Short Article, Int J Cardiovasc Res Vol: 9 Issue: 8
A Rare Case of Multiple Valve Infective Endocarditis Complicated by Septic Pulmonary Embolism in a Young Patient
Rime Benmalek*, Zeine El Abasse, Karim Mounaouir and Rachida Habbal
Department of Cardiology, Hospital University Center Ibn Rochd, Casablanca, Morocco
*Corresponding Author: Dr. Rime Benmalek
Resident in Department of cardiology, Hospital University Center Ibn Rochd, Casablanca, Morocco
Tel: +212 607 717 951
E-mail: Rime.benmalek@gmail.com
Received: November 05, 2020 Accepted: December 02, 2020 Published: December 09, 2020
Citation: Benmalek R, Abasse ZE, Mounaouir K, Habbal R (2020) A Rare Case of Multiple Valve Infective Endocarditis Complicated by Septic Pulmonary Embolism in a Young Patient. Int J Cardiovasc Res 9:8.. doi: 10.37532/icrj.2020.9(8).426
Abstract
Septic Pulmonary Embolism (SPE) is an uncommon and severe complication of infective endocarditis that requires early diagnosis and proper management in order to prevent mortality.
Keywords: Septic Pulmonary Embolism
Case Report
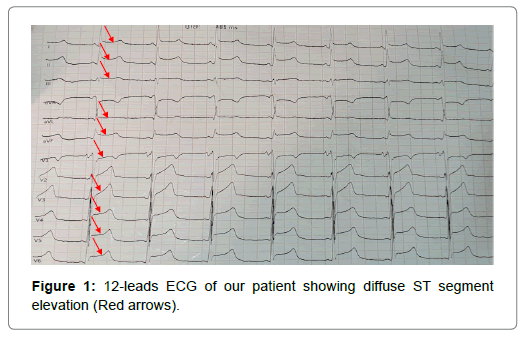
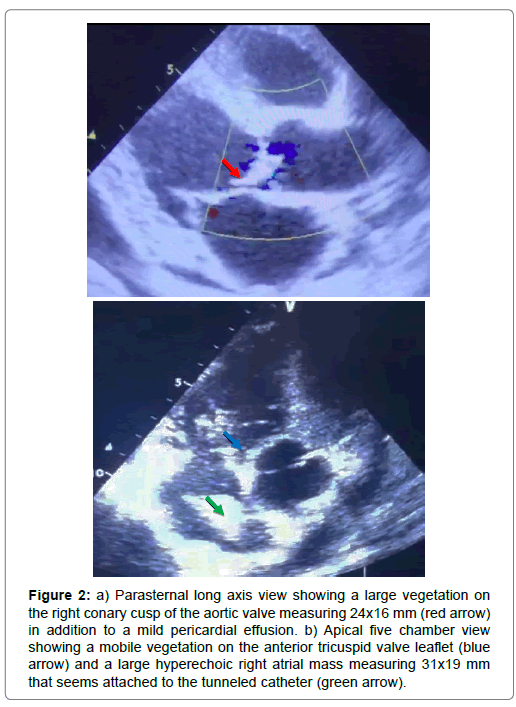
We report the case of a 39-year-old man who recently started hemodialysis for end-stage kidney disease through a tunneled catheter, who presented to the emergency department with chest pain associated with New York Heart Association (NYHA) III dyspnea, fever and severe asthenia that started 3 days ago. Physical examination found a febrile (38.2°C), normotensive (blood pressure at 126/77 mmHg) patient, with tachycardia (heart rate at 105/ min) and low oxygen saturation at 94%. Moreover, the patient had moderate bilateral lower limb edema, abdominal swelling and indistinct heart and lung sounds on auscultation. 12-leads Electrocardiogram (ECG) showed non-evolutive diffuse ST segment elevation (Figure 1). Transthoracic Echocardiography (TTE) was performed and showed thickened Aortic Valves with a large vegetation on the right conary cusp measuring 24x16 mm (Figure 2a), associated to a moderate aortic regurgitation, in addition to a mobile vegetation on the anterior tricuspid valve leaflet (Figure 2b) and a large hyperechoic mass measuring 31x19 mm was found in the right atrium attached to the dialysis catheter (Figure 2b). The patient also had polyserositis according to the thoraco-abdominal Computed Tomography (CT) with mild circumferential pericardial effusion, moderate pleural effusion and severe ascites. Cerebral CT scan was normal and blood tests revealed high C-reactive protein level (214 mg/L) and procalcitonin (2.6 mg/L), in addition to hyperneutrophilia (17 400/mm3), normocytic normochromic anemia (Hemoglobin 7.1 g/dL), hypoalbuminemia (24 g/L) and severely altered Renal function (Glomerular filtration rate (according to the Modification of Diet in Renal Disease equation)=8 mL/min). Moreover, both blood and catheter cultures came positive for Methicillin-Resistant Staphylococcus Aureus (MRSA). We concluded to the diagnosis of multiple Infective Endocarditis (IE) on native valve starting from the tunneled catheter and initiated antibiotherapy with Vancomycin 30 mg/Kg/day after removing the catheter. The patient didn’t respond to the antibiotherapy and presented on the 6th day of onset a severe respiratory distress associated to hemoptysis, with echocardiographic signs of acute cor pulmonale and significant reduction of the right atrial vegetation’s size. Despite several attempts of resuscitation, the patient unfortunately deceased of a massive septic pulmonary embolism.
Figure 2: a) Parasternal long axis view showing a large vegetation on the right conary cusp of the aortic valve measuring 24x16 mm (red arrow) in addition to a mild pericardial effusion. b) Apical five chamber view showing a mobile vegetation on the anterior tricuspid valve leaflet (blue arrow) and a large hyperechoic right atrial mass measuring 31x19 mm that seems attached to the tunneled catheter (green arrow).
Discussion
Cardiac device endocarditis associated with SPE is a rare and serious disorder associated with significant morbidity and mortality [1]. It is characterized by embolization of infected vegetations from a primary infectious site into the venous circulation with implantation into pulmonary vasculature resulting in parenchymal infection [2]. Although right sided vegetations are the main source of cardiac SPE [3], this condition can also be caused by double-sided vegetations like it was the case in our patient.
The clinical presentation varies from an insidious illness with fever and respiratory symptoms such as cough, pleuritic chest pain, dyspnea and hemoptysis to an acute sepsis syndrome that can sometimes be fatal like for our patient [2]. The diagnosis should be rapidly suspected in a febrile bacteremic patient especially in the context of a known underlying IE, who develops acute secondary pulmonary symptoms. It remains a difficult diagnosis due to its varied clinical presentations but can be confirmed in the right clinical context, by a characteristic pattern on CT Pulmonary angiography showing multiple bilateral peripheral pulmonary nodules, often pleural based, with or without cavitation’s [4,5]. Additional investigations including blood cultures and cardiac ultrasound can be performed to look for valvular lesions in case of unknown association with IE, and also for signs of acute cor pulmonale that are usually seen in non-infective Pulmonary Embolism (PE) and are exceptional in SPE, but their presence is associated with a poor outcome [2], which was the case of our patient.
The management of these patients remains challenging and must be discussed by the heart team. Source control and prolonged antimicrobial therapy are the cornerstones of the management of SPE [6]. The choice of antibiotic therapy depends on the causative organisms, the pharmacokinetics and pharmacodynamics of the available drugs. Aside from antimicrobial therapy and removal of infected devices, patients with IE and acute onset of SPE symptoms, must undergo timely surgery, performed within the first two days after diagnosis, in order to avoid increased risk of septic in-hospital complications and mortality [7]. It is confirmed in the latest recommendations that indicate pulmonary involvement such as septic emboli or cavitation as one of the key indications for surgery in right-sided IE [8]. In a recent chinese retrospective study, all patients who underwent cardiac surgery survived and only 1 of 6 patients who did not receive surgery survived, and the other 5 who received antibiotics without surgery died [9]. In Cook et al. [1] case series, all 14 patients recovered from SPE after surgery, confirming the importance of early cardiac surgery to eradicate the source of the septic emboli in patients with cardiac SPE.
Concerning anticoagulation which is the major treatment in non-infective PE, it has been a controversial topic in the management of IE and septic emboli due to the increased risk of bleeding in the area of the infected embolus [10]. Its administration depends on the requirements of cardiac surgery and whether the infection is controlled, in addition to the presence of a pre-existing indication such as mechanical valve replacement or atrial fibrillation in the absence of other contraindications [11].
Conclusion
Finally, patients with severe sepsis syndrome and respiratory distress require management in critical care with vasoactive and respiratory support, which should have been the case of our patient before rapid deterioration of his respiratory state.
References
- Cook RJ, Ashton RW, Aughenbaugh GL, Ryu JH (2005) Septic pulmonary embolism: presenting features and clinical course of 14 patients. Chest. 128:162-166.
- Goswami U, Brenes JA, Punjabi GV, LeClaire MM, Williams DN, et al. (2014) Associations and outcomes of septic pulmonary embolism. Open Respir Med J. 8:28-33
- Liu S, Xie J, Chen Y, Yang J, Zhang J, et al. (2014) Presenting features and clinical course of 34 patients with septic pulmonary embolism caused by right-sided infective endocarditis. Chin Med J (Engl). 127:2735-2739.
- Huang RM, Naidich DP, Lubat E, Schinella R, Garay SM, et al. (1989) Septic pulmonary emboli: CT-radiographic correlation. AJR Am J Roentgenol. 153:41-45
- Iwasaki Y, Nagata K, Nakanishi M, Harada H, Kubota Y, et al. (2001) Spiral CT findings in septic pulmonary emboli. Eur J Radiol. 37:190-194.
- Lee SJ, Cha SI, Kim CH, Park JY, Jung TH, et al. (2007) Septic pulmonary embolism in Korea: microbiology, clinicoradiologic features, and treatment outcome. J Infect. 54:230-234.
- Ali A, Raza S, Khan R, Bechard D, Kaszala K, et al. (2012) Septic pulmonary embolism in a patient with defibrillator lead endocarditis. Am J Respir Crit Care Med. 185:e2.
- Habib G, Lancelotti P, Antunes MJ, Bongiorni MJ, Casalta JP, et al. (2015) 2015 ESC Guidelines for the management of infective endocarditis: The task force for the management of infective endocarditis of the European Society of Cardiology (ESC) endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM). European Heart Journal. 36:3075-3128.
- Song XY, Li S, Cao J, Xu K, Huang H, et al. (2016) Cardiac septic pulmonary embolism: A retrospective analysis of 20 cases in a Chinese population, Medicine (Baltimore). 95: e3846.
- Aslam AF, Aslam AK, Thakur AC, Vasavada BC, Khan IA, et al. (2005) Staphylococcus aureus infective endocarditis and septic pulmonary embolism after septic abortion. Int J Cardiol. 105:233-235.
- Davis KA, Huang G, Petty SA, Tan WA, Malaver D, et al. (2020) The Effect of preexisting anticoagulation on cerebrovascular events in left-sided infective endocarditis. Am J Med. 133:360-369.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi