Review Article, Int J Cardiovasc Res Vol: 9 Issue: 4
Cardiopulmonary Exercise Testing in Children and Adolescents: Focusing on the Oxygen Uptake Efficiency Slope
Reizo Baba*, Koji Kitatsuji, Yukiko Okamura, Norio Hotta and Hisayoshi Ogata
Department of Lifelong Sports and Health Sciences, Chubu University College of Life and Health Sciences, Japan
*Corresponding Author: Dr. Reizo Baba
Department of Lifelong Sports and Health Sciences, Chubu University College of Life and Health Sciences, 1200 Matsumoto-cho, Kasugai, Aichi 487-8501, Japan
Tel: 81568519212
E-mail: reizobaba@gmail.com
Received: June 06, 2020 Accepted: June 22, 2020 Published: June 29, 2020
Citation: Baba R, Kitatsuji K, Okamura Y, Hotta N, Ogata H (2020) Cardiopulmonary Exercise Testing in Children and Adolescents: Focusing on the Oxygen Uptake Efficiency Slope. Int J Cardiovasc Res 9:4. doi: 10.37532/icrj.2020.9(4).405
Abstract
Cardiopulmonary Exercise Testing (CPET) is a clinical testing that allows for the analysis of gas exchange during exercise. Maximal oxygen uptake (VO2max), comprehensive index of cardiac, respiratory, and skeletal muscle functions, is one of the most important measurements obtained in CPET. Anaerobic threshold, the exercise intensity at which lactate starts to accumulate in the blood, is widely used, as it represents an exercise level that is not too strenuous, but not too mild. The Minute Ventilation/Carbon Dioxide Output relationship (VE/VCO2 slope) is often used as a prognostic marker of cardiac failure. The Oxygen Uptake Efficiency Slope (OUES), a submaximal index of cardiorespiratory functional reserve, correlates strongly with VO2max and is utilized as a prognostic tool for various heart diseases including congenital heart defects.
Keywords: Cardiopulmonary exercise testing; Oxygen uptake; Oxygen uptake efficiency slope
Introduction
In our everyday clinical practices of pediatric cardiology, various clinical tests at rest, e.g., chest x-ray, electrocardiogram, echocardiogram, blood gas analysis, serum biochemical tests, etc. are essential and indispensable for their evaluation. However, these clinical tests at rest can only observe, in a sense, extraordinary sedentary unloaded physiological functions of the patients, not at all their status during everyday activities like playing, exercising, standing, or sleeping. Therefore, appropriate evaluations of their physiological and cardiopulmonary responses to various stresses are essential in our clinical practices.
CPET is a test indispensable for the evaluation of functional reserve in subjects with cardiorespiratory diseases, predicting their prognosis, and effectiveness of treatment [1]. Therefore, this review overviews the basics of various measurements obtained from CPET sessions, e.g., VO2max, Anaerobic Threshold (AT), the VE, VCO2regression slope (VE/VCO2 slope), and the OUES, in mainly pediatric population.
What does the VO2max mean?
The VO2max, one of the most important and accurate prognostic indices of patients with heart failure, shows the “maximal power output” of a subject, which is determined comprehensively by the reserve functions of the circulatory, respiratory, and the skeletal muscles [2].
When one mole of glucose is aerobically metabolized, a total of 6 moles of oxygen is used and 36 moles of Adenosine Triphosphate (ATP) is produced, namely:
C6H12O6+6O2+36ADP+36Pi→6CO2+42H2O+36ATP
ATP is called “currency of energy” which produces certain amount of energy (30.5 kJ/mol) when it is hydrolyzed to ADP. The proportional relationship addressed in this chemical formula tells us that measuring the amount of oxygen utilized in (or taken into) the body in a certain period (usually in a minute) is proportional to the amount of energy produced in the body during the period, i.e., measuring the work rate (power output) of the subject. Although we cannot measure the power produced by the body directly, we can measure it indirectly by measuring the amount of oxygen taken into the body in a certain period, i.e., the oxygen uptake (VO2). Therefore, measuring the maximal amount of oxygen one can take into the body in a certain period is nothing other than measuring the maximal energy output a person can produce.
With the Fick’s LAW, VO2 is described as:
VO2 = C.O.×(CaO2-CVO2) = C.O.×(CPV-CPA),
where C.O. is minute cardiac output, CaO2, CVO2, CPV and CPA, are oxygen content of the arterial, mixed venous, pulmonary venous, and pulmonary arterial blood. As C.O., CaO2 - CVO2, and CaO2 - CVO2 indicate the functions of the heart, efficiency of skeletal muscular oxygen utility, and oxygen intake function of the lungs, respectively, VO2max can be considered as an index of comprehensive reserves of cardiac, skeletal muscular, and respiratory functions. A normal value of VO2max for a normal, non-regularly exercising man is about 30- 40ml/min/kg, with slightly lower value in a woman.
Limitation of the VO2max
The VO2max is, however, only a “conceptual gold standard”. Maximal exercise is often difficult and sometimes dangerous because it may lead to myocardial ischemia [3,4]. We therefore have to compromise by using submaximal measurements. The most frequently used measurement is the peak VO2, the value at the end of incremental exercise testing. Other indices that do not need maximal exercise are anaerobic threshold (AT), the slope of the Minute Ventilation (VE)/ Carbon Dioxide Production (VCO2) regression, and the OUES.
AT and ventilatory threshold
Since the 1920s, the phenomenon of the rise in serum lactate concentration during strenuous exercise has been known, which is produced in the working skeletal muscles. In the 1960s, Wasserman and coworkers hypothesized that the production of lactate was associated with the ischemia of the muscles above a certain level of exercise intensity, and named the phenomenon as AT [5]. This hypothesis was persuasive and many a researchers and clinicians believed it. Then, researchers reported that the use of expired gas analysis during incremental exercise testing can detect the threshold non-invasively, and named it Ventilatory Threshold (VT). These studies have made the AT the mainstream of the exercise physiology and exercise cardiology during the 1980s and 1990s. However, studies afterwards have proved that
1) Any level of exercise intensity cannot cause ischemia of the skeletal muscle mitochondria which leads to anaerobic energy production [6],
2) Lactate is produced from the skeletal muscles at any level of exercise intensity [7-9],
3) The serum lactate levels are determined by the balance between its production and clearance [10,11], and
4) Therefore, there is not any “threshold” of the serum lactate levels [12,13]. These studies have led most researchers today to “abandon faith” for AT.
Although most researchers today believe that the AT theory that Wasserman advocated has been disproven, the AT is still widely used in our clinical practices. It is because AT represents the exercise intensity that is not too strenuous but not too mild. In fact, significant lactate accumulation in the blood does not occur under the exercise intensity below the AT levels. Also, cardiac ischemia hardly occurs below the AT levels, which often makes the AT level exercise intensity for cardiac rehabilitation. Also, the AT is still widely used in the practices of athletic training, as appropriate training can suppress the blood levels of lactate under the same exercise intensity. For example, Hurley and coauthors have shown that a 12-week exercise program elicited significantly lower lactate concentrations at the same relative exercise intensities of the 55–75% of VO2max after training [14].
Usually, AT (VT) can be determined by the CPET [15]. Most commonly, it is determined as the level of exercise intensity (or VO2) at which the Ventilatory Equivalent of the oxygen (VE/VO2) begins to increase during incremental exercise [15]. Also, the point at which the end-expiratory partial pressure of oxygen begins to increase [15], or the first point of departure from linearity of VCO2 plotted against VO2 [16].
The VE/VCO2 regression slope
The alveolar ventilation equation concisely addresses the relation among the minute Alveolar Ventilation (VA), VCO2, and the arterial partial Pressure of Carbon Dioxide (PaCO2), namely:
VA = 863×VCO2/PaCO2.
When we replace VA with a more easily measured parameter VE, this equation can be rewritten as:
VE = 863×VCO2/(PaCO2.×(1-Vd/Vt)),
where, Vd and Vt represent dead space ventilation and tidal volume, respectively.
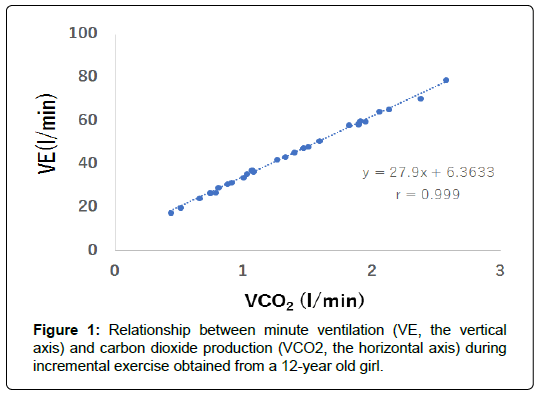
We can consider that VE is expressed as a linear equation of VCO2, as PaCO2, Vd and Vt are relatively stable during exercise. Actually, the relation between VE and VCO2 during incremental exercise testing shows linear just before maximal exercise until the respiratory compensation point (Figure 1). The slope of the regression equation shows the efficiency of ventilation during exercise. In patients with heart failure, pulmonary blood flow cannot distribute evenly to their alveoli, causing greater values of Vd, which leads to steeper linear relation between VE and VCO2. Therefore, the slope of the VE/VCO2 regression shows the ventilatory response to exercise. Also, there have been many studies that show the relation of the regression slope and the prognosis of patients with heart failure [17-19].
Oxygen uptake efficiency slope
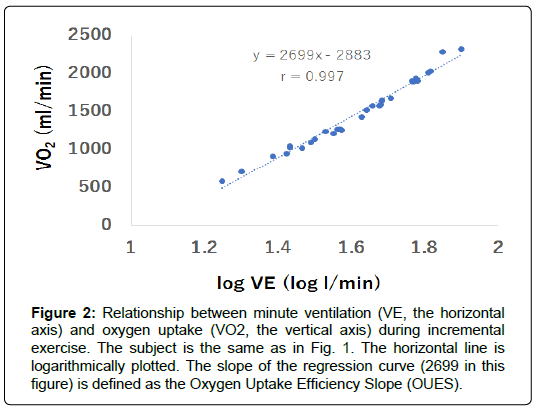
As shown in Figure 2 the relation between VO2 and VE during incremental exercise. Note that the x-axis is logarithmically plotted. Therefore, their relation can be described as:
Figure 2: Relationship between minute ventilation (VE, the horizontal axis) and oxygen uptake (VO2, the vertical axis) during incremental exercise. The subject is the same as in Fig. 1. The horizontal line is logarithmically plotted. The slope of the regression curve (2699 in this figure) is defined as the Oxygen Uptake Efficiency Slope (OUES).
VO2=a logVE+b
where a and b are constants.
The relation can be observed with high values of regression coefficients regardless of subjects and exercise protocol [20]. Differentiation of the both sides of the equation above by VE gives:
d VO2/dVE=a ln10/VE.
This equation shows that the increment of VO2 against VE is determined by VE and the constant a. Therefore, the constant a indicates the rate of the increase in VO2 at a certain minute ventilation VE. We have named the slope a the OUES [20]. The OUES is a measure of the ability to increase VO2 per 10-fold rise in minute ventilation. In other words, a steeper slope (or, a greater value of OUES) shows that the subject can take oxygen into the body without excessively increasing ventilation, i.e., without causing shortness of breath.
One of the most prominent features of OUES is that this index is strongly correlated with VO2max [20]. Baba et al. [20] have reported in 1996, using patients with a variety of pediatric cardiac diseases, that the regression coefficient was 0.941. The close correlation is also shown in various populations, e.g., healthy adults (r=0.966) [21], healthy children (r=0.920) [22], obese and non-obese children (r=0.91) [23,24], and adult patients with heart failure (r=0.78) [25].
Another feature of OUES is that this can be accurately calculated without imposing maximal exercise on subjects. As the OUES is defined as the slope of the logarithmic relation between VO2 and VE during incremental exercise, submaximal exercise data is theoretically sufficient for its calculation. In fact, Baba and coauthors have shown that calculation of the OUES with the first 90% and 75% of incremental exercise data are almost identical to measurements obtained from maximal data using populations of children [20], adults with heart failure [24], and healthy adults [21]. Also, Akkerman et al. [26] have shown, with a population of 46 children that the OUES values are consistent between those calculated with maximal and submaximal exercise data up to the AT. This strong point is clinically important in children who often cannot understand why they must perform “maximal” exercise testing, or in patients with cardiac diseases on whom imposing maximal exercise is dangerous.
OUES is now often used as prognostic indicators of cardiac patients. One of the most important studies would be one that Davies et al. [27] have published in the European Heart Journal in 2006. This study has analyzed the prognosis of 243 patients with heart failure using the measurements of OUES, peak VO2, VT, and the VE/VCO2 regression slope, and has shown that only OUES is the independent risk factor of death when multivariable model was used, with the cut-off value of 1.47 ml/min/log (l/min) [27]. Then, Arena et al. [28] have analyzed the prognosis of adult patients with heart failure, with the end-points of death, cardiac transplantation, or implantation of Ventricular Assist Device (VAD), and have shown that both the VE/ VCO2 regression slope and the OUES are independent risk factors, with the area under the curves (AUCs) of 0.73 and 0.74, respectively. Further, Myers et al. [29] using a large cohort of 2625 patients with heart failure, have shown that a scoring system with a combination of the OUES, the VE/VCO2 regression slope, the heart rate reserve, endexpiratory partial pressure of carbon dioxide (PetCO2), and peak VO2 is a strong prognostic marker of the patients. Recently, Coeckelberghs et al. [30] have shown that the OUES is an independent predictor for all-cause and cardiovascular mortality in patients with coronary artery disease, irrespective of a truly maximal effort during CPET. Also, Tang et al. [31] have shown that the OUES provides prognostic information for predicting clinical worsening and mortality in patients with idiopathic pulmonary hypertension.
The clinical applications of the OUES in pediatric populations have also been reported. Bongers et al. [32] have provided sex and age-related normative values for OUES which facilitates the interpretation of OUES in children. Hossri et al. [33] also have published reference values of OUES and concluded that OUES is a marker tool in the differentiation between preserved or abnormal functional capacity in children and adolescents with and without congenital heart disease, even at the submaximal level of exercise. Recently, several studies have shown the prognostic values of the OUES in patients with congenital heart diseases. Chen and coauthors have reported that submaximal exercise parameters including OUES provide superior prognostic information to maximal exercise data for predicting cardiac morbidity in Fontan patients [34]. Moreover, the association between the OUES and cardiac morbidity is independent of relevant baseline clinical information [34]. Also, Tsai et al. [35] have shown, using forty post-surgical patients with tetralogy of Fallot younger than 12 years old, that the OUES normalized by body surface area, as well as peak VO2, are useful predictors of cardiac-related hospitalization.
Conclusion
As the OUES is now considered as an excellent and useful parameter of exercise tolerance and gas exchange efficiency, many a guidelines and textbooks today describe it as an independent item. We expect future development and clinical applications of this parameter.
References
- Mudge GH, Goldstein S, Addonizo LJ, Caplan A, Mancini D, et al. (1993) 24th Bethesda Conference Taskforce 3: Heart transplantation: Recipient gidelines/prioritization. J Am Coll Cardiol 22: 21-31.
- Mancini DM, Eisen H, Kussmaul W, Mull R, Edmunds Jr LH, et al. (1991) Value of peak exercise oxygen consumption for optimal timing of cardiac transplantation in ambulatory patients with heart failure. Circulation 83: 778-786.
- Myers J, Walsh D, Buchanan N, Froelicher VF (1989) Can maximal cardiopulmonary capacity be recognized by a plateau in oxygen uptake? Chest 96: 1312-1316.
- Rowland TW, Cunningham LN (1992) Oxygen uptake plateau during maximal treadmill exercise in children. Chest 101: 485-489.
- Wasserman K, McIlroy MB (1964) Detecting the threshold of anaerobic metabolism in cardiac patients during exercise. Am J Cardiol 14: 844-852.
- Jöbsis FF, Stainsby WN (1968) Oxidation of NADH during contractions of circulated mammalian skeletal muscle. Respir Physiol 4: 292-300.
- Connett RJ, Gayeski TE, Honig CR (1984) Lactate accumulation in fully aerobic, working, dog gracilis muscle. Am J Physiol 246: H120-128.
- Hogan M.C (2001) Fall in intracellular PO2 at the onset of contractions in Xenopus single skeletal muscle fibers. J Appl Physiol 90: 1871-1876.
- Gladden LB (2000) Muscle as a consumer of lactate. Med Sci Sports Exerc 32: 764-771.
- Donovan CM, Pagliassotti MJ (2000) Quantitative assessment of pathways for lactate disposal in skeletal muscle fiber types. Med Sci Sports Exerc 32: 772-777.
- Brooks G.A (2000) Intra- and extra-cellular lactate shuttles. Med Sci Sports Exerc 32: 790-799.
- Myers J, Ashley E (1997) Dangerous curves. A perspective on exercise, lactate, and the anaerobic threshold. Chest 111: 787-795.
- Yeh MP, Gardner RM, Adams TD, Yanowitz FG, Crapo RO, et al. (1983) "Anaerobic threshold": problems of determination and validation. J Appl Physiol Respir Environ Exerc Physiol 55: 1178-1186
- Hurley BF, Hagberg JM, Allen WK, Seals DR, Young JC, et al. (1984) Effect of training on blood lactate levels during submaximal exercise. J Appl Physiol Respir Environ Exerc Physiol. 56: 1260-1264
- Wasserman K, Whipp BJ, Koyl SN, Beaver L (1973) Anaerobic threshold and respiratory gas exchange during exercise. J Appl Physiol 35: 236-243.
- Beaver WL, Wasserman K, Whipp BJ (1986) A new method for detecting anaerobic threshold by gas exchange. J Appl Physiol 60: 2020-2027.
- Chua TP, Ponikowski P, Harrington D, Anker SD, Webb-Peploe K, et al. (1997) Clinical correlates and prognostic significance of the ventilatory response to exercise in chronic heart failure. J Am Coll Cardiol 29: 1585-1590.
- Kleber FX, Vietzke G, Wernecke KD, Bauer U, Opitz C, et al. (2000) Impairment of ventilatory efficiency in heart failure: prognostic impact. Circulation 101: 2803-2809.
- Buller NP, Poole-Wilson PA (1990) Mechanism of the increased ventilatory response to exercise in patients with chronic heart failure. Br Heart J 63: 281-283.
- Baba R, Nagashima M, Goto M, Nagano Y, Yokota M, et al. (1996) Oxygen uptake efficiency slope: A new index of cardiorespiratory functional reserve derived from the relation between oxygen uptake and minute ventilation during incremental exercise. J Am Coll Cardiol 28: 1567-1572.
- Baba R, Nagashima M, Goto M, Nagano Y, Yokota M, et al. (1996) Oxygen intake efficiency slope: a new index of cardiorespiratory functional reserve derived from the relationship between oxygen consumption and minute ventilation during incremental exercise. Nagoya J Med Sci 59: 55-62.
- Marinov B, Mandadzhieva S, Kostianev S (2007) Oxygen uptake efficiency slope in healthy 7 to 18 years old children. Pediatr Exerc Sci 19: 159-170.
- Marinov B, Kostianev S (2003) Exercise performance and oxygen uptake efficiency slope in obese children performing standardized exercise. Acta Physiol Pharmacol Bulg 27: 59-64.
- Drinkard B, Roberts MD, Ranzenhofer LM, Han JC, Yanoff LB, et al. (2007) Oxygen-uptake efficiency slope as a determinant of fitness in overweight adolescents. Med Sci Sports Exerc 39: 1811-1816.
- Baba R, Tsuyuki K, Kimura Y, Ninomiya K, Aihara M, et al. (1999) Oxygen uptake efficiency slope as a useful measure of cardiorespiratory functional reserve in adult cardiac patients. Eur J Appl Physiol Occup Physiol 80: 397-401.
- Akkerman M, Brussel M, Bongers BC, Hulzebos EH, Helders JM, et al. (2010) Oxygen uptake efficiency slope in healthy children. Pediatr Exerc Sci 22: 431-441
- Davies LC, Wensel R, Georgiadou P, Cicoira M, Coats JS, et al. (2006) Enhanced prognostic value from cardiopulmonary exercise testing in chronic heart failure by non-linear analysis: oxygen uptake efficiency slope. Eur Heart J 27: 684-690.
- Arena R, Myers J, Abella J, Pinkstaff S, Brubaker P, et al (2010) Prognostic significance of the oxygen uptake efficiency slope: percentpredicted versus actual value. Am J Cardiol 105: 757-758.
- Myers J, Oliveira R, Dewey F, Arena R, Guazzi M,et al. (2013) Validation of a cardiopulmonary exercise test score in heart failure. Circ Heart Fail 6: 211-218.
- Coeckelberghs E, Buys R, Goetschalckx K, Cornelissen A, Vanhees L, et al. (2016) Prognostic value of the oxygen uptake efficiency slope and other exercise variables in patients with coronary artery disease. Eur J Prevent Cardiol 23: 237-244.
- Tang Y, Luo Q, Liu Z, Ma X, Zhao Z, et al. (2017) Oxygen uptake efficiency slope predicts poor outcome in patients with idiopathic pulmonary arterial hypertension. J Am Heart Assoc 30: e005037.
- Bongers BC, Hulzebos EH, Helbing WA, Harkel AD, Brussel MV, et al. (2016) Response profiles of oxygen uptake efficiency during exercise in healthy children. Eur J Prevent Cardiol 23: 865-873.
- Hossri CA, Souza IPAD, Oliveira JS, Mastrocola LE (2019) Assessment of oxygen-uptake efficiency slope in healthy children and children with heart disease: generation of appropriate reference values for the OUES variable. Eur J Prevent Cardiol 26: 177-184.
- Chen CA, Chen SY, Chiu HH, Wang JK, Chang CI, et al. (2014) Prognostic value of submaximal exercise data for cardiac morbidity in Fontan patients. Med Sci Sports Exerc 46: 10-15.
- Tsai YJ, Li MH, Tsai WJ, Tuan SH, Liao TY, et al. (2016) Oxygen uptake efficiency slope and peak oxygen consumption predict prognosis in children with tetralogy of Fallot. Eur J Prev Cardiol 23: 1045-1050.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi