Research Article, Int J Cardiovasc Res Vol: 8 Issue: 2
Assessment of Rheumatic Heart Disease Adherence to Secondary Prophylaxis and Factor Affecting Among Patients with Rheumatic Heart Disease Attending Jimma University Teaching Hospital, South West of Ethiopia
Ahmed AA* and Germossa GN
Jimma University, College of Health Science, Department of Nursing and Midwifery, Ethiopia
*Corresponding Author : Abdulwahid Awol Ahmed
Jimma University, College of Health Science, Department of Nursing and Midwifery, Ethiopia
E-mail: abdiiawol@gmail.com
Received: February 23, 2018 Accepted: Mar 04, 2019 Published: April 02, 2019
Citation: Ahmed AA, Germossa GN (2019) Assessment of Rheumatic Heart Disease Adherence to Secondary Prophylaxis and Factor Affecting Among Patients with Rheumatic Heart Disease Attending Jimma University Teaching Hospital, South West of Ethiopia. J Cardiovasc Res 8:2. doi: 10.4172/2324-8602.1000375
Abstract
Background:
Rheumatic heart disease is a chronic heart condition caused by rheumatic fever that can be prevented and controlled by secondary prophylaxis. However, there is paucity of information on adherence of patients to rheumatic heart disease secondary prophylaxis in Jimma, southwest of Ethiopia.
Objective:
To assess level of adherence to secondary prophylaxis and factor affecting among patients with rheumatic heart disease attending Jimma University Teaching Hospital, Cardiac clinic.
Methodology:
Facility based cross-sectional study was done on all rheumatic heat disease patients (277) coming for follow-up during specified period at Jimma University Teaching Hospital cardiac follow-up clinic. Records of all patients were reviewed. Using structured questionnaire the patients or their attendants were interviewed. The descriptive statistics and chi square were used to analyze/compute some variables by using computer.
Results:
Of the total 277 who gave responses, 249 (89.9%) took rheumatic heart disease secondary prophylaxis and all of them used benthanthine penicillin. One fifth (20.5%) patients out of 249 on secondary prophylaxis missed their regular injection at least once. Distance from treatment center and knowledge on disease prevention were strongly associated with adherence to rheumatic heart disease secondary prophylaxis (p<0.03).
Conclusion and Recommendation:
About one-fifth of the patients were missed their secondary prophylaxis and the main reasons were distance from hospital, lack of money, dissatisfaction with staff and lack of knowledge. Educating patients/care givers on the cause and prevention rheumatic heart disease as well as complication following missing of secondary prophylaxis are helpful to improve adherence level of patients to secondary prophylaxis.
Keywords: Rheumatic heart disease; Secondary prophylaxis; Adherence; Jimma
Abbreviations
RHD: Rheumatic Heart Disease; RF: Rheumatic Fever; JUTH: Jimma University Teaching Hospital
Introduction
Rheumatic heart disease (RHD) is a chronic heart condition caused by rheumatic fever (RF) that can be prevented and controlled by secondary prophylaxis [1-4].
Research evidence suggests that RHD can be prevented by monthly administration of long-acting penicillin, benzanthine penicillin injection or oral erythromycin in patients with allergy to penicillin [5-7]. Secondary prevention benefits clients by preventing recurrent attack of acute rheumatic fever. This can be done by regular administration of antibiotics which may be the only feasible option in the third world countries as compared to resource intensive surgical repair of heart valves [1].
Secondary prophylaxis should be effective and can be effective only when adherence to recommended follow up is ensured. But adherence to chronic disease treatment is a global challenge. For instance just over one-third (35%) RHD cases on follow up in Brazil, over two-fifth (41%) in Australia and half of study participants in 12 different countries in Africa, Yemen and India are non-adherent to medication [8-10].
Research report across the world shows that availability and acceptability of health services, educational status, residency, painful injection site, lack of knowledge and perception on ARF/RHD communities [9,11,12] are factors associated with adherence.
Distance from the nearest health facility was determined to assess access to health care. Previous studies in developing countries have showed that distance of 5 kilometres or less to a health unit predicted better access to health care [13]. The study done in Cape Town, South Africa shows that, patients who stayed far from the health facilities (>10 km) were significantly associated with poor compliance [14].
In Ethiopia, 4.6-6.4 per 1000 children estimated to have RHD and 22% of them on regular prophylaxis [15]. But to what extent they are adhering to this secondary prophylaxis and which factors affect adherence is not known, particularly in Jimma zone. Thus, this study investigated adherence to secondary prophylaxis and factors affecting among patients in Jimma context.
Method and Material
Study area and period
The study was conducted in Jimma University teaching hospital cardiac clinic, which is located at 357km south west from Addis Ababa. Currently it provides follow up care for 1890 adults and 338 pediatric patients with different cardiac diseases out of which RHD patients are 731. The study was conducted from March 12 to April 15/2015.
Study design
Facility based cross sectional study was conducted to determine rheumatic heart disease adherence to secondary prophylaxis and factors affecting among patients with rheumatic heart disease attending Jimma University Teaching Hospital, cardiac clinic.
Populations
Source population: All rheumatic heart disease patients on follow up.
Study population: The sampled rheumatic heart diseases patients coming for follow up.
Sample size and sampling technique
Sample size: In order to determine sample size, single proportion formula was used based on the following assumptions:
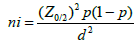
Where ni= the initial sample; P= 0.5(50%) prevalence; Z = 95%=1.96 confidence interval; d= 5%=0.05 – the desired precision of the estimate/ margin of error ; N= 731 = total RHD patients on follow up.
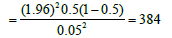
Since our source population is less than 10,000 which are 731 we use the correction formula.
nf corrected=ni/(1+ni/N) = 384/(1+384/731) = 252
With 10% of non-response rate the final sample size was =277
Sampling technique: Convenient sampling method was used.
Study variables
Dependent variables: Level of adherence to secondary prophylaxis, is the dependent variable while
Independent variable: Sex, Age, Address, ethnicity, Religion, Educational status, Knowledge about disease, Secondary prophylaxis, Income, and Condition of the patients are independent variables.
Data collection process
The structured questionnaire was prepared in English language that fulfill the objective of the study were adopted through reviewing of different literatures and previous similar studies. The instrument adapted from different literatures developed for similar purpose by different authors. Data were collected using structured questionnaire from patients or their attendants those came for follow up during specified period. Three data collectors were recruited among graduating class of nursing students.
Data processing and analysis
Data were processed and analysed using master sheet, manual scientific calculator, and computer. The result was summarized and presented in tables and figure with description. The frequency, percentage and cross tabulation of variables were done.
Ethical considerations
Official letter of approval was obtained from Jimma University, department of nursing and brought to hospital administrative bodies, the purpose of the study had explained and permission was obtained from Jimma University Teaching Hospital. To keep privacy of patients the name of the patients were not written in the questionnaire and before interviewing, informed consent was obtained from patients or care givers after explaining the purpose of the study and, they were also informed that, the information obtained from them will not be disclosed to the third body.
Data quality assurance
The quality of data was ensured though training of data collectors, close supervision and reviewing of each of the completed questionnaire daily. Data consistence and completeness were checked though out collection, data entry and analysis.
Result
Socio-demographic characteristics
A total of 277 RHD patients participated in the study giving response rate of 100%. Of the total respondents, majority140 (51%) of them were female and 78(28.2%) were in age range of 15-29 years. Majority of respondents were Muslim 173(62.4%) by religion and 185(66.8%) of them were from Oromo ethnic group. About 103 (37.2%) of patients or their attendants were illiterate, 125(45.1%) of them were from rural residence and 127(45.8%) of them were farmers. About 157(56.0%) respondents had monthly income below 1710 birr and the nearest distance was 1km and the furthest distance was 240 km (Table 1).
| Socio-demographic characteristics | Number | Percentage | |
|---|---|---|---|
| Sex | Male | 137 | 49.0 |
| Female | 140 | 51.0 | |
| Total | 277 | 100 | |
| Age | <15 | 63 | 22.7 |
| 15-29 | 78 | 28.2 | |
| 30-44 | 64 | 23.1 | |
| 45-59 | 56 | 20.2 | |
| ≥ 60 | 16 | 5.8 | |
| Total | 277 | 100 | |
| Religion | Muslim | 173 | 62.4 |
| Orthodox | 74 | 26.7 | |
| Protestant | 30 | 10.8 | |
| Ethnicity | Oromo | 185 | 66.8 |
| Amhara | 40 | 14.4 | |
| Dawro | 23 | 8.3 | |
| Gurage | 20 | 7.2 | |
| Others | 9 | 2.9 | |
| Total | 277 | 100 | |
| Family income | <570 | 8 | 2.9 |
| 570-1139 | 47 | 17.0 | |
| 1140-1709 | 100 | 36.1 | |
| 1710-2279 | 49 | 17.7 | |
| ≥ 2280 | 73 | 26.4 | |
| Total | 277 | 100 | |
| Educational status (patient/care taker) | Illiterate | 103 | 37.2 |
| Read and write only | 9 | 3.2 | |
| Grade 1-4 | 68 | 24.6 | |
| Grade 5-8 | 49 | 17.7 | |
| Grade 9-10 | 17 | 6.1 | |
| Grade 11-12 | 7 | 2.5 | |
| >12 | 24 | 8.7 | |
| Total | 277 | 100 | |
| Occupation | Farmer | 127 | 45.8 |
| Government employee | 45 | 16.2 | |
| Merchant | 84 | 30.3 | |
| Daily labor | 21 | 7.6 | |
| Total | 277 | 100 | |
| Address | Urban | 152 | 54.9 |
| Rural | 125 | 45.1 | |
| Total | 277 | 100 | |
| Distance from JUTH | ≤10 | 84 | 30.3 |
| >10 | 193 | 69.7 | |
| Total | 277 | 100 | |
Table 1: Socio-demographic characteristics of RHD patients affected with rheumatic heart disease attending JUTH cardiac clinic, Jimma, Ethiopia, 2015.
Knowledge about the disease
From a total of 277 patients the majority of them 223(80.5%) did not know the cause of their or their child’s illness, some of them 21(7.6%) said infection of the throat and heart, few of them 13 (4.5%) associated it with heavy work, and others 5(1.8%) with hereditary. Almost all of them 223 (80.5%) did not know how to prevent the occurrence of rheumatic heart disease, even though few of them 54(19.5%) suggested early treatment as preventive method (Table 2).
| Knowledge of disease prevention | Number | Percentage |
|---|---|---|
| Yes | 54 | 19.5 |
| No | 223 | 80.5 |
| Total | 277 | 100 |
Table 2: Knowledge of prevention among patients affected with rheumatic heart disease attending JUTH cardiac clinic Jimma, Ethiopia, 2015.
RHD secondary prophylaxis adherence
Out of the total 277 respondents, majority of them 249(89.9%) were took secondary prophylaxis during follow-up. All of them were using benzanthine penicillin as secondary prophylaxis. From a total of 249 rheumatic heart disease patients who took secondary prophylaxis, 51(20.5%) of them missed their regular injection at least once.
Factor affecting RHD secondary prophylaxis adherence
Distance from JUTH and knowledge on disease prevention of the patients/care givers were statistically strongly associated with missing of secondary prophylaxis in this study with p-value 0.000 and 0.007 respectively. Age of the patients, monthly family income and sex of the patients were not significantly associated with missing of secondary prophylaxis (Tables 3 and 4).
| Socio-demographic Variables | Ever miss secondary prophylaxis | X2 | p-value | |||
|---|---|---|---|---|---|---|
| Yes(n,%) | No (n,%) | Total (n,%) | ||||
| Educational status (patient/care taker) |
Illiterate | 29(11.6) | 62(24.9) | 91(36.5) | 14.737 | 0.022 |
| Read and write only |
1(0.4) | 7(2.8) | 8(3.2) | |||
| Grade 1-4 | 7(2.8) | 54(21.7) | 61(24.5) | |||
| Grade 5-8 | 6(2.4) | 43(17.3) | 49(19.7) | |||
| Grade 9-10 | 4(1.6) | 13(5.2) | 17(6.8) | |||
| Grade 11-12 | 0(0.0) | 7(2.8) | 7(2.8) | |||
| >12 | 4(1.6) | 12(4.8) | 16(6.4) | |||
| Total | 51(20.5) | 198(79.5) | 249(100) | |||
| Occupation | Farmer | 33(13.2) | 81(32.5) | 112(45.0) | 9.822 | 0.025 |
| Government employee |
5(2.0) | 36(14.4) | 41(16.4) | |||
| Merchant | 11(4.4) | 66(26.5) | 77(30.9) | |||
| Daily labour | 2(0.8) | 15(6.0) | 17(6.8) | |||
| Total | 51(20.5) | 198(79.5) | 249(100) | |||
| Address | Urban | 21(8.4) | 113(45.4) | 134(53.8) | 4.122 | 0.042 |
| Rural | 30(12.0) | 85(34.1) | 115(46.2) | |||
| Total | 51(20.5) | 198(79.5) | 249(100) | |||
| Distance from JUTH |
≤ 10 | 6(2.4) | 71(28.5) | 77(30.9) | 11.021 | 0.001 |
| >10 | 45(18.1) | 127(51.0) | 172(69.1) | |||
| Total | 51(20.5) | 198(79.5) | 249(100) | |||
Table 3: Association between selected socio-demographic characteristics and missing of secondary prophylaxis among patients affected with rheumatic heart disease attending JUTH cardiac clinic Jimma, Ethiopia, 2015.
| Knowledge of disease prevention | Ever miss secondary prophylaxis | X2 | p-value | ||
|---|---|---|---|---|---|
| Know | 4(7.4) | 50(92.6) | 54(21.7) | 7.237 | 0.007 |
| Do not know | 47(24.1) | 148(75.9) | 195(78.3) | ||
| Total | 51(20.5) | 198(79.5) | 249(100) | ||
Table 4: Association between knowledge of disease prevention and missing of secondary prophylaxis among patients affected with rheumatic heart disease attending JUTH cardiac clinic Jimma, Ethiopia, 2015.
Reason for missing prophylaxis and their perception towards their illness
The main reasons to miss their regular prophylaxis was distance from hospital 23(45.1%) followed by lack of money 21(41.2%). The majority 243(87.7%) of patients were improved during follow-up (Tables 5 and 6).
| Reason for missing secondary prophylaxis | Frequency | Percentage (%) |
|---|---|---|
| Distance from hospital | 23 | 45.1 |
| Lack of money | 21 | 41.2 |
| Dissatisfaction with clinic staff | 14 | 27.4 |
| Lack of knowledge | 13 | 25.5 |
| Total | 71 | 139.2 |
Table 5: Reason for missing secondary prophylaxis among patients affected with rheumatic heart disease attending JUTH cardiac clinic Jimma, Ethiopia, 2015.
| Condition of the patient | Frequency | Percentage (%) |
|---|---|---|
| Improving | 243 | 87.7 |
| Same | 28 | 10.1 |
| Deteriorating | 6 | 2.2 |
| Total | 277 | 100 |
Table 6: Patient’s perception of condition of their illness during follow up among patients affected with rheumatic heart disease attending JUTH, Jimma, Ethiopia, 2015.
Discussion
Rheumatic heart disease (RHD) is a chronic heart condition caused by rheumatic fever (RF). It can be prevented and controlled by monthly administration of benzanthine penicillin injection or oral erythromycin [5-7]. These agents are the only available secondary prophylaxis [1-4] as an option to surgical repair of heart valves [1] in resource limited countries. The use of secondary prophylaxis benefits clients by preventing recurrent attack of acute rheumatic fever. However, this can only be achieved when client use regular secondary prophylaxis regimen. The adherence level of RHD to secondary prophylaxis is context based and varies from country to country. The current study identified adherence level and associated factors with patients to RHD secondary prophylaxis in south west Ethiopia.
In this study, 89.9% of the patients took secondary prophylaxis. This is almost four fold higher than national estimate (22%) [15]. All of clients took benzanthine penicillin which is in accordance with various studies and medical text books recommendations [5-7].
In the current study about one-fifth (20.5%) of patients missed their secondary prophylaxis at least once during follow up. This implies that 79.5% patients who should have taken their regular prophylaxis are at risk of recurrent rheumatic fever attack which may leads to development of further complication. The current adherence level is by far lower than adherence reports from Brazil (35%) [8] and Australia (41%) [9]. Another recent study conducted in Africa and Asia [10] shows nearly half of study participants were not adhered to antibiotic prophylaxis which is over two folds of this study. The difference may be attributed to difference in socio economic status, availability & accessibility of health care facility, health care system, year of study, study design, sample size and methods of analysis of adherence. Distance from hospital, lack of money, dissatisfaction with staff and lack of knowledge are main reasons for non-adherence. Whereas, while availability and acceptability are main reason for poor adherence in Brazil [8], lack of active recall system and negative perception to secondary prophylaxis were reported reasons in Australia [9].
Even though 20.5% of the patients were missed their regular injection at least once, 87.7% of them reported perceived improvement in their health condition during follow-up. This is consistent with WHO reports on the effects taking regular secondary prophylaxis [5,6,11].
Estimated distance from service center (JUTH), knowledge of disease prevention, educational status, Occupation and residency (urban or rural) are associated with adherence to RHD secondary prophylaxis adherence (P<0.05). This is relatively similar with study done in remote area of Australia [9] and Cape Town, South Africa [14]. Study is the first of its kind in the study area and provided information on RHD secondary prophylaxis service, deterrence level and associated factor. However, it fails to establish cause-effect relationship between adherence level and the identified factors. It would have been better if it was prospective analytical study in order to identify independent predictors
Conclusions and Recommendations
Most of the patients were taking secondary prophylaxis and all of them were using benzanthine penicillin. And about one-fifth of them was not adhered to secondary prophylaxis and missed their regular injection at least once. Distance from hospital, lack of money, dissatisfaction with staff and lack of knowledge were the main reason to miss their injection. Educating patients/care givers on the cause and prevention rheumatic heart disease as well as complication following missing of secondary prophylaxis are helpful to improve adherence level of patients to secondary prophylaxis. Further epidemiologic research is needed to better answer the question as to what makes some patients adhere to their injection and others not.
Acknowledgement
We would like to acknowledge Jimma University for giving us this golden chance, study participants and Jimma University Teaching Hospital Health professionals for their unreserved support for the realization of the study.
References
- Mendis S, Puska P, Norrving B (2011) Global Atlas on Cardiovascular Disease Prevention and Control. World Health Organization (in collaboration with the World Heart Federation and World Stroke Organization), Geneva 2011.
- Diao M, Kane A, Ndiaye MB, Mbaye A, Bodian M, et al. (2011) Pregnancy in women with heart disease in Sub-Saharan Africa. Arch Cardiovasc Dis 104: 370-374.
- Koegelenberg CF, Doubell AF, Orth H, Reuter H (2003) Infective endocarditis in the western cape province of south Africa: A three-year prospective study. QJM 96: 217-225.
- Benjamin EJ, Wolf PA, D’Agostino RB, Silbershatz H, Kannel WB, Levy D (1998) Impact of atrial fibrillation on the risk of death: the Framingham heart study. Circulation 98: 946-952.
- Robert M Kliegman, Richard E Behrman, Hal B Janson and Bonita F Stanton (2007) Nelson Text book of pediatric. (18th Edtn) Elsevier - Health Sciences Division New York.
- Faucin AS, Wiener C, Longo DL, Kasper DL (2012) New York heart Association functional classification: Harrison`s 17th edition principle of internal medicine, McGraw-Hill Education, New York.
- Abraham G (1982) Pattern of cardiovascular disease among adults hospitalized in Ethiopian. Ethiop med J, 20: 63-68.
- Pelajo CF, Lopez-Benitez JM, Torres JM, de Oliveira SK (2010) Adherence to secondary prophylaxis and disease recurrence in 536 Brazilian children with rheumatic fever. Pediatric Rheumatol online 8: 22
- Harrington Z, Thomas DP, Currie BJ, Bulkanhawuy J (2006) Challenging perceptions of non-compliance with rheumatic fever prophylaxis in a remote Aboriginal community MJA 184: 514-517.
- Zuhlke L, Engel ME, Karthikeyan G, Rangarajan S, Mackie P, et al. (2015) Characteristics, complications, and gaps in evidence-based interventions in rheumatic heart disease: the Global Rheumatic Heart Disease Registry (the REMEDY study) Eur heart J 36: 1115a-1122a.
- Rheumatic Fever and Rheumatic heart disease report of a WHO expert consultation, world health organization Geneva 2004 (Technical report series No 923).
- Wilson N, Charles K M (2013) Benzathine penicillin adherence for secondary prophylaxis among patients affected with rheumatic heart disease attending Mulago Hospital. Cardiovasc J Afr 24: 124-129.
- World Health Organization (2003) Adherence to long-term therapies. Evidence for action. Geneva, Switzerland: World Health Organization.
- Walker KG, Human DG, De Moor MM, Sprenger KJ (1987) The problem of compliance in rheumatic fever. S Afr Med J 72: 781-783.
- Yadeta D, Tesfaye G, Abraha G, Bekele A, Tamre W, et.al. (2005) Knowledge of rheumatic fever and RHD in rural Ethiopia. Ethiopia.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi 



