Research Article, Int J Cardiovasc Res Vol: 8 Issue: 6
Assessment of the Relation between Average Aortic Valve Sclerosis Score Index and Severity of Coronary Artery Disease in Patients with Acute Coronary Syndrome
Mahmoud Shawky Abd El Moneum*
Cardiology Department, Faculty of Medicine, Benha University, Egypt
*Corresponding Author: Mahmoud Shawky Abd El Moneum
Cardiology Department, Faculty of Medicine, Benha University, Egypt
Tel: +20 109 567 1308
E-mail: m_zaki86@yahoo.com
Received: August 05, 2019 Accepted: August 20, 2019 Published: August 27, 2019
Citation: El Moneum MSA (2019) Assessment of the Relation between Average Aortic Valve Sclerosis Score Index and Severity of Coronary Artery Disease in Patients with Acute Coronary Syndrome. Int J Cardiovasc Res 8:6.
Abstract
Objectives: The aim of this study was to assess the relation between average aortic valve (AV) sclerosis score index (AVSSI) and severity of coronary artery disease (CAD) in patients with acute coronary syndrome (ACS).
Patients and methods: A total of 100 patients with ACS were studied. They were classified into 2 equal groups of 50 patients each. Group (1) involved patients with average AVSSI>1 and group (2) involved patients with average AVSSI ≤ 1. They were matched in age and sex. For these patients electrocardiography (ECG), conventional echocardiography, coronary angiography and SYNTAX score were determined.
Results: The study found that there is a strong correlation between CAD and average AVSSI (r=0.791, p<0.001). There is increase in the incidence of average AVSSI with increase of CAD risk factors such as hypertension, diabetes mellitus, dyslipidemia, male gender, aging, family history, smoking, increased blood calcium and body mass index (BMI). Also there is decrease in LVEF % in group 1 (43.6 ± 7.14) compared to group 2 (51.2 ± 6.98) with statistically significant difference (p<0.001), while there is increase in E/e’ in group 1 (9.68 ± 3.58) compared to group 2 (5.68 ± 3.27), p<0.05. The prevalence of three-vessel CAD was higher in group 1 (24%) than in group 2 (8%), p<0.001. SYNTAX score was higher in average AVSSI>1 (16.4 ± 9.67) than average AVSSI ≤ 1 patients (8.82 ± 10.1), p<0.001.
Conclusion: It is concluded that there is a strong relationship between average AVSSI and severity of coronary artery disease, and is consistent with other high-risk echocardiographic findings.
Keywords: Coronary artery disease; Aortic valve sclerosis; Acute coronary syndrome
Introduction
Aortic valve sclerosis (AVS) is a form of AV disease affecting an estimated 1 in 4 people above the age of 65 years. An aging population and more widespread use of noninvasive imaging are increasing the incidence of AVS [1]. AVS is typically defined as calcification of the aortic leaflets without impairment in leaflet excursion or a significant transvalvular pressure gradient [2]. It is characterized by a gradual progression beginning with calcium deposition that may ultimately transform to aortic stenosis (AS) with obstruction of outflow from the left ventricle. Severe AS eventually leads to ventricular remodeling and hemodynamic compromise with a high morbidity and mortality if not treated. Long considered an incidental age‐related degenerative process as a result of progressive wear and tear, there is substantial emerging evidence related to AVS that challenges this assumption [1].
Aortic sclerosis is defined by conventional echocardiography, as a focal area of micro-calcification and thickening of a trileaflet aortic valve, in the absence of commissural fusion and/or obstruction of ventricular outflow (antegrade velocity across the valve <2.5 m/s). Its frequency increases with age: 21–29% of adults aged >65 years exhibit aortic valve sclerosis, whereas the frequency increases to 48% in individuals >84 years [3].
Recent observations have shown that the development of AVS and AS may involve chronic inflammatory infiltrates, deposition of atherosclerotic lipoproteins, and calcification, akin to CAD. However, AVS has unique features, including calcium predominance on histology, gradual progression, and location at a site of high pressure that serves as a gateway from the heart to the systemic circulation. Some investigators have reported the frequent coexistence of either AVS or AS in patients with underlying CAD [4].
Several studies have demonstrated that independent risk factors in the progression of CAD, such as dyslipidemia, hypertension, and male sex, may also affect development of AVS and its progression to AS [5]. These observations not only highlight the many shared characteristics of CAD and AVS but have also prompted investigators to test the efficacy of medical interventions that may have salutary effects on both conditions [1].
Heart disease is the leading cause of death in the Egyptians. The majority of these deaths are attributed to CAD. Improvements in treatment for CAD, such as statins, angiotensin inhibitors (ACEI), and revascularization, have resulted in a larger proportion of the population living with CAD [6]. Realizing the potential similarities between the underlying pathophysiology for AVS and CAD, many clinically relevant questions remain unanswered [7]. For instance, does the presence of AVS suggest existence or progression of underlying CAD? Should AVS be considered a novel risk factor for the development of CAD? Does the finding of AVS warrant the initiation and careful titration of medications with lifestyle changes analogous to current strategies used in treating patients with diabetes mellitus? This study tried to answer these questions.
Aim
The aim of this study was to assess the relation between average aortic valve sclerosis score index and severity of coronary artery disease in patients with acute coronary syndrome.
Patients and Methods
Study design and population
The study was performed in Benha university hospital in the period of one year from March 2018 to March 2019 on 100 patients with ACS of them 50 patients with average AVSSI>1 represent group (1) and 50 patients with average AVSSI ≤ 1 represent group (2).
Inclusion criteria included patients presented with ACS represent the population of this study classified into two equal groups as mentioned above, they were matched in age and sex, both sexes included in the study.
Exclusion criteria included patient refusal, heart muscle disease (severe heart failure and cardiomyopathy), severe myocarditis, significant arrhythmia, previous pacemaker implantation, or cardiac surgery.
All participants included in this study were subjected to:
• Informed consent: each participant has to perform written consent
• Full history taking: including history of hypertension, diabetes mellitus and smoking habit.
• General and local examination of the heart
• 12 lead ECG
• Routine laboratory tests including: complete blood picture, liver functions, renal functions, serum calcium and lipid profile.
• Conventional echocardiography was performed for all the participants within 24 hours of admission by the same operator.
• Coronary angiography was performed for all patients.
Conventional echocardiographic diagnosis of aortic sclerosis
Echocardiography was performed on all patients within 24 hour of admission. The presence of aortic sclerosis was assessed by echocardiography (Vivid 7 Dimension ultrasound framework, GE Healthcare, Waukesha, WI, USA) using a 2.5 MHz probe [8]. The aortic valve was zoomed in the parasternal long axis view to 8 cm. Three loops of 3 cardiac cycles each were recorded ensuring that the aortic valve leaflets are visible in diastole. Sclerosis grading was recorded according to the visual sclerosis score (VSS) which assigned to each valve on the basis of its 2D appearance in the parasternal short axis view [9].
0=normal
1=slight increase in reflectance of the cusp bodies or margins
2=mild increase in overall reflectance and cusp thickness
3=generalized hyper-reflectance, cusps markedly thickened with markedly hyper-reflective masses.
For the purpose of subsequent analysis, the presence of aortic sclerosis was defined as an average aortic valve sclerosis score index (AVSSI) of ≥ 1. Doppler echocardiography was used to assess velocity in the LV outflow tract and through the aortic valve [6].
Other echocardiographic parameters
The left ventricular ejection fraction (LVEF) and variables of left ventricular diastolic function and filling pressure, such as transmitral pulsed Doppler early diastolic velocities (E wave), early diastolic tissue Doppler mitral annular velocities (e’), and E/e’ ratio, were also determined.
Coronary angiography
Coronary angiography in multiple views was performed according to the standard Judkins or Sones technique. At least five views, including two orthogonal views, were acquired for the left coronary artery and at least two orthogonal views for the right coronary artery. Angiographic results were interpreted by the angiographers who had no knowledge of conventional echocardiographic findings. Coronary angiography was applied to identify plaques (at least 20%) indicating the presence of atherosclerosis. Significant CAD was defined as 50% reduction in the internal diameter of left main vessel or >70% reduction in the internal diameter of other vessels (left anterior descending artery, left circumflex artery and right coronary artery). The definition of 1-, 2- or 3-vessel disease was based on the criteria of the Coronary Artery Surgery Study [10].
N.B: SYNTAX score (SS)
The Synergy between Percutaneous Coronary Intervention with Taxus and Cardiac Surgery (SYNTAX) score (SS) is an angiographic method for grading the complexity and intensity of CAD and provides more comprehensive evaluation of properties of the coronary lesion [11].
The SS is used to evaluate the complexity of CAD. Coronary arteries larger than 1.5 mm in diameter and with stenosis of ≥ 50% were included for evaluation. The online latest updated version (2.11) was used to calculate the SS (www.SYNTAXscore.com, accessed in October 2014). SSs were divided into 2 groups (low SYNTAX: <22, high SYNTAX: ≥ 22). All angiographic variables were computed by 2 cardiologists who were unaware of the study data (ST, UA). In the case of disagreement the final decision was made by consensus [12].
Statistical Analysis
Measurable investigation was performed utilizing Statistical Package for Social Sciences (SPSS) variant 23.0 for windows (SPSS Inc., Chicago, IL, USA). Numeric values are reported as means ± SD or as proportions of the sample size. Comparisons between the study and control groups were made with the Chi square (χ2) test for categorical data and Student’s t-test for continuous data. Intra- and inter-observer variability was assessed ANOVA test. Multiple logistic regression analysis (backward stepwise) was applied to evaluate the association of significant CAD with AVS and other coronary risk factors. A p value <0.05 was considered significant, while p>0.05 was considered non-significant.
Results
This study included 100 patients with signs of acute coronary syndrome, of them 50 with average AVSSI>1 (group 1), they were 36 (72%) of them were males and 14 (28%) were females, and 50 with average AVSSI ≤ 1 (group 2), they were 30 (60%) were males and 20 (40%) were females. There were no significant differences as regard age and gender between the two groups, i.e. they were matched in age (Table 1).
| Variable | AVSSI>1 (N=50) |
AVSSI ≤ 1 (N=50) |
Statistical test of significance | |||
|---|---|---|---|---|---|---|
| N | % | N | % | χ2-test | p value | |
| Age (years): • ≤ 60 • >60 |
50 12 38 |
100 24 76 |
50 29 21 |
100 58 42 |
0.021 9.26(1) 5.54(2) |
0.197 0.001* 0.018* |
| Sex: • Males • Females |
50 36 14 |
100 72 28 |
50 30 20 |
100 60 40 |
0.021 7.24(1) 5.96(2) |
0.197 0.003* 0.028* |
Table 1: Age and sex distribution of the studied groups.
Assessment of cardiovascular risk factors
All risk factors in this study (hypertension, diabetes mellitus, smoking, dyslipidemia, family history, Body Mass Index and calcium) showed a statistically significant difference (p<0.05) as presented in Table 2.
| Risk factors | AVSSI>1 (n=50) | AVSSI ≤ 1 (n=50) | Statistical test of significance | |||
|---|---|---|---|---|---|---|
| N | % | N | % | χ2-test | p value | |
| Hypertension | 38 | 76.0 | 20 | 40.0 | 6.218 | 0.011* |
| Diabetes mellitus | 32 | 64.0 | 16 | 32.0 | 5.946 | 0.026* |
| Dyslipidemia | 28 | 56.0 | 23 | 46.0 | 5.021 | 0.044* |
| Smoking | 34 | 68.0 | 12 | 24.0 | 7.069 | 0.0042* |
| Family history | 24 | 48.0 | 19 | 38.0 | 4.492 | 0.041* |
| BMI (Kg/m2): • <20 • >20 |
8 42 |
16.0 84.0 |
28 22 |
56.0 44.0 |
6.297 | 0.0032* |
| Calcium:
• 0–1 • 2–3 |
6 44 |
12.0 88.0 |
38 12 |
76.0 24.0 |
8.845 | 0.0013* |
Table 2: Risk factors in the studied groups.
Patients’ clinical conditions
There was a statistical non-significant difference as regard presence of STEMI, non-STEMI and unstable angina in the two groups (p>0.05) as shown in Table 3.
| Patients clinical conditions | AVSSI>1 (n=50) | AVSSI ≤ 1 (n=50) | Statistical test of significance | |||
|---|---|---|---|---|---|---|
| N | % | N | % | F-test | p value | |
| STEMI | 20 | 40.0 | 21 | 42.0 | 0.173 | 0.256 |
| NSTEMI | 20 | 40.0 | 16 | 32.0 | 0.164 | 0.201 |
| Unstable angina | 10 | 20.0 | 13 | 26.0 | 0.297 | 0.158 |
Table 3: Patients clinical conditions in the studied groups.
Aorti valvesclerosis grading in the studied groups
There was statistically highly significant difference in each grade of AVS (p<0.001) in group (1) compared to group (2) as illustrated in Table 4.
| Grade | AVSSI>1 (n=50) | AVSSI ≤ 1 (n=50) | Statistical test of significance | |||
|---|---|---|---|---|---|---|
| N | % | N | % | χ2-test | p value | |
| 0 | 0 | 0.0 | 44 | 88.0 | - | - |
| 1 | 0 | 0.0 | 6 | 12.0 | - | - |
| 2 | 37 | 76.0 | 0 | 0.0 | 19.223 | 0.0000* |
| 3 | 13 | 26.0 | 0 | 0.0 | 13.621 | 0.0000* |
| Average AVSSI | 1.49 ± 0.43 | 0.79 ± 0.28 | t= 26.201 | 0.001* | ||
Table 4: Average AVSSI by conventional echocardiography in the studied groups.
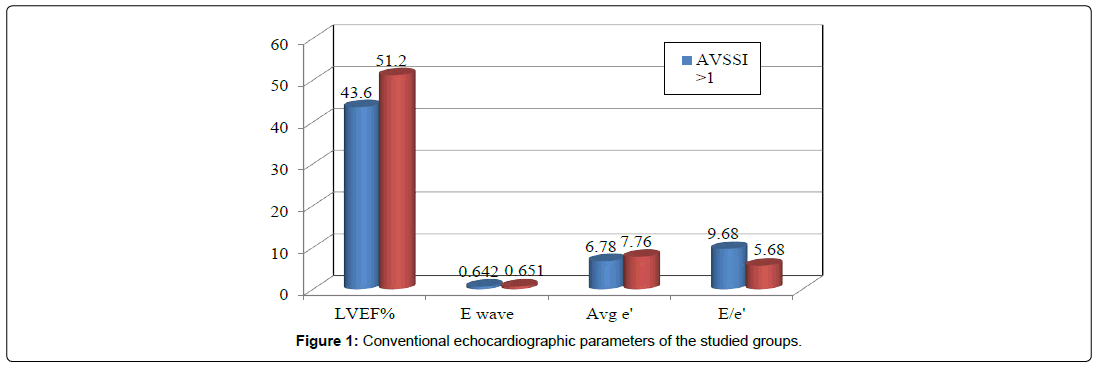
Conventional echocardiographic parameters of the studied groups
There was a statistical significant difference (p<0.001) as regard the left ventricular ejection fraction (LVEF) percent which decreases in group (1) compared to group (2), and also there is a statistical significant difference (p<0.05) as regard E/e’ ratio that increase in group (1) compared to group (2), (Figure 1) (Table 5).
| Variable (Mean ±SD) |
AVSSI>1 (n=50) | AVSSI ≤ 1 (n=50) | t-test | p value |
|---|---|---|---|---|
| LVEF (%) | 43.6 ± 7.14 | 51.2 ± 6.98 | 8.554 | 0.001* |
| E wave (m/s-1) | 0.642 ± 0.17 | 0.651 ± 0.18 | 0.324 | 0.117 |
| Avg e’ (cm/s-1) | 6.78 ± 1.92 | 7.76 ± 1.94 | 7.225 | 0.027* |
| E/e’ | 9.68 ± 3.58 | 5.68 ± 3.27 | 7.951 | 0.011* |
Table 5: Conventional echocardiographic parameters of the studied groups.
Coronary angiography findings in the studied groups
There was a statistically highly significant difference (p<0.001) in the prevalence of 3 vessels CAD in group (1) compared to group (2) that illustrated in Table 6.
| Number of obstructive vessels (Lesion >70%) |
AVSSI>1 (n=50) | AVSSI ≤ 1 (n=50) | Statistical test of significance | |||
|---|---|---|---|---|---|---|
| N | % | N | % | χ2-test | p value | |
| 0 | 0 | 0.0 | 10 | 20.0 | - | - |
| 1 | 18 | 36.0 | 18 | 36.0 | 0.00 | 0.999 |
| 2 | 20 | 40.0 | 18 | 36.0 | 2.55 | 0.079 |
| 3 | 12 | 24.0 | 4 | 8.00 | 10.62 | 0.001* |
Table 6: Relation between CAD by coronary angiography and average AVSSI groups.
SYNTAX score (SS) of the studied groups
There was a statistical significant difference as regard the mean SS in group (1) compared to group (2) (Table 7).
| SYNTAX score | AVSSI>1 (n=50) | AVSSI ≤ 1 (n=50) | Statistical test of significance | ||||
|---|---|---|---|---|---|---|---|
| N | % | N | % | χ2-test | p value | ||
| Low (<22) | 24 | 48.0 | 48 | 96.0 | - | - | |
| High (≥22) | 26 | 52.0 | 2 | 4.00 | 13.372 | 0.000* | |
| Mean ± SD | 16.4 ± 9.67 | 8.82 ± 10.1 | 2.719^ | 0.006* | |||
Table 7: SYNTAX score by conventional echocardiography in the studied groups.
Discussion
Greater attainment of ideal cardiovascular health in midlife to late life is associated with a lower prevalence of AV disease in late life, attainment of ideal cardiovascular health and valvular heart disease is unknown [13].
In 2010, the American Heart Association Strategic Planning Task Force and Statistics Committee defined the concept of ideal cardiovascular health as the attainment of 4 health behaviors (body mass index <25 kg/m2, absent of smoking, physical activity, and healthy diet) and 3 health factors (untreated blood pressure <120/<80 mmHg, fasting blood glucose <100 mg/dL, and untreated total cholesterol <200 mg/dL) [14].
This study included 100 patients with signs of acute coronary syndrome, of them 50 with average AVSSI>1 (group 1), they were 36 (72%) of them were males and 14 (28%) were females, and 50 with average AVSSI ≤ 1 (group 2), they were 30 (60%) were males and 20 (40%) were females. There were no significant differences as regard age and gender between the two groups, i.e. they were matched in age (Table 1), however males (72%) are more affected than females (28%) in AVSSI>1 patients, in our study.
This was coincides with Shavelle et al. [15] who found 67% of AVSSI were males and Milin et al. [1] found 66% male patients had AVS. Korkmaz et al. [16] and Milin et al. [1] considered male gender as a risk factor for AVS.
In this study most of patients were above 60 years of age. This was in agreement with Soydinc et al. [10] stated that male gender (72%) and Sengeløv et al. [13] who reported that average AVS increased with age. They reported increased prevalence of average AVS above 80 years of age. Soydinc et al. [10] stated that patients with average AVS were significantly older than those without AVS (54.9 ± 8.3 vs. 47.6 ± 8.3 years; p<0.001). Also Bhatt et al. [7] demonstrates an increase in the prevalence of AVS with aging, especially in patients >71 years old. AVS has been consistently linked with age and is considered a marker of senile degenerative changes resulting from hemodynamic stress in heart [11].
In this study, there was increase in the incidence of average AVS with increase of CAD risk factors such as hypertension (76%), diabetes mellitus (64%), dyslipidemia (56%), family history (48%), smoking (68%), increased blood calcium (88%) and body mass index (BMI) (84%). This was similar to many authors such as Shavelle et al. [15] who found hypertension (67%), smoking (40%), DM (35%), hyperlipidemia (42%), and family history (42%) as risk factors for AVS. Korkmaz et al. [16] found risk factors for AVS as hypertension (88%), DM (13%), smoking (16%), and dyslipidemia (26%), however they mentioned that they were insignificant which opposing to our results.
In another study Soydinc et al. [10] stated that diabetes mellitus (32%), hypertension (44%) and smoking (50%) were also more common in AVSSI patients (group 2) than group 1 (p=0.006, 0.004, 0.027 and 0.029, respectively). Of the serum lipid evaluation, total cholesterol levels (206.02 ± 29.9 vs. 180.3 ± 34.06 mg/dl; p<0.001) and LDL cholesterol levels (130 ± 23.35 vs. 107.34 ± 19.31; p<0.001) were higher in the AVSSI patients than control in that study. HDL cholesterol levels and body mass index were similar between groups.
We did not find a significant relation between the two groups as regard patients conditions (STEMI, NSTMI and unstable angina), p>0.05. As regard high SYNTAX Score (SS) in this study we found high statistically significant relation between group (1) and (2). SS was high in 26 patients (52.0%) of AVSSI>1 group (1) with mean of 16.4 ± 9.67 and only in 2 patients (4%) of AVSSI ≤ 1 group (2), with mean of 8.82 ± 10.1, p value was highly significant (<0.001).
In agreement with this study Topcu et al. [12] reported that the high SS group had significantly higher AVS positivity compared to the low SS group (31.3% vs. 10.6%, p< 0.001 and OR=3.8, 95% CI: 2.4–6.1) as there were 28 AVS positive and 237 AVS-negative cases in the low SS group, there were 87 AVS-positive and 191 AVS-negative cases in the high SS group.
Opposing to our results Bhatt et al. [7] found that the presence of AVS was not associated with SYNTAX score (p=0.684). They stated that angiographic interpretation of coronary lesion characteristics and SYNTAX score (using an algorithm) was limited to an experienced interventional cardiologist, which eliminates the inter-observer variability.
Conventional echocardiographic evaluation of AVS may help to detect the presence of CAD and to determine the severity of relevant CAD at rest using a noninvasive procedure that requires only a few minutes [10].
In this study there was a statistical significant difference (p<0.001) as regard the left ventricular ejection fraction (LVEF) percent which decreases in patients with AVSSI>1 (group 1) compared to patients with AVSSI ≤ 1 (group 2), from mean ± SD of 43.6 ± 7.14 to 51.2 ± 6.98 percent, respectively, and also there is a statistical significant difference (p<0.05) as regard E/e’ ratio that increase in group (1) with mean of 9.68 ± 3.58 compared to group (2) with a mean of 5.68 ± 3.27.
These results coincide with Topcu et al. [12] who stated that LVEF was lower in group 1 (median, 47) than in group 2 (median 55) which was statistically highly significant (p<0.001).
There is a statistically highly significant correlation between severity of CAD and number of affected vessels (multivessel lesion) with average aortic valve sclerosis index (p<0.001). We have shown that existence of ACS and its severity, and AVSSI are related to each other.
In agree with our results, in a study of 160 patients, Soydinc et al. [10] found that AVS was associated with the presence of triple vessel CAD and was independently associated with Gensini score. Of the 50 patients with AVS, 45 were found to have CAD compared with 88 of the 110 patients without AVS. The AVSSI patients had a higher rate of 3-vessel disease (AVS group vs. non-AVS: 40 vs. 13.6%; p<0.001). However, no significant correlation was found between AVS and the presence or absence of 1- or 2-vessel disease.
Also, Mazzone et al. [3] reported that aortic sclerosis was found in 49% of 415 patients and, at 1-year follow-up, patients with acute coronary syndromes. They found also that coronary artery disease was found in 76% of patients with a similar prevalence of the presence or not of aortic valve sclerosis.
Opposing to our study Bhatt et al. [7] found that the presence of AVS was not associated with number of obstructive vessels (p=0.831), lesions with >70% stenosis in major (p=0.849) and minor (p=0.1) epicardial arteries, lesions with 50-70% stenosis in major (p=0.267) and minor (p=0.237) epicardial arteries or SYNTAX score (p=0.684). They added that AVS should not be used in isolation from cardiovascular risk factors as a noninvasive indicator of coronary atherosclerosis, and its use as a marker for severe obstructive CAD remains a topic of debate.
A study of 230 patients from Fazlinezhad et al. [17] found AVS to be an independent predictor of obstructive coronary disease (i.e., >50% stenosis).
In a large study of a cohort of more than 2000 patients with aortic valve sclerosis, 16% developed aortic stenosis, with 10.5% in mild stenosis and 2.5% in severe stenosis, over a time interval of 8 years [18]. A similar percentage was observed in a smaller group of patients, although only a small percentage of patients with aortic sclerosis progress to aortic stenosis: 2-4% of adults aged over 65 years [19].
From the above results and studies we can say that there is a strong association between CAD and average AVSSI. The mechanisms suggested for the similarity between AVS and atherosclerosis are as follows: 1) AVSSI has risk factors for atherosclerosis, 2) AVSSI and atherosclerosis have similar histopathological characteristics, and 3) it was shown that AVSSI and CAD are related to systemic atherosclerosis, just like the relation of carotid artery disease and peripheral arterial disease with systemic atherosclerosis [20,21].
Conclusion
It is concluded that there is a strong relationship between average AVSSI and severity of coronary artery disease, and is consistent with other high-risk echocardiographic findings.
Limitations
The major limitations of this study is the lack of control (normal) group which may be useful for comparison of diseased and normal values, the small number of study which may give inaccurate statistical comparison between the two studied groups and lastly the limited duration of this study that may affect the studying of all parameters and risk factors.
References
- Milin AC, Vorobiof G, Aksoy O, Ardehali R (2014) Insights into aortic sclerosis and its relationship with coronary artery disease. J Am Heart Assoc 3: e001111.
- Freeman RV, Otto CM (2005) Spectrum of calcific aortic valve disease: pathogenesis, disease progression, and treatment strategies. Circulation 111: 3316-3326.
- Mazzone A, Venneri L, Berti S (2007) Aortic valve stenosis and coronary artery disease: pathophysiological and clinical links. J Cardiovasc Med (Hagerstown) 8: 983-989.
- Losi MA, Brevetti G, Schiano V, Barbati G, Parisi V, et al. (2010) Aortic valve sclerosis in patients with peripheral and/or coronary arterial disease. Echocardiography 27: 608-612.
- Owens DS, Budoff MJ, Katz R, Takasu J, Shavelle DM, et al. (2012) Aortic valve calcium independently predicts coronary and cardiovascular events in a primary prevention population. JACC Cardiovasc Imaging 5: 619-625.
- Nabel EG, Braunwald E (2012) A tale of coronary artery disease and myocardial infarction. N Engl J Med 366: 54-63.
- Bhatt H, Sanghani D, Julliard K, Fernaine G (2015) Does aortic valve sclerosis predicts the severity and complexity of coronary artery disease? Indian Heart J 67: 239-44.
- Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, et al. (2015) Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging 16: 233-270.
- Ngo DTM, Wuttke RD, Turner S, Marwick TH, Horowitz JD (2004) Quantitative assessment of aortic sclerosis using ultrasonic backscatter. J Am Soc Echocardiogr 17: 1123.
- Soydinc S, Davutoglu V, Dundar A, Aksoy M (2006) Relationship between aortic valve sclerosis and the extent of coronary artery disease in patients undergoing diagnostic coronary angiography. Cardiology 106: 277-282.
- Head SJ, Farooq V, Serruys PW, Kappetein AP (2014) The SYNTAX score and its clinical implications. Heart 100: 169-177.
- Topcu S, Aksu U, Kalkan K, Gülcü O, Kalayci Karabay A, et al. (2017) Aortic valve sclerosis is associated with the extent of coronaryartery disease in stable coronary artery disease. Turk J Med Sci 47: 614-620.
- Sengelov M, Cheng S, Biering-Sørensen T, Matsushita K, Konety S, et al. (2018) Ideal Cardiovascular Health and the Prevalence and Severity of Aortic Stenosis in Elderly Patients. J Am Heart Assoc 7: e007234.
- Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, et al. (2010) Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s Strategic Impact Goal through 2020 and beyond. Circulation 121: 586-613.
- Shavelle DM, Buljabasic N, Takasu J, Babaie A, Rosales J, et al. (2006) Validation of the severity index by cardiac catheterization and Doppler echocardiography in patients with aortic sclerosis and stenosis. Cardiovasc Ultrasound 4: 12.
- Korkmaz L, Agac MT, Bektas H, Varol MO, Erkan H, et al. (2013) Aortic valve sclerosis is a sign of increased arterial stiffness in clinically asymptomatic subjects. Cardiol J 20: 318-322.
- Fazlinezhad A, Leila Hosseini L, Yousefzadeh H (2013) Correlation between aortic valve sclerosis and coronary artery disease: a cross e sectional study. J Cardio-Thoracic Med 1: 20e25.
- Cosmi JE, Kort S, Tunick PA, Rosenzweig BP, Freedberg RS, et al. (2002) The risk of the development of aortic stenosis in patients with ‘benign’ aortic valve thickening. Arch Intern Med 162: 2345-2234.
- Chandra HR, Goldstein JA, Choudhary N, Neill CS, George PB, et al. (2004) Adverse outcome in aortic sclerosis is associated with coronary artery disease and inflammation. J Am Coll Cardiol 43:169-175.
- Coffey S, Cox B, Williams MJ (2014) The prevalence, incidence, progression, and risks of aortic valve sclerosis: a systematic review and meta-analysis. J Am Coll Cardiol 63: 2852-2861.
- Rossi A, Gaibazzi N, Dandale R, Agricola E, Moreo A, et al. (2014) Aortic valve sclerosis as a marker of coronary artery atherosclerosis; a multicenter study of a large population with a low prevalence of coronary artery disease. Int J Cardiol 172: 364-367.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi