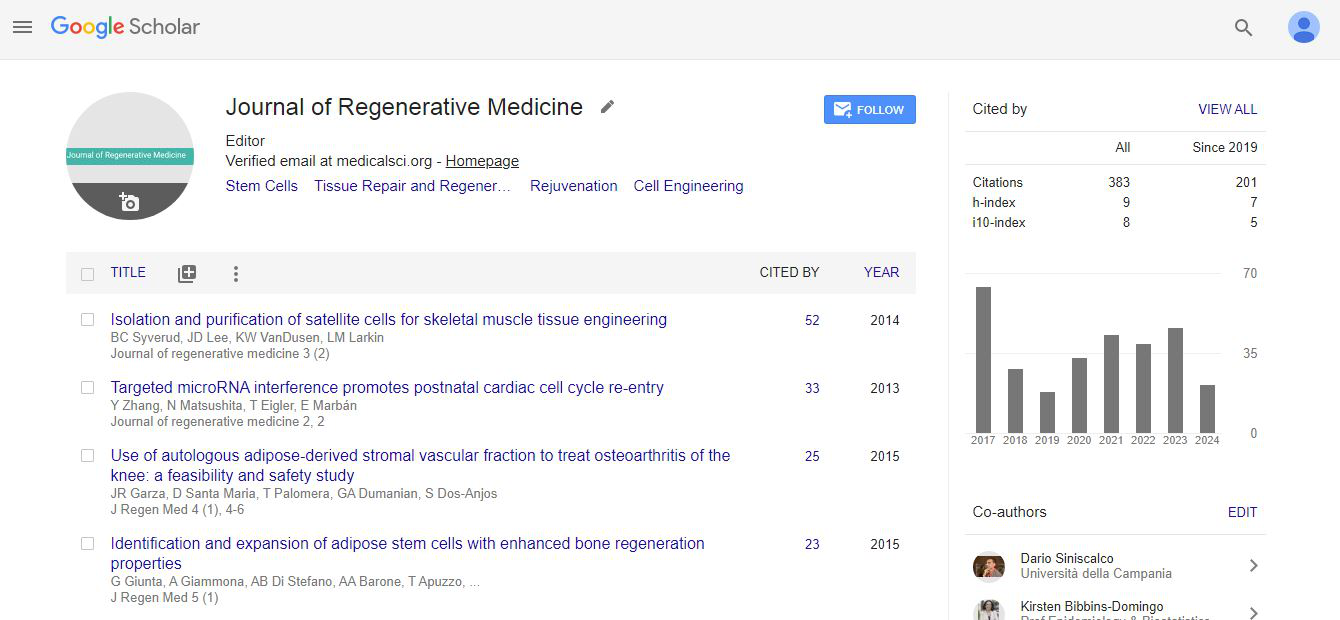
Commentary, J Regen Med Vol: 2 Issue: 1
Stem Cell Therapy for Diabetes: A Call for Efficient Differentiation of Pancreatic Progenitors
| Lina Sui1, Jing Qu1, Fei Yi2* and Guang-Hui Liu1* | |
| 1National Laboratory of Biomacromolecules, Institute of Biophysics, Chinese Academy of Sciences, Beijing 100101, China | |
| 2Department of Molecular and Cellular Physiology, Stanford University School of Medicine, 265 Campus Drive, Stanford, California 94305, USA | |
| Corresponding authors : Guang-Hui Liu National Laboratory of Biomacromolecules, Institute of Biophysics, Chinese Academy of Sciences, Beijing 100101, China, E-mail: ghliu@ibp.ac.cn Fei Yi Department of Molecular and Cellular Physiology, Stanford University School of Medicine, 265 Campus Drive, Stanford, California 94305, USA E-mail: fyi@stanford.edu |
|
| Received: February 02, 2013 Accepted: March 06, 2013 Published: March 10, 2013 | |
| Citation: Sui L, Qu J, Yi F, Liu GH (2013) Stem Cell Therapy for Diabetes: A Call for Efficient Differentiation of Pancreatic Progenitors. J Regen Med 2:1. doi:10.4172/2325-9620.1000104 |
Abstract
Stem Cell Therapy for Diabetes: A Call for Efficient Differentiation of Pancreatic Progenitors
Given the capacity of differentiating into functional beta cells in vivo, transplantation of pancreatic progenitors derived from human embryonic stem cells (hESCs) has been considered as a promising avenue in beta cell replacement therapy . Besides the concerns of preventing teratoma formation, reducing host immune system rejection and other related safety issues , generating sufficient number of pancreatic progenitors is one of the priorities before any consideration of clinical application.
Keywords: hESCs; Pancreatic progenitors; Small molecules; Cell therapy
Keywords |
|
| hESCs; Pancreatic progenitors; Small molecules; Cell therapy | |
Abbreviations |
|
| BIO: 6-Bromoindirubin-3’-oxime; BMP: Bone Morphogenetic Protein; CHIR: a Specific Inhibitor of Glycogen Synthase Kinase 3, CHIR 99021; CpdC: Dorsomorphin; FGF: Fibroblast Growth Factor; GSK3b: Glycogen Synthase Kinase 3 Beta; hESCs: Human Embryonic Stem Cells; IDE1/2: Inducer of Definitive Endoderm 1/2; ILV: (-) Indolactam V; PKC: Protein Kinase C; RA: All-trans Retinoic Acid; SB: SB431542; SHH: Sonic-hedgehog; TGF beta: Transforming Growth Factor Beta; WNT: Wingless-type MMTV Integration Site Family | |
| Given the capacity of differentiating into functional beta cells in vivo, transplantation of pancreatic progenitors derived from human embryonic stem cells (hESCs) has been considered as a promising avenue in beta cell replacement therapy [1,2]. Besides the concerns of preventing teratoma formation, reducing host immune system rejection and other related safety issues [3], generating sufficient number of pancreatic progenitors is one of the priorities before any consideration of clinical application. Recently, studies focusing on the scalable production of hESCs and definitive endoderm have been developed in order to enlarge the population of further derived pancreatic progenitors [4,5]. On the other hand, differentiation of pancreatic progenitors from hESCs in a both standard and efficient manner is fundamental to any clinical purpose. | |
| Directing hESCs towards pancreatic cells in culture is a multisteps procedure mimicking the key events of pancreatic development in vivo, which sequentially includes stages of definitive endoderm, pancreatic progenitor, endocrine progenitor and mature beta cell. Definitive endoderm differentiation of hESCs has been well studied and efficiently achieved [6-8]. However, an efficient process for generating pancreatic progenitors and functional beta cells has not yet been well described (Table 1). In mice, pancreatic progenitors are characterized by the co-expressions of Foxa2, Hnf6, Hlxb9, Sox9, Pdx1, Ptf1a, Nkx6.1 and Nkx2.2 during pancreas organogenesis [9-12]. Foxa2, Hnf6, Hlxb9 and Sox9 are widely expressed in the gut tube following definitive endoderm formation and are maintained in the pancreatic endoderm. Pdx1 is expressed robustly after pancreas specification and Ptf1a and Nkx6.1 expression are recruited later in Pdx1 positive populations. The cells co-expressing Pdx1, Nkx6.1 and Ptf1a are usually defined as pancreatic progenitors [13]. Assessing the cells that co-express these makers in hESC derivatives can be a reliable readout for evaluating the efficacy of pancreatic differentiation. However, most research groups selectively focus on beta cell induction at the final stage without evaluating the efficiency of obtaining pancreatic progenitors during differentiation [1,7,14-17]. A few investigators assessed this issue, but only quantified the number of PDX1 positive cells without evaluating the number of cells co-expressing this transcription factor with other progenitor markers. These evaluations are insufficient to indicate a genuine pancreatic progenitor population since PDX1 is also broadly expressed in other tissues such as posterior stomach and small intestine. To date, a maximum of 98% PDX1 and 86% NKX6.1 positive cells were derived from one of the most commonly used H1 ESC line by directly exposing DE cells to KGF in the presence of fetal serum, followed by inhibition of BMP4 and TGF beta pathways and activation of PKC pathway [18]. However, they did not assess the expression of PTF1a, which is indispensable for defining pancreatic progenitors (Table 1). Some groups who investigated the expressions of NKX6.1 and PTF1a together with PDX1 at transcriptional levels failed to provide decisive evidence of fully specified pancreatic progenitor derivation at a certain stage by showing PDX1, NKX6.1 and PTF1a triple positive cells [16,19-21]. It is not sufficient to specify pancreatic progenitors only based on mRNA levels without showing the co-expression of these transcription factors in the same cell. Additionally, some papers that clearly defined the number of PDX1 and NKX6.1 positive cells showed a limited number of co-expressing cells [12,22]. All of these suggest that extra signals might be required for a full specification of pancreatic progenitors. Finally, a systematic comparison of hESC-derived pancreatic progenitors with bona fide fetal pancreatic counterparts, as proof of concept, should also be done. | |
| Table 1: An overview of representative protocols for pancreas differentiation in vitro. | |
| A few trophic growth factors required for definitive endoderm and pancreas development in vivo are implemented in the in vitro pancreatic differentiation studies. Nodal and Wnt are key signaling pathways regulating definitive endoderm differentiation; moreover, BMP4, FGF, SHH and RA signalings are employed mainly with the intention of making pancreatic progenitor cells [9,11]. However, the potencies of recombinant proteins used for manipulating these pathways often vary from batch to batch and demonstrate instability in cell culture. This disadvantage of applying recombinant proteins can be effectively overcome by using small molecules. The SMAD2/3 pathway activators IDE1/2 and the GSK3b pathway inhibitors BIO and CHIR have been widely used as substitutes for Activin A and Wnt3a respectively. The combination of these small molecules allowed for efficient induction of definitive endoderm from hESCs [23-25]. Small molecules are also applied in the pancreatic and endocrine progenitor induction. For example, BMP4 inhibitor dorsomorphin (CpdC) was used to block liver commitment from definitive endoderm, and TGF beta-receptor inhibitor SB431542 (SB) and the protein kinase C (PKC) pathway activator (-) indolactam V (ILV) were exploited for efficient induction of pancreatic progenitors [16,24,26,27] (Figure 1). It is foreseeable that the general use of such chemical approaches would effectively help to diminish the financial and biological hurdles associated with recombinant proteins for manipulating signaling pathways in the future. Although, like growth factors, we still don’t know the full range of biological effects and interactions of small molecules. | |
| Figure 1: An image of the signaling pathways involved in the process of pancreatic differentiation from hESCs. The growth factors and the related small molecule substitutes regulating these pathways are listed. Green arrow: activation; Red arrow: inhibition. | |
| In summary, efficient generation of pancreatic progenitors from hESCs provides an exciting promise for beta cell replacement therapy. To date, although a high percentage of PDX1 positive cells could be obtained in culture [22], a convincing evidence of generating fully specified pancreatic progenitors is still missing. Additionally, only a limited number of insulin positive cells can be derived from hESCs at the terminal stage of differentiation, and most of them failed to demonstrate the glucose responsiveness. The failure to generate functional beta cells by hESCs differentiation in vitro suggests that certain signals or factors crucial for this process are still lacking. It is possible that a precise regulation of specific signaling pathways and epigenetic features using small molecules may eventually lead to an efficient and standard protocol of generating pancreatic progenitors and completely mature and functional beta cells from hESCs. Finally, cell surface marker based methods are promising for a specific selection and enrichment of such pancreatic progenitor and mature beta cell population [28]. | |
Competing Interests |
|
| The authors indicate no potential conflicts of interest. | |
Acknowledgements |
|
| GHL is supported by the Thousand Young Talents program of China, the National Laboratory of Biomacromolecules, the Strategic Priority Research Program of the Chinese Academy of Sciences (XDA01020312), and NSFC (81271266, 31222039, 31201111). | |
References |
|
|
|