Review Article, J Aging Geriatr Med Vol: 1 Issue: 2
A Life Course Approach to Dementia Prevention
Dorina Cadar*
Research Department of Behavioural Sciences and Health, University College London, London, UK
*Corresponding Author : Dorina Cadar
Research Associate in Dementia, Department of Behavioural Health Sciences, University College London, Torrington Place, London, UK
Tel: 02076795969
E-mail: d.cadar@ucl.ac.uk
Received: February 27, 2017 Accepted: April 17, 2017 Published: April 24, 2017
Citation: Cadar D (2017) A Life Course Approach to Dementia Prevention. J Aging Geriatr Med 1:2.
Abstract
Across the world, there is an unprecedented growth in the number of older people, with clear implications for the prevalence of cognitive decline and dementia. This review discusses the global burden of dementia on individuals and societies around the world, as well as the risk factors associated with dementia and cognitive impairment from a life course approach. Dementia and Mild Cognitive Impairment are etiologically discussed with a particular focus on the role of modifiable lifestyle behaviors and their biological mechanisms. The early life period is likely to be the most critical for the development of cognitive reserve (learning, and education); the midlife period is particularly sensitive to lifestyle behaviors, environmental exposures, head trauma or depression, while the later stage of life period seems to be more sensitive to the role of social support and networks, physical activities or hormone therapy. Some factors may overlap between these standard periods. For example, the development and control of vascular and metabolic risk factors have been shown to be particularly influential in middle life (the 40s to 60s), whereas mental and physical activity patterns may continue to moderate the risk of dementia from mid into later life. Interventions targeting healthy lifestyle (e.g. exercise, diet, nonsmoking, moderate drinking and social participation) may lead to robust effects throughout later life and could offer an increase in life expectancy and a lower risk of dementia.
Keywords: Dementia; Mild cognitive impairment; Risk factors; Lifestyle behaviors; Biological mechanisms; Life course approach
Introduction
An important determinant of quality of life is the optimal function of physical and mental health. Highly complex measurements can assess mental capabilities within specific cognitive tasks, such as memory, processing speed, attention, language, reasoning and problem-solving. These cognitive abilities tend to decline as part of normal aging [1]. However, the amount of cognitive decline varies considerably depending on the level of education [2], genetic influence [3], social class and early environment [4], lifestyle behaviors such as alcohol consumption [5], fruit and vegetables intake [6], cigarette smoking [7] and low exercise (both physical and mental) [8,9]. Severe cognitive decline is not inevitable, but remains one of the greatest concerns in present-day aging societies, as the cognitive decline is an important predictor for the development of dementias [10,11]. With people living longer than ever before, developing realistic strategies to reduce cognitive decline and thereby prevent dementia has been regarded as a high priority by governments around the world [12].
Across the world, there is an unprecedented growth in the number of older people, with clear implications for the prevalence of cognitive decline and dementia. It is estimated that by 2050 over two billion people (30% of the total population) will be over 65, and there is a high probability that they will be exhibiting the most common motor and cognitive behavioral changes that occur with aging [13]. Along with the increase in the number of older people in the population, life expectancy has also been continuously increasing in the last few decades.
With an accompanying continuous decline in mortality and fertility rates, the aging of the population has now become a worldwide phenomenon, and this shift is no longer restricted to high-income countries [14].
Dementia: a public health issue
Associated with older age, pathologies such as dementia have become leading public health concerns of modern populations. A consequence of the increase in lifespan is that in 20 years time there will be nearly twice as many people with dementia in the world as there is today.
The term "dementia" refers to a group of neurodegenerative diseases that are characterized by a progressive decline in multiple cognitive functions, resulting in impaired daily activities [15]. People with dementia suffer from amnesia (loss of memory), aphasia (language impairment), apraxia (impaired ability to carry out motor activities despite normal motor function), agnosia (failure to recognize or identify objects despite intact sensory function) or decreased reasoning ability. A distinction has often been made between two groups of dementias: primary degenerative dementia (e.g. Alzheimer's disease) and secondary dementia (e.g. vascular dementia), which is caused by the development of another illness [16]. However, the distinction between degenerative and vascular dementia has been breaking down to some extent, as there is evidence to suggest that the latter contributes to the etiology of the former [17]. Rare forms of dementia can result from other causes, such as alcohol poisoning, brain tumor or human immunodeficiency virus (HIV) [15].
Research into dementia progression suggests the existence of a progressive decline in cognitive function before the actual diagnosis of dementia. Therefore, it is critical to study the subtle cognitive changes that seem to appear from early midlife [18-21] in order to detect people at risk of developing dementia. People with cognitive functioning lower than normal may be diagnosed with "Mild Cognitive Impairment" (MCI). This concept was first proposed by Petersen, as a nosologic entity referring to elderly individuals with the mild cognitive deficit, but without dementia. Even if the clinical criteria for the diagnosis of MCI is still evolving today, the terminology has become widely used and accepted by practicing clinicians.
Currently, the criteria for clinically probable AD identify people after a substantial degree of cognitive decline has occurred. According to many findings, up to 50% of individuals with MCI develop dementia within five years after diagnosis [23,24]. The prevalence of dementia is approximately 1.5% among those aged 65, and this seems to double every five years, to over 30% in people over 85 [25,15]. With the increasingly aging population, the number of older people affected by dementia may be rising in parallel. There are currently 24.3 million people with dementia in the world, with an estimated 4.6 million new cases every year. This is the equivalent to one new case every seven seconds. The number of older people affected by dementia is projected to double approximately every 20 years to 42.3 million in 2020 and 81.1 million by 2040 [21].
Impact and prevention
Cognitive impairment and dementia result in functional, psychological and financial problems. In cases of severe deficits in memory or motor function, hospitalization or residential care is a likely outcome, putting a financial burden on healthcare services. Reducing or preventing age-related decrements in the neuronal function will curb the otherwise exponentially rising healthcare costs. The human burden is enormous, not only for sufferers, family, and friends but also in economic terms to the state in general. Since cognitive decline frequently precedes dementia, it is important to understand what predicts cognitive decline and what could potentially prevent dementia. The application of preventive thinking with regard to dementia is relatively recent. Primary prevention has been centered on delaying clinical symptoms rather than on avoiding initial pathogenic events that can occur decades before the disease becomes expressed [26]. An increased focus on primary prevention is now on developing interventions to prevent the progression of neuropathology before irreversible damage is done. This, however, depends on early identification of people at risk. Primary prevention may depend on the initiation and maintenance of behavioral changes to delay cognitive decline, but research is essential to clarify its validity.
While descriptive epidemiology is useful in investigating the impact of dementia in a population, analytical epidemiological studies are important for the identification of disease risk factors. Risk factors can be divided into modifiable and non-modifiable ones. Those that are modifiable discriminate the obvious targets for preventive treatment or behavior modification, and some of these (alcohol use, smoking, physical activity and diet) could impact dementia risk independently and in combination. The non-modifiable risk factors are still important in understanding the pathogenesis of the disease. These include age, sex, family history and genetic factors. As demonstrated in the incidence and prevalence studies of dementia mentioned above, age was the most consistent risk factor across many studies [27,28]. The longer a person lives, the more time there is for plaque accumulation and the greater the likelihood that clinical dementia will occur. Also, the maturing brain is exposed to a lifetime of changes, and small insults such as oxidative stress, trauma, inflammation and white matter disease from small vessel ischemia may slowly accumulate over the years, eventually to become symptomatic.
A life course perspective
For a long time, "age" was considered in a purely chronological sense, disregarding essential pathways grounded on biological, psychological and social contributions. A life course approach underlines the need to study the long-term, complex interplay among genetic, biological and psychological mechanisms from birth. This approach encompasses evidence that adult functioning and age-related chronic diseases have their origins at different points in the life course, and share common risk factors across. Adult health and disease risk can be linked to physical or social exposures which occur during gestation, childhood, adolescence, adult life, or across generations [29]. With such models, lifestyle risk factors contributing to the development of chronic diseases are measured over the life course and are considered cumulatively.
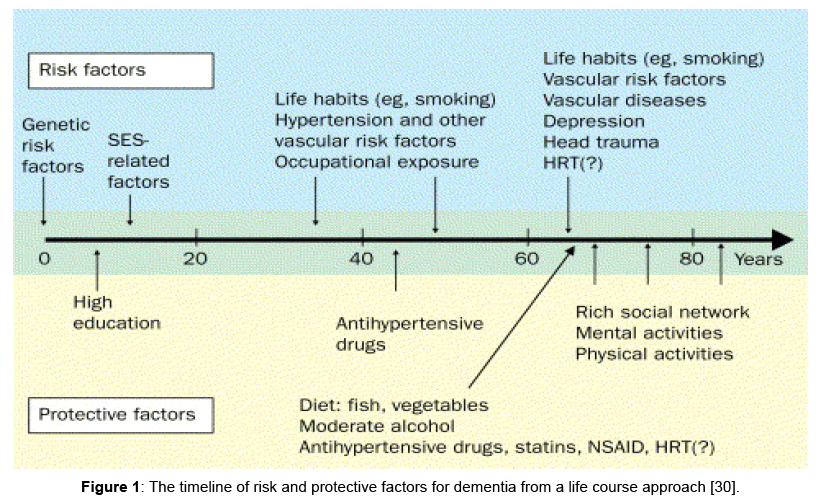
Risk and protective factors for cognitive decline and dementia can also exert their influence at different times in the life course. Life course epidemiology can examine the association between modifiable risk and protective factors, and address the hypothesis that an active and socially integrated lifestyle in later life may protect against AD. This can be incorporated into a general model of dementia occurrence, taking into account different risks and protective factors acting throughout the life course (Figure 1) [30]. Childhood cognitive ability and education correlate highly with cognitive ability in midlife and old age [31,32]. Learning during childhood is critical for the development of cognitive reserve [33], but this may also be a time when distal adverse influences contributing to the risk of dementia may first become active. The cognitive reserve hypothesis refers to a lifetime cognitive experience, influencing the number of neurons and synapses that survive into adult life [34-39]. The term defines the mind's resistance to the physiological damage to the brain, by engaging increased neural networks and hemispheric activation. Neural plasticity and repair mechanisms may support the lifelong accumulation of cognitive reserve.
Figure 1: The timeline of risk and protective factors for dementia from a life course approach [30].
Epidemiological and neuroimaging studies have proposed that to reach a given level of clinical severity of dementia, AD pathology must be more advanced in patients with higher educational and occupational attainment [40]. This is more likely because raised levels of cognitive reserve are believed to increase an individual's ability to mask AD pathology and prolong everyday functioning even where there was substantial neurodegeneration [35]. The amount of cognitive reserve is adaptable and is influenced by various preventive interventions. However, when should prevention begin? At which life stages are preventive interventions most effective? The best available answers come from longitudinal studies examining associations between different modifiable and protective risk factors for cognitive decline and dementia at various points across the life course.
From these studies, three key periods were acknowledged and suggested as to when the risk or protective factors were most likely to occur during the life course. The early life period is likely to be the most critical for the development of cognitive reserve (IQ, learning, and education) [41]. The midlife period is particularly sensitive to lifestyle behaviors, occupational exposures, head trauma and depression, while the later life period seems to be closely linked with social networks, physical activities, and hormone therapy. Some factors may overlap between these standard periods. For example, the development and control of vascular and metabolic risk factors have been shown to be particularly influential in middle life (the 40s to 60s), whereas mental and physical activity patterns may continue to moderate the risk of dementia from mid into later life [30]. There is also the possibility that certain factors such as lifestyle behaviors could occur across the whole life course (e.g. diet and various degrees of physical activity). A similar set of risk factors contributing to cardiovascular disease (hypertension, high cholesterol, diabetes) are associated with cognitive impairment and dementia, and there is a strong possibility that certain lifestyle behaviors could influence these (e.g. diet and various degrees of physical activity).
The role of lifestyle behaviors
The term "lifestyle behavior" refers to activities of daily living that affect health (e.g. smoking, use of alcohol, diet, and physical activity). Because of a direct link to health outcomes, the term "lifestyle behaviors" has also been referred to in the literature as "health-related behaviors." Many studies have shown that lifestyle behaviors are associated with cardiovascular disease, type 2 diabetes [42], coronary heart disease [43] and mortality [44].
Lifestyle factors showing a relatively consistent association with decreased risk of dementia and cognitive decline are cognitive engagement, social and physical activities. Direct influences such as increased cerebral blood flow related to physical activity, which in turn promotes nerve cell growth and enhanced cerebrovascular function, were most frequently cited in the in aging literature research. However, it is very likely that physical activity may also improve cognition through its effects on mediator variables such as depression, sleep, appetite (diet), and energy levels by postponing or preventing age-related diseases (e.g. diabetes, hypertension) known to affect cognition. In addition, there were also well-known benefits of non-smoking [45,46] moderate alcohol consumption [5,47] and healthy dietary choices [6,48] for cognitive functioning from mid to later life. However, less is known about the combined effects of these behaviors on cognitive decline and dementia.
In addition to considerable observational data of the independent effects of lifestyle factors, there is now increasing empirical evidence from intervention studies [49] that alterations in lifestyle factors may lessen an individual's risk of developing cognitive decline. These interventions carry few risks and have many additional health benefits, so they can be recommended for most of the older population. Other interventions such as increasing social engagement, cognitive stimulation and homocysteine-lowering vitamin supplements also appear promising, with considerable observational evidence supporting their uptake, although there is still a lack of empirical evidence for these interventions. Similarly, fitness training interventions were found to have robust but selective benefits for cognition, with the largest fitness-induced benefits occurring for executive control processes [50]. This indicates that cognitive and neural plasticity could be maintained throughout the lifespan. However, the real risk of dementia is probably underestimated, and it is not clear how many people quit smoking between the time of the initial survey and the onset of dementia, but there were clear longterm consequences of mid-life smoking.
Research has also shown that diet can help prevent, better manage or even reverse conditions such as hypertension, hyperlipidemia (high cholesterol), hyperglycemia (high blood sugar) and atherosclerosis that may lead to cardiovascular and cerebrovascular disease. This, in turn, affects optimal functioning of organs including the brain due to inefficient transfer of glucose and oxygen necessary for optimal neuronal transmission, with a significant impact on cognitive functioning.
Biological mechanisms
The proposed biological mechanisms underpinning the role of lifestyle behaviors on the cognitive functioning are shared among several lifestyle behaviors such as alcohol consumption, smoking, physical activity and diet (mainly discussed in this review). There are at least five pathways identified. Firstly, cardiovascular risk factors have been associated with cognitive impairment and dementia [51]. This association has been acknowledged by the saying "what's good for the heart is also good for the head" (Department of Health, 2009). The association may be through embolism or decreased cerebral perfusion [52].
One cardiovascular risk factor of interest is the amino acid homocysteine. Several studies have suggested that levels of homocysteine tend to increase with age and poor lifestyle (such as high alcohol consumption or smoking), and rise even further through vitamin B deficiency [53,54]. An excessively high blood level of homocysteine results in injuries of the inner lining of blood vessel walls [55], induces oxidative stress and increases blood clot formation, representing a powerful risk factor for cardiovascular disease [56,57], stroke and dementia [58]. This mechanism suggests that a healthier lifestyle will maintain low levels of homocysteine, which in turn could be protective against cardiovascular and dementia outcomes.
Secondly, inflammation is thought to be an underlying feature of the metabolic syndrome, and one of the mechanistic pathways directly linked to changes in functional biomarkers associated with the pathogenesis of cognitive decline, functional impairment, and associated neurodegenerative processes [59]. Unnecessary inflammation occurs due to an imbalance in the transfer of oxygen between cells through cell damage and oxidative stress. It has been suggested that flavonoids, present in colorful fruit and vegetables but also in wine, protect the brain from chronic inflammation, and thus protect cognitive performance [60,61].
Thirdly, neurotransmission processes are altered. Moderate amounts of alcohol may stimulate the release of the neurotransmitter acetylcholine in the hippocampus, whereas memory impairment from chronic and heavy alcohol consumption parallels a reduction in cholinergic neurotransmission [62,63]. Physical activity has also been associated with altering levels of serotonin [64] and dopamine [65], leading to improved plasticity and neuronal survival.
Fourthly, CNS white matter is affected. There is population-based evidence showing that moderate drinkers have fewer white matter abnormalities in later life than abstainers or heavy drinkers [66], thus raising the possibility of a neuro protective effect of moderate consumption. However, the beneficial effect of low to moderate alcohol intake on brain structures is still debated [67]. Smoking has also been linked to white matter loss caused by either cerebral small vessel disease or lacunar infarcts [68]. Furthermore, empirical evidence and theoretical supposition both suggest that physical activity modifies brain structures that are involved in age-related decline. Neuroimaging studies have shown changes in brain structure and function with regular exercise. Most changes have been linked to the prefrontal, frontal, and parietal cortices in older adults [69], including the hippocampus and neocortex. One of the reasons is that these areas exhibit some of the most striking types of cellular plasticity, such as neurogenesis and synaptogenesis. Evidence also suggests a positive association of leisure-time physical activity with greater intensity of activation in the left caudate volume in patients diagnosed with amnestic MCI or affected by AD pathology [70,71]. Physical activity has also been linked with increased neurogenesis – the development of new brain cells – in the dentate gyrus of the hippocampus.
Fifthly, oxidative stress is an intrinsic part of the neurodegeneration process. Oxidative damage has been implicated in the pathogenesis of Alzheimer's disease and neuronal death. Evidence suggests that an extended period of gradual oxidative damage accumulation precedes the clinical and pathological symptoms of dementia, including amyloid (Aβ) deposition, neurofibrillary tangle formation, metabolic dysfunction and cognitive decline [72]. Increased evidence shows an association between the Mediterranean diet and lower levels of memory and thinking problems [73]. The typical Mediterranean Diet includes a high intake of plant-based food, which form a good source of antioxidants; whole grains, legumes, and nuts; while limiting intake of red meat and replacing butter with healthy fats, such as olive oil. The high levels of antioxidants from fruits and vegetables may help to protect against some of the damage to brain cells associated with dementia, as well as increasing the levels of proteins in the brain that protect brain cells from this damage. Alternative elements such as marijuana and cannabis oils are now considered as potential treatment options for Alzheimer’s disease. For example, tetrahydrocannabinol (THC) has been shown to lower the high levels of amyloid-beta and reduce the buildup of the plaques and tangles associated with the disease [74]. Recent evidence from a study on mice has shown that THC reverses the age-related decline in memory performance, which was attributed to the concomitant increase in hippocampal synaptic spine density [75]. This was in turn due to THC restoring hippocampal gene expression to the level seen in younger mice. These are potential new targets for treating and preventing dementia and Alzheimer’s disease if regulation permits.
Conclusions
Effective preventive measures represent key components of any response to the potentially overwhelming problem of dementia. Accumulating evidence points to the potential risk factors of cardiovascular disorders or dementia (e.g. midlife obesity and cigarette smoking) and the potential protective roles of psychosocial and lifestyle factors (e.g. higher education, regular exercise, healthy diet, intellectually challenging leisure activities, and an active socially integrated lifestyle). Optimal control and management of lifestyle factors have demonstrated efficacy in the prevention of cognitive decline and dementia, highlighting a close link between the risk factors for cardiovascular and cerebrovascular disease and dementia. Furthermore, the study of lifestyle behaviors across different periods of life demonstrates that the association with cognitive decline or dementia can also change depending on the time in life when these behaviors are measured or clustered with other cardiovascular risk factors. Interventions targeting healthy lifestyle (e.g. cognitive, exercise, diet, social networks, non-smoking and moderate drinking) may lead to robust effects throughout later life and could offer an increase in life expectancy and a lower risk of dementia. In conclusion, there is an important role of lifestyle behaviors in preventing dementia, that should start as early as midlife so the message should be simple “Use it, don't lose it!".
Acknowledgement
D. Cadar would like to thank Professor Marcus Richards (MRC Unit for Lifelong Health and Ageing at UCL, UK), Professor Gita Mishra (University of Queensland, Australia) and Dr Hynek Pikhart (UCL, UK) for their helpful suggestions during the preparation of this review.
Funding
D. Cadar is currently supported by the National Institute on Aging (NIA) (Grant 528122) and was previously funded by the UK Medical Research Council. The content is solely the responsibility of the author and does not necessarily represent the official views of the NIA or other funding bodies mentioned above.
References
- Schaie KW (1994) The course of adult intellectual development. Am Psychol 49: 304-313.
- Roe CM, Xiong C, Grant E, Miller JP, Morris JC (2008) Education and reported onset of symptoms among individuals with Alzheimer disease. Arch Neurol 65: 108-111.
- Yaffe K (2010) Biomarkers of Alzheimer's disease and exercise: one step closer to prevention. Ann Neurol 68: 275-276.
- Richards M, Wadsworth ME (2004) Long term effects of early adversity on cognitive function. Arch Dis Child 89: 922-927.
- Espeland MA, Gu L, Masaki KH, Langer RD, Coker LH, et al. (2005) Association between reported alcohol intake and cognition: results from the Women's Health Initiative Memory Study. Am J Epidemiol 161: 228-238.
- Morris MC, Evans DA, Tangney CC, Bienias JL, Wilson RS (2006) Associations of vegetable and fruit consumption with age-related cognitive change. Neurology 67: 1370-1376.
- Anstey KJ, von Sanden C, Salim A, O'Kearney R (2007) Smoking as a risk factor for dementia and cognitive decline: a meta-analysis of prospective studies. Am J Epidemiol 166: 367-378.
- Larson EB, Wang L, Bowen JD, McCormick WC, Teri L, et al. (2006) Exercise is associated with reduced risk for incident dementia among persons 65 years of age and older. Ann Intern Med 144: 73-81.
- Salthouse TA (2006) Mental Exercise and Mental Aging. Perspect Psychol Sci 1: 68-87.
- Almkvist O, Tallberg IM (2009) Cognitive decline from estimated premorbid status predicts neurodegeneration in Alzheimer's disease. Neuropsychology 23: 117-124.
- Bäckman L, Small BJ (2007) Cognitive deficits in preclinical Alzheimer's disease and vascular dementia: patterns of findings from the Kungsholmen Project. Physiol Behav 92: 80-86.
- Prince M, Bryce R, Albanese E, Wimo A, Ribeiro W, et al. (2013) The global prevalence of dementia: a systematic review and metaanalysis. Alzheimers Dement 9: 63-75.
- Christensen K, Doblhammer G, Rau R, Vaupel JW (2009) Ageing populations: the challenges ahead. Lancet 374: 1196-1208.
- Kinsella K (2000) Demographic dimensions of global aging. J Fam Issues 21: 541-558.
- Ritchie K, Lovestone S (2002) The dementias. Lancet 360: 1759-1766.
- Ritchie K (2004) Mild cognitive impairment: an epidemiological perspective. Dialogues Clin Neurosci 6: 401-408.
- Richards M, Brayne C (2010) What do we mean by Alzheimers disease? BMJ 341: c4670.
- Singh-Manoux A, Kivimaki M, Glymour MM, Elbaz A, Berr C, et al. (2012) Timing of onset of cognitive decline: results from Whitehall II prospective cohort study. BMJ 344: d7622.
- Amieva H, Le Goff M, Millet X, Orgogozo JM, Pérès K, et al. (2008) Prodromal Alzheimer's disease: successive emergence of the clinical symptoms. Ann Neurol 64: 492-498.
- Hachinski V (2008) Shifts in thinking about dementia. JAMA 300: 2172-2173.
- Brayne C (2007) The elephant in the room - healthy brains in later life, epidemiology and public health. Nat Rev Neurosci 8: 233-239.
- Petersen RC (2000) Mild cognitive impairment: transition between aging and Alzheimer's disease. Neurologia 15: 93-101.
- Brookmeyer R, Johnson E, Ziegler-Graham K, Arrighi HM (2007) Forecasting the global burden of Alzheimer's disease. Alzheimers Dement 3: 186-191.
- Chertkow H, Massoud F, Nasreddine Z, Belleville S, Joanette Y, et al. (2008) Diagnosis and treatment of dementia: 3. Mild cognitive impairment and cognitive impairment without dementia. CMAJ 178: 1273-1285.
- Ferri CP, Prince M, Brayne C, Brodaty H, Fratiglioni L, et al. (2005) Global prevalence of dementia: a Delphi consensus study. Lancet 366: 2112-2117.
- Braak H, Braak E (1991) Neuropathological stageing of Alzheimer-related changes. Acta Neuropathol 82: 239-259.
- Fitzpatrick AL, Kuller LH, Ives DG, Lopez OL, Jagust W, et al. (2004) Incidence and prevalence of dementia in the Cardiovascular Health Study. J Am Geriatr Soc 52: 195-204.
- Fratiglioni L, Launer LJ, Andersen K, Breteler MM, Copeland JR, et al. (2000) Incidence of dementia and major subtypes in Europe: A collaborative study of population-based cohorts. Neurologic Diseases in the Elderly Research Group. Neurology 54: S10-S15.
- Ben-Shlomo Y, Kuh D (2002) A life course approach to chronic disease epidemiology: conceptual models, empirical challenges and interdisciplinary perspectives. Int J Epidemiol 31: 285-293.
- Fratiglioni L, Paillard-Borg S, Winblad B (2004) An active and socially integrated lifestyle in late life might protect against dementia. Lancet Neurol 3 343-353.
- Deary IJ, Corley J, Gow AJ, Harris SE, Houlihan LM, et al. (2009) Age-associated cognitive decline. Br Med Bull 92: 135-152.
- Richards M, Black S, Mishra G, Gale CR, Deary IJ, et al. (2009) IQ in childhood and the metabolic syndrome in middle age: Extended follow-up of the 1946 British Birth Cohort Study. Intelligence 37: 567-572.
- Richards M, Deary IJ (2005) A life course approach to cognitive reserve: A model for cognitive aging and development?. Ann Neurol 58: 617-622.
- Fratiglioni L, Wang HX (2007) Brain reserve hypothesis in dementia. J Alzheimers Dis 12: 11-22.
- Stern Y (2002) What is cognitive reserve? Theory and research application of the reserve concept. J Int Neuropsychol Soc 8: 448-460.
- Stern Y (2009) Cognitive reserve. Neuropsychologia 47: 2015-2028.
- Stern Y (2009) Cognitive reserve: a catalyst for research. J Neurol Sci 283: 256.
- Stern Y (2012) Cognitive reserve in ageing and Alzheimer's disease. Lancet Neurol 11: 1006-1012.
- Whalley LJ, Deary IJ, Appleton CL, Starr JM (2004) Cognitive reserve and the neurobiology of cognitive aging. Ageing Res Rev 3: 369-382.
- Nithianantharajah J, Hannan AJ (2009) The neurobiology of brain and cognitive reserve: mental and physical activity as modulators of brain disorders. Prog Neurobiol 89: 369-382.
- Borenstein AR, Copenhaver CI, Mortimer JA (2006) Early-life risk factors for Alzheimer disease. Alzheimer Dis Assoc Disord 20: 63-72.
- Schulze MB, Hu FB (2002) Dietary patterns and risk of hypertension, type 2 diabetes mellitus, and coronary heart disease. Curr Atheroscler Rep 4: 462-467.
- Chiuve SE, McCullough ML, Sacks FM, Rimm EB (2006) Healthy lifestyle factors in the primary prevention of coronary heart disease among men: benefits among users and nonusers of lipid-lowering and antihypertensive medications. Circulation 114: 160-167.
- van Dam RM, Li T, Spiegelman D, Franco OH, Hu FB (2008) Combined impact of lifestyle factors on mortality: prospective cohort study in US women. BMJ 337: a1440.
- Cadar D, Pikhart H, Mishra G, Stephen A, Kuh D, et al. (2012) The role of lifestyle behaviors on 20-year cognitive decline. J Aging Res 2012: 304014.
- Sabia S, Nabi H, Kivimaki M, Shipley MJ, Marmot MG, et al. (2009) Health behaviors from early to late midlife as predictors of cognitive function: The Whitehall II study. Am J Epidemiol 170: 428-437.
- Ganguli M, Vander Bilt J, Saxton JA, Shen C, Dodge HH (2005) Alcohol consumption and cognitive function in late life - A longitudinal community study. Neurology 65: 1210-1217.
- Kang JH, Ascherio A, Grodstein F (2005) Fruit and vegetable consumption and cognitive decline in aging women. Ann Neurol 57: 713-720.
- Flicker L (2009) Life style interventions to reduce the risk of dementia. Maturitas 63: 319-322.
- Colcombe SJ, Erickson KI, Raz N, Webb AG, Cohen NJ, et al. (2003) Aerobic fitness reduces brain tissue loss in aging humans. J Gerontol A Biol Sci Med Sci 58: 176-180.
- Breteler MM (2000) Vascular involvement in cognitive decline and dementia. Epidemiologic evidence from the Rotterdam Study and the Rotterdam Scan Study. Ann N Y Acad Sci 903: 457-465.
- Pullicino PM, Hart J (2001) Cognitive impairment in congestive heart failure?: Embolism vs hypoperfusion. Neurology 57: 1945-1946.
- Herrmann W, Obeid R (2011) Homocysteine: a biomarker in neurodegenerative diseases. Clin Chem Lab Med 49: 435-441.
- Clarke R, Halsey J, Bennett D, Lewington S (2011) Homocysteine and vascular disease: review of published results of the homocysteine-lowering trials. J Inherit Metab Dis 34: 83-91.
- Schnyder G, Roffi M, Pin R, Flammer Y, Lange H, et al. (2001) Decreased Rate of Coronary Restenosis after Lowering of Plasma Homocysteine Levels. N Engl J Med 345: 1593-1600.
- Ruijter W, Westendorp RG, Assendelft WJ, den Elzen WP, de Craen AJ, le CS, et al. (2009) Use of Framingham risk score and new biomarkers to predict cardiovascular mortality in older people: population based observational cohort study. BMJ 338: a3083.
- Lonn E, Yusuf S, Arnold MJ, Sheridan P, Pogue J, et al. (2006) Homocysteine lowering with folic acid and B vitamins in vascular disease. N Engl J Med 354: 1567-1577.
- Van Dam F, Van Gool WA (2005) Hyperhomocysteinemia and Alzheimer's disease: A systematic review. Arch Gerontol Geriatr 48: 425-430.
- Ershler WB (2007) A gripping reality: oxidative stress, inflammation, and the pathway to frailty. J Appl Physiol 103: 3-5.
- Peneau S, Galan P, Jeandel C, Ferry M, Andreeva V, et al. (2011) Fruit and vegetable intake and cognitive function in the SU.VI.MAX 2 prospective study. Am J Clin Nutr 94: 1295-1303.
- Nurk E, Refsum H, Tell GS, Engedal K, Vollset SE, et al. (2005) Plasma total homocysteine and memory in the elderly: The Hordaland Homocysteine study. Ann Neurol 58: 847-857.
- Fadda F, Rossetti ZL (1998) Chronic ethanol consumption: from neuroadaptation to neurodegeneration. Prog Neurobiol 56: 385-431.
- Criswell H E, Breese GR (2004) The Effect of Ethanol on Ion Channels in the Brain: A New Look. In Victor RP, Ronald RW, Comprehensive Handbook of Alcohol Related Pathology, Oxford: Academic Press, USA 865-869.
- Blomstrand E, Perrett D, Parry-Billings M, Newsholme EA (1989) Effect of sustained exercise on plasma amino acid concentrations and on 5-hydroxytryptamine metabolism in six different brain regions in the rat. Acta Physiol Scand 136: 473-481.
- Spirduso WW (1980) Physical Fitness, Aging, and Psychomotor Speed: A Review. J Gerontol 35: 850-865.
- Mukamal KJ, Kronmal RA, Mittleman MA, O'Leary DH, Polak JF, et al. (2003) Alcohol consumption and carotid atherosclerosis in older adults - The cardiovascular health study. Arterioscler Thromb Vasc Biol 23: 2252-2259.
- Verbaten MN (2009) Chronic effects of low to moderate alcohol consumption on structural and functional properties of the brain: beneficial or not?. Hum Psychopharmacol 24: 199-205.
- Gons RA, van Norden AG, de Laat KF, van Oudheusden LJ, van Uden IW, et al. (2011) Cigarette smoking is associated with reduced microstructural integrity of cerebral white matter. Brain 134: 2116-2124.
- Colcombe SJ, Kramer AF, Erickson KI, Scalf P, McAuley E, et al. (2004) Cardiovascular fitness, cortical plasticity, and aging. Proc Natl Acad Sci U S A 101: 3316-3321.
- Erickson KI, Prakash RS, Voss MW, Chaddock L, Hu L, et al. (2009) Aerobic fitness is associated with hippocampal volume in elderly humans. Hippocampus 19: 1030-1039.
- Seidenberg M, Guidotti L, Nielson KA, Woodard JL, Durgerian S, et al. (2009) Semantic memory activation in individuals at risk for developing Alzheimer disease. Neurology 73: 612-620.
- Bonda DJ, Wang X, Perry G, Nunomura A, Tabaton M, et al. (2010) Oxidative stress in Alzheimer disease: a possibility for prevention. Neuropharmacology 59: 290-294.
- Dai J, Jones DP, Goldberg J, Ziegler TR, Bostick RM, et al. (2008) Association between adherence to the Mediterranean diet and oxidative stress. Am J Clin Nutr 88: 1364-1370.
- Currais A, Fischer W, Maher P, Schubert D (2017) Intraneuronal protein aggregation as a trigger for inflammation and neurodegeneration in the aging brain. FASEB J 31: 5–10.
- Bilkei-Gorzo A, Albayram O, Draffehn A, Michel K, Piyanova A, et al. (2017) A chronic low dose of Δ9-tetrahydrocannabinol (THC) restores cognitive function in old mice. Nat Med.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi