Research Article, Int J Cardiovasc Res Vol: 7 Issue: 2
A Novel ECG Ward Telemetry System with Smartphone Based Alarm Escalation
Rainer Hoffmann1*, Jochen Michaelsen1, Lukas Langenbrink1, Mirlind Kastrati1, Michal Piatkowski1, Guido Hengemühle1, Tobias Schüll2 and Matthias Lammers3
1Department of Cardiology, Angiology and Sleep Medicine, Bonifatius Hospital Lingen, Lingen, Germany
2Philips Healthcare Germany, Hamburg, Germany
3Department of Information Technology, Bonifatius Hospital Lingen, Lingen, Germany
*Corresponding Author : Rainer Hoffmann, MD
Department of Cardiology, Angiology and Sleep Medicine, Bonifatius Hospital Lingen, Wilhelmstr. 13, 49808 Lingen, Germany
Tel: +49-591-910-6251
Fax: +49-591-910-6259
E-mail: rainer.hoffmann@hospital-lingen.de
Received: March 26, 2018 Accepted: April 10, 2018 Published: April 16, 2018
Citation: Hoffmann R, Michaelsen J, Langenbrink L, Kastrati M, Piatkowski M (2018) A Novel ECG Ward Telemetry System with Smartphone Based Alarm Escalation. Int J Cardiovasc Res 7:2. doi: 10.4172/2324-8602.1000345
Abstract
Background: Need for a permanent control person and alarm fatigue are limitations of telemetry surveillance systems ending at the central surveillance monitor. This study evaluated an escalation system expanding the alarm sequence by smartphones.
Methods: Telemetry system with 26 monitoring units and WLAN based alarm escalation system to three smartphones (Care Event, Philips) was evaluated during 128 days regarding major arrhythmia alarm (MAA) frequency, escalation of alarms within the system and response times. ECG triggering the MAA, patient name and position are shown on the smartphone display. MAA are forwarded initially to smartphone one. Forwarding of MAA to two further smartphones is actively triggered or occurs automatically after 20 sec without response by smartphone one.
Results: During the analysis period 11576 MAA were forwarded, ranging from 15 to 238 alarms/day. The number of MAA was minimal at 11 pm and maximal at 8 am (ratio 1:1.8). In 69% only smartphone 1 was involved, in 31% occurred an escalation to smartphone 2 and in 13% to smartphone 3. The median MAA response time at the smartphone was 8 sec at daytime and 9 sec at nighttime. 14 min of running time could be saved on average every day by direct visit of the patient triggering an alarm and omission of the central monitoring system.
Conclusions: A smartphone based alarm escalation system redundancies the permanent presence of nursing staff at the central surveillance system. The multilevel surveillance system with smartphone based escalation allows low alarm response times and warrants excellent surveillance quality
Keywords: Electrocardiogram; Cardiac rhythm; Monitoring; Smartphone; WLAN
Introduction
There is an increasing need for monitoring of vital patient parameters such as heart rate, blood pressure, and respiration rate as well as oxygen saturation. In addition, there are an increasing number of patients requiring the monitoring of cardiac rhythm for detection of rhythm disorders [1-5]. The majority of patients requiring monitoring of cardiac rhythm do not need the intensive care of a coronary care unit. These patients may be adequately monitored on a regular ward with the addition of a telemetry system.
In universally used ward telemetry systems the alarm sequence ends at the central surveillance system and monitor. Thus, there is the requirement for permanent presence of a control person at the central surveillance station responding to alarms which may be the result of a potentially dangerous and harmful rhythm disorders. A commonly applied alternative involves a loud alarm signal which is heard throughout the ward and requires the immediate visit of the central surveillance station by a staff nurse to check the reason and origin of the alarm. This is demanding regarding staff requirements. Furthermore, most alarms may be false alarms resulting in unnecessary nurse activities and time spent as well as the potential for alarm fatigue. More than 90% of alarms have been reported to be without clinical relevance and contributed to alarm desensitization [6,7]. Alarm fatigue is increasingly perceived as a limitation of conventional monitoring systems which has been linked to serious adverse events including death and may likely be underreported [7-10]. To lower the frequency of unrecognized serious rhythm events a dedicated nurse to continuously monitor the central alarm system has been proposed and found to be associated with increased fidelity of true rhythm event recognition [11].
A novel WLAN based escalation system has been developed which expands the alarm sequence from the central surveillance station further to several smart phones. It has obtained certification for reliable alarm forwarding. There are currently no reports on the clinical experience with the system. This study evaluated in clinical practice this novel system allowing the forwarding of major arrhythmia alarms (MAA) to smart phones thereby making permanent monitoring at the central surveillance station unnecessary. The analysis aimed at assessment of MAA frequency, frequency of MAA escalation, MAA response times as well as assessment of nurse experiences in patient care using the alarm escalation system.
Methods
Study setting
This study was performed in a secondary care hospital with 60 cardiology beds on 2 regular wards and a central monitoring system with 26 patient monitoring units covering both wards. 12 of the patient monitoring units are WLAN based telemetry systems allowing free movement of the patient within the ward area while 14 units are fixed bedside monitoring systems. There are WLAN spot points throughout both wards. The central unit on each of the two wards allows simultaneous display of all 26 monitored patient ECGs as well as further analysis of registered ECGs and alarms. In addition to this conventional centralized monitoring and alarm system, a WLAN based escalation system (CareEvent, Philips Medical Systems, 3000 Minuteman Road, Andover, MA 01810 USA) with 3 smartphones (Ascom, Baar, Switzerland) is part of the novel monitoring and alarm system. It is meant to expand the alarm sequence in case of a MAA. MAA were predefined as ventricular tachycardia, ventricular fibrillation, asystole and heart rate crossing a limit of either beyond 150 beats/min or below 45 beats/min. In special cases, the heart rate limits were altered corresponding to specific patient situations to reduce the number of unnecessary alarms. Once a MAA is forwarded to a smartphone, the display of the smartphone shows the ECG of the identified arrhythmia resulting in the alarm, the patients name and the room number of the patient within the ward. Alarms are forwarded in the first step to the smartphone of the nurse responsible for the care of the alarm generating patient. Forwarding of the alarm to a second and subsequently to a third smartphone level can be actively triggered instantaneously by the nurse or occurs automatically after 20 sec. (Asystole, VTach and Vfib-Tach) or 40 sec. (Extreme Tachy, extreme Brady, extreme arterial pressure, extreme oxygen saturation, extreme respiration rate) in case of missing response to the alarm by the first escalation level. During day shift 3 escalation levels within a ward are active, at night the third escalation level is switched to the other ward. MAA can be accepted using a smartphone. However, the central alarm system can only be completely reset (“silenced”) after each MAA at the central ward monitor or the patient monitor. Thus, after acceptance of a MAA using the smartphone, it is still later necessary to visit either the central monitor or the patient monitor.
The central monitoring and alarm escalation system saves by itself each alarm with the history of the alarm, including time at start of an alarm, time at escalation of alarm for each escalation level, time at alarm acceptance and end of alarm. For each MAA the reason of the alarm is stored. Thus, the system provides data on all alarms of the past. These data are provided in a SQL Database for further analysis. In this study only MAA were considered in the analysis. Indications for patient monitoring included status post syncope, acute coronary syndrome within the first 48 hours or prior to coronary angiography, status post percutaneous coronary intervention in acute coronary syndrome patients, new onset atrial fibrillation with initiated rhythm or frequency control, post resuscitation status with documented ventricular tachycardia or ventricular fibrillation until ICD implantation, documented symptomatic AV-Block until pacemaker implantation and immediately after pacemaker or ICD implantation, status post SVT or pulmonary vein ablation therapy, status post ICD shock until precipitating event treated.
The system was evaluated during a 128 day period between 01.12.2016 and 07.04.2017. Thus, all MAA noted by the system during this time period were included in the analysis.
To evaluate the potential time savings in the adequate recognition and response to MAA on the ward with the use of the Care Event system with alarm escalation as compared to a conventional central monitoring system only, the time to walk or run from all areas of the two wards directly to the patient or the central monitoring system whatever is shorter was compared to the time required to walk or run from any area of the two wards to the corresponding central monitoring system.
Statistical analysis
Statistical analysis was performed with the use of the SPSS software version 17.0 (SPSS, Inc., Chicago, Illinois, U.S.A.). Categorical data are presented as frequencies and were compared using Fischer´s Exact test. Continuous data are presented as mean ± standard deviation and were compared using Student´s t-test or ANOVA as adequate. A p<0.05 was considered significant.
Results
Alarm structure
Within the study period 11576 MAA were registered by the CareEvent server. All MAA have been forwarded within the CareEvent system. No alarm escalation failure was noted during the study period. In 45% of cases a ventricular tachycardia was defined by the system, in 21% of cases a high heart rate beyond the upper frequency limit was detected, in 16% of cases a low heart rate below the lower frequency limit was detected, in 11% a systole was detected, in 3% the alarm was due to low respiration movements, in 2% the system detected ventricular fibrillation and in 1% the cutaneous oxygen sensor indicated low oxygen saturation. There was a daily variation of alarms ranging from 15 to 238 alarms/day with an average of 90.4 alarms forwarded by the care event system/day.
The average number of MAA was 3.8 per hour. The number of MAA/hour varied with a minimum of 2.8 MAA/hour at 11 pm and a maximum at 8 am with 6.0 alarms/hour, indicating a ratio of 1:2.1.
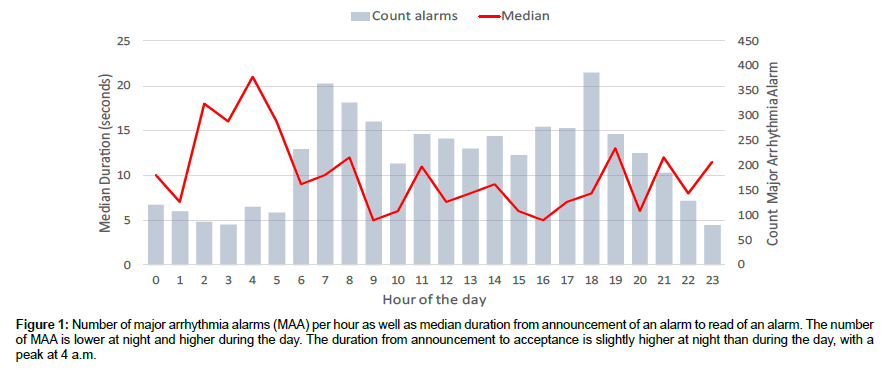
Alarm escalation
In 69% of the alarms, the CareEvent system forwarded the alarm only to smartphone 1, in 31% there was an additional escalation to smartphone 2 and in 13% escalation involved also to smartphone 3. The escalation frequency was higher during the day shift between 6 am to 5 pm when all escalation levels were on the same ward with escalation to level two in 35% and level three in 16% compared to during the night shift between 5 pm to 6 am, when the other ward was involved in the third escalation level with escalation to level two in 26% and level three in 11%. The median time to accept an alarm at the smartphone was 8 sec. during the day and 9 sec. during the night. There was a peak in the average time to acceptance of an alarm at 4 am. Figure 1 show the median duration between announcement and acceptance of an alarm during the day.
Figure 1: Number of major arrhythmia alarms (MAA) per hour as well as median duration from announcement of an alarm to read of an alarm. The number of MAA is lower at night and higher during the day. The duration from announcement to acceptance is slightly higher at night than during the day, with a peak at 4 a.m.
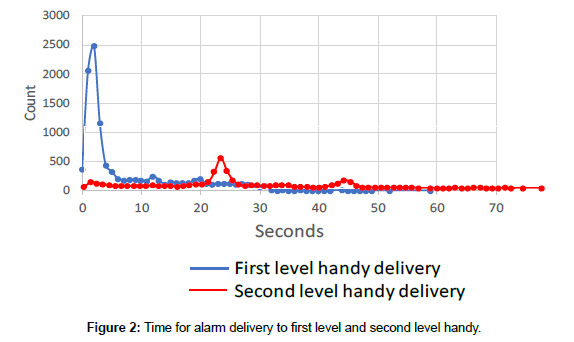
Time effect of care event application
The time for a nurse to quickly move from any point of the two wards to the central monitoring system was determined to range from 0 to 39 seconds, with the time to quickly move from any of the patient beds to the central monitoring system ranging from 9 to 39 seconds. Thus, the time required without the CareEvent application to respond to a MAA by moving to the central monitoring system and back to the initial point on the ward may by up to 78 seconds. Considering the average of 90.4 MAA per day and an average of 45 seconds spent per alarm with the conventional central monitoring system, a total of 67 min would be spent/day to respond to the daily MAA. Considering the mean time saved in each alarm event with the CareEvent application an average of 14 min of quick moving time could be saved every day by direct visit of the patient who triggered an alarm and omission of the central monitoring system which would have been looked after first otherwise (Figure 2).
Discussion
This study demonstrated that 1) response to all MAA is time consuming putting a high time burden on the nursing staff, 2) the smartphone based alarm escalation system was highly applicable without system failures, allowing the omission of a permanent control person at the central monitoring system, 3) escalation of MAA from the first alarm level to the second and third level was used in a considerable frequency, 4) time to acceptance of MAA was low throughout the day indicating no significant alarm fatigue, 5) there were moderate time savings with the smartphone based alarm escalation system due to less time spent to move around the ward.
Guidelines on the use of monitoring systems in the hospital setting deal with settings and indications for their application [1,2]. They have been set up to improve patient selection for monitoring, reduce alarm fatigue and improve monitoring quality. In the AHA (American Heart Association) Scientific Statement on practice standards for electrocardiographic monitoring in hospital settings, broad rationales for arrhythmia monitoring are mentioned (2). These are (I) the immediate recognition of sudden cardiac arrest to improve time to defibrillation, (II) the recognition of deteriorating conditions that may lead to a life-threatening, sustained arrhythmia, (III) arrhythmia monitoring to facilitate management of arrhythmias even if not immediately life-threatening, (IV) arrhythmia monitoring to facilitate diagnosis of arrhythmia or cause of symptoms such as syncope and palpitations to subsequently guide appropriate management. The settings which require permanent ECG monitoring or result in the recommendation to use it have also been described considering diagnosis and clinical situation [1,2,12]. Although the number of patients with permanent monitoring needs could be reduced, there is a high number of patients with permanent ECG monitoring in the hospital. In particular cardiology wards tend to be equipped with central monitoring systems allowing permanent ECG monitoring of several patients. However, there is only limited data on the clinical experience with hospital monitoring systems and their effect on patient outcome [13,14]. Hospital monitoring systems tie nursing staff and are time consuming to use. In addition to the initial placement at the patient, the permanent need for an experienced nursing staff to either be present at the central monitoring system or check each alarm at the central alarm system is very time consuming. The time requirements in clinical practice are not well defined. Furthermore, these systems may generate a high number of false and non-actionable alarm signals distracting the nurse, bothering the patient and potentially desensitizing nurses and clinicians to respond to the alarms. Significant attention has been spent to evaluate alarm artifacts and improve alarm settings and thereby reduce false alarms [15-18]. Even off-site monitoring has been evaluated to improve monitoring quality [19].
Thus, potential overuse and limited effects on patient outcomes with conventional telemetry and monitoring systems have been noted [2,9,12,20]. An alarm escalation system, which redundantises permanent presence at a central monitoring system and reduces other time requirements will increase acceptance of the system, may potentially increase patient safety and improve the balance of efforts spent to those of enhanced patient outcomes.
This is the first description of a novel smartphone based alarm escalation system allowing less dependency on the central monitoring system. The system received high acceptance by the nursing staff, was found to have excellent reliability, and resulted in moderate time savings due to less required movements of the nurse to check alarms. This study allowed also interesting insights into the frequency of MAA requiring immediate attention by a nurse. In this observational study an average of almost 4 major alarms was registered per hour indicating that there is a permanent need to be involved and respond to the system as well as the potentially alarm causing rhythm disorders. Although the frequency is dependent on alarm setting, a similar frequency has been reported in the ALARMED study [14]. These alarms were more frequent in the early hours of the day compared to at night. This may have been due to more true rhythm disorders. However, the major cause may have been a higher rate of false alarms due to patient movements. In most alarms the response was initiated by the nurse being contacted by the escalation system in the first level. However, in 35% of cases during the day and 26% of cases at night escalation of the alarm to a further level was initiated, indicating that the option to escalate is frequently used as it may allow pursuing current activities with less interruption compared to a conventional monitoring system. The time interval between MAA onset and alarm acceptance was low. It was low during the day and at night indicating excellent patient surveillance and safety as well as absent alarm fatigue.
References
- Drew BJ, Califf RM, Funk M, Kaufman ES, Krucoff MW, et al. (2004) Practice standards for electrocardiographic monitoring in hospital settings: an American Heart Association scientific statement from the Councils on Cardiovascular Nursing, Clinical Cardiology, and Cardiovascular Disease in the Young: endorsed by the International Society of Computerized Electrocardiology and the American Association of Critical-Care Nurses. Circulation 110: 2721-2467.
- Sandau KE, Funk M, Auerbach A, Barsness GW, Blum K, et al. (2017) American Heart Association Council on Cardiovascular and Stroke Nursing; Council on Clinical Cardiology; and Council on Cardiovascular Disease in the Young. Update to Practice Standards for Electrocardiographic Monitoring in Hospital Settings. A Scientific Statement from the American Heart Association. Circulation 136: e273-e344.
- Estrada CA, Rosman HS, Prasad NK, Battilana G, Alexander M, et al. (1995) Role of telemetry monitoring in the non-intensive care unit. Am J Cardiol 76: 960-965.
- Brignole M, Alboni P, Benditt D, Bergfeldt L, Blanc JJ, et al. (2001) Guidelines on management (diagnosis and treatment) of syncope. Eur Heart J 22: 1256-1306.
- Moya A, Sutton R, Ammirati F, Ammirati F, Blanc JJ, et al. (2009) Guidelines for the diagnosis and management of syncope (version 2009): The Task Force for the Diagnosis and Management of Syncope of the European Society of Cardiology (ESC). Eur Heart J 30: 2631-2671.
- Lawless ST (1994) Crying wolf: False alarms in a pediatric intensive care unit. Critical Care Medicine 22: 981-985.
- Sendelbach S, Funk M (2013) Alarm fatigue: A patient safety concern. AACN Advanced Critical Care 24: 378-386.
- Stukshis I, Funk M, Johnson CR, Parkosewich JA (1997) Accuracy of detection of clinically important dysrhythmias with and without a dedicated monitor watcher. Am J Crit Care 6: 312-317.
- Henriques-Forsythe MN, Ivoneye CC, Kamuguisha LKK, Jamched U, Olejeme KA, et al. (2009) Is telemetry overused? Is it as helpful as thought? Cleveland Clinic Journal of Medicine 76: 368-372.
- Knight BP, Pelosi F, Michaud GF, Strickberger SA, Morady F (1999) Clinical consequences of electrocardiographic artifact mimicking ventricular tachycardia. New England Journal of Medicine 341: 1270-1274.
- Funk M, Parkosewich JA, Johnson CR, Stukshis I (1997) Effect of dedicated monitor watchers on patients’ outcomes. Am J Crit Care 6: 318-323.
- The Joint Commission. NPSG.06.01.01 on Clinical Alarm Safety for Hospitals.
- Schull MJ, Redelmeier DA (2000) Continuous electrocardiographic monitoring and cardiac arrest outcomes in 8, 932 telemetry ward patients. Acad Emerg Med 7: 647-652.
- Atzema C, Schull MJ, Borgundvaag B, Slaughter GR, Lee CK (2006) ALARMED: adverse events in low-risk patients with chest pain receiving continuous electrocardiographic monitoring in the emergency department: a pilot study. Am J Emerg Med 24: 62-67.
- Burgess LPA (2009) Alarm limit settings for early warning systems to identify at risk patients. Journal of Advanced Nursing 65: 1844-1852.
- Siebig S, Kuhls S, Imhoff M, Gather U, Schölmerich J, et al. (2010) Intensive care unit alarms: How many do we need? Critical Care Medicine. 38:451-456.
- Keller KB, Lemberg L (2007) Electrocardiographic artifacts. American Journal of Critical Care. 16: 90-92.
- Márquez MF, Colín L, Guevara M, Iturralde P, Hermosillo AG (2002) Common electrocardiographic artifacts mimicking arrhythmias in ambulatory monitoring. American Heart Journal. 144: 187-197.
- Cantillon DJ, Loy M, Burkle A, et al. (2016) Association between off-site central monitoring using standardized cardiac telemetry and clinical outcomes among non-critically ill patients. JAMA 316: 519-524.
- Hollander JE, Valentine SM, McCuskey CF, Brogan Jr GX (1997) Are monitored telemetry beds necessary for patients with nontraumatic chest pain and normal or nonspecific electrocardiograms? Am J Cardiol 79: 1110-1111.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi