TF activity. This is in line with the results of other groups which showed miR-19 to downregulate the TF expression [22,23]. Moreover, Teruel et al. showed that in patients with systemic lupus erythematosus or antiphospholipid syndrome the reduced expression of miR-19 was associated with an increased TF-mediated thrombotic risk [22]. | |
Conclusions |
|
| In conclusion, our observations are unique in that they provide valuable new information about the regulatory network of miRNAs in human endothelial cells. This study points to miR-19a and miR- 126 to be - at least in parts - involved in the TF isoform expression regulation on post-transcriptional level in resting as well as in TNF-α- induced human microvascular endothelial cells. Our findings indicate that miRNA-mediated modulation of the TF isoform expression may be involved in the regulation endothelial TF activity, which is of immense importance for the regulation of blood thrombogenicity under (patho-) physiologic conditions. | |
Acknowledgment |
|
| This work was supported by grants from the Deutsche Forschungsgemeinschaft (DFG) (GRK 865; SFB-TR19). | |
References |
|
|
|