Short Communication, Int J Cardiovasc Res Vol: 8 Issue: 3
Comparison of Cardio Vascular Magnetic Resonance Imaging (MRI) and Positron Emission Tomography (PET) for Detection of Myocardial Viability
Reena Anand*, Nikhil Gupta and Bharat Aggarwal
Max Super Speciality Hospital, Saket, New Delhi, India
*Corresponding Author: Reena Anand
Max Super Speciality Hospital, Saket, New Delhi, India
Tel: 9650300500
E-mail: destinationreena@gmail.com
Received: March 13, 2019 Accepted: March 26, 2019 Published: April 05, 2019
Citation: Anand R, Gupta N, Aggarwal B (2019) Comparison of Cardio Vascular Magnetic Resonance Imaging (MRI) and Positron Emission Tomography (Pet) for Detection of Myocardial Viability. Int J Cardiovasc Res 8:3. doi: 10.4172/2324-8602.1000378
Abstract
Coronary artery disease (CAD) remains the most common cause of death. However, the number of deaths from myocardial infarction has decreased. Mortality from congestive heart failure has more than doubled. It is important to note that CAD accounts for the majority (almost 70%) of congestive heart failure cases.
In the clinical management of patients with symptom of heart condition by CAD, the correct assessment of cardiac muscle viability is crucial to guide treatment and this will be as a result of revascularization of dysfunctional however viable heart muscle can improve cavity perform and future survival.
Generally nuclear imaging, stress echocardiography and stress electrocardiography have been the clinical main step for assessing myocardial viability as well as to detect myocardial Ischemia.
Recently cardiovascular MR (CMR) is a rapidly emerging non-invasive imaging technique, providing high resolution images of the heart in any desired plane and without radiation. CMR has the unique ability to evaluate several markers of myocardial viability that are of proven value. The focus of the present study is on the rapidly emerging clinical role of cardiovascular MRI in the detection of viable myocardium.
Objective: To assess the role of cardiovascular MRI for detection of myocardial viability
Keywords: Magnetic resonance imaging; Positron emission tomography; Myocardial infarction; Coronary artery disease; Myocardium; Ventricular dysfunction
Background and Rationale
Ischemic coronary illness related mortality has been on the decline stage, in spite of the fact that its pervasiveness has been on the ascent since the late 1970s. One of the contributing elements to this decay has been improved determination and restorative administration. Each clinician looks to respond to two key inquiries while assessing patients with suspected or known IHD: What is the worldwide ventricular capacity? Is the myocardium practical? A PET is the pillar of finding of myocardial practicality. In the previous decade cardiovascular attractive reverberation (CMR) imaging has risen as a critical clinical strategy with the capability of responding to all the appropriate inquiries in a solitary report [1-4]. Direct imaging of myocardial fibrosis is currently conceivable with the utilization of a reversal recuperation arranged T1, weighted slope reverberation grouping after the intravenous organization of a gadolinium-Chelate (Gad). The CMR technique has been named delayed-enhancement (DE-MRI) and demonstrate nonviable tissue as “hyper enhanced” or bright [5,6].
The DE-MRI technique is rapidly assuming a prominent role in the assessment of viability, as it has the advantages of being performed under resting condition and with no exposure to radiation.
Klein et al. discovered that the territory complexity improvement is estimated by CECMR correlated closely with myocardial infarcts defined by PET in patients with Ischemic cardiomyopathy [7].
Kuhl et al. compared F-18 fluorodeoxyglucose (FDG) PET and CECMR in 26 patients. The study showed that segmental glucose uptake by PET is inversely correlated with the segmental extent of contrast enhancement and that using a cut off value of 37% segmented enhancement, optimally differentiated viable from non-viable segment defined by PET, using PET as the gold standard, this resulted in a sensitivity and specificity of CECMR for detection of viable myocardium of 96% and 84% respectively [8].
Because of its superior spatial resolution, CMR has the unique ability to assess small infarcts and to measure the trans mural extent of myocardial infarction [9,10]. This advantage has been used to detect micro-infants associated with successful coronary angioplasty, as well as the detection of sub endocardial infarcts which are missed by SPECT.
Methods
It was a prospective observational study. Patients who had undergone cardiac PET underwent cine MRI for ventricular motion abnormality. Then rest perfusion study was performed with 5 ml IV contrast *Omniscan where perfusion defect was detected to rule out ischemia. It was followed by late gadolinium enhancement where contrast media omniscan was given with dose of 0.1 mmole/kg body weight and a wait of 10 minutes is required to acquire delayed imaging for detection of scar The study was conducted at Max Super Specialty hospital (a unit of Max Healthcare institute limited) in the department of Radiology. The duration of the study was approx. 14 months. Around 27 subjects recruited for the study were undergone MRI. The procedure for MRI was around 1 hr.
*Currently, gadolinium enhanced MRI of the heart is off-label use for all approved GBCAs.
Image analysis
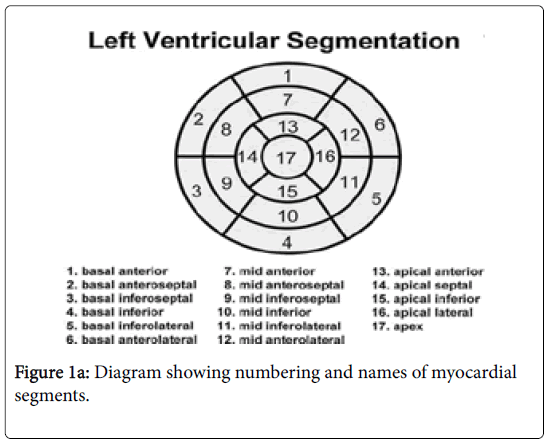
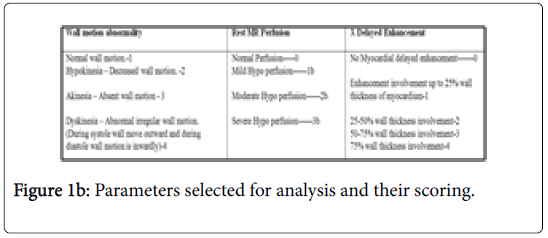
Image analysis was done on GE MRI work station by experienced radiologist blinded to PET finding. 17 myocardial segments of heart (Figure 1a) were assessed and analysis of three parameters for these particular segments were selected and done with the following protocol (Figure 1b). All Cardiac PET and MRI finding were compared and retrospective analyses were done to correlate both modalities.
Selection and enrollment of participants
The patients were recruited based upon the inclusion and exclusion criteria. The subject were enrolled after voluntary consent was taken. A total of 27subjects were recruited.
Inclusion criteria:
• Age>45 years, male or female
• Indication - Patients who have undergone cardiac PET and showed positive result
• Renal function Test clearance. E.g. Creatinine, Urea, GFR
Ejection fraction
Patient who have ejection fraction ranging from<45%.
Exclusion criteria
Reason for ineligibility:
• Claustrophobic patients (Patient who can’t lie down in MRI Scanner)
• High Creatinine/low GFR patients.
• Abnormal value of creatinine ->1.4
• Abnormal eGFR-<50
List of excluded drugs/eatable. With use of adenosine while doing CMR the list of drugs/eatables which can be avoided:
• Contra-indication
• Acute myocardial infarction within few days
• Asthma
• Second or third degree Atrio-ventricular block
• Sick sinus syndrome
• Symptomatic bradycardia
Study enrollment procedure
Patient who fulfilled all the inclusion and none of exclusion criteria and willing to give voluntary informed consent to participate in the study were enrolled in the study. Prior to first recruitment of subject into the study Institutional Ethics Committee approval were taken of the site.
Ethical consideration
This project was carried out according to ethical guidelines for biomedical research on human participants, Indian council of medical research, Indian good clinical practice guidelines and Declaration of Helsinki 2013. This statement had been developed to protect the interests of people who agree to participate in human research studies.
Informed consent forms
The consent forms were prepared by the research team after explanation of the purpose, risks and benefits of the study. For subjects who cannot read and write English, a consent form is prepared in Hindi.
Participant confidentiality
Any data, forms reports, video recordings and other records that leave the site were identified only by a participant identification number (Participant ID) to maintain confidentiality. All records were kept in a locked file cabinet. All computer entry and networking programs were done using PIDs only. Information were not released without written permission of the participant, except as necessary for monitoring by Institutional ethics committee (IEC) of the site and any regulatory authority.
Statistical Analysis
Agreement between PET and MR findings was evaluated separately for each segment for perfusion, viability and motion. Agreement in terms of percentage and cohen kappa wwere calculated for statistical significance. SPSS was used for calculations.
Results
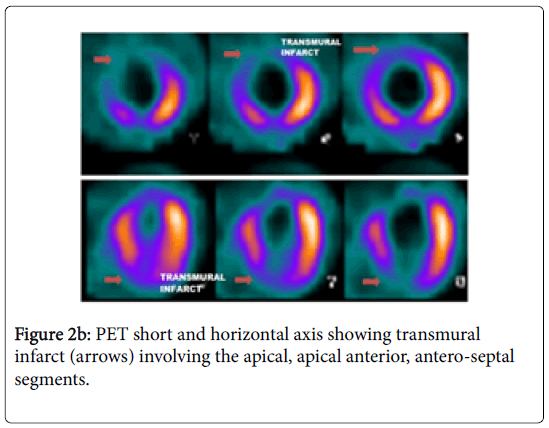
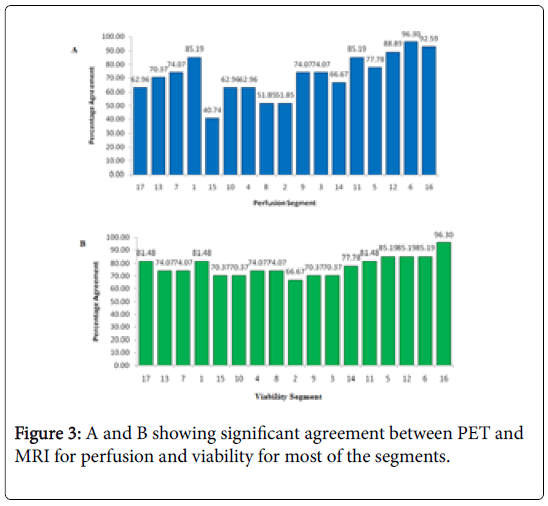
CMR and PET data of all 27 patients were done for the evaluation and 459 segments were compared in total. In our study we got significant agreement between PET and MRI for perfusion and viability (Figures 2a and 2b) for most of the segments (-75-80%) (Figures 3a and 3b). CMR found more scar/fibrosis than PET in subjects with EF<35%. CMR revealed less scars than PET in subjects with EF>40%. There was no significant agreement noted between PET and MRI for myocardial motion.
Discussion
It has been shown that patients with chronic ventricular dysfunction and CAD have poor long term survival. Identification of such patients who may benefit from revascularization procedures is the major goal to improve outcomes. Several viability studies have estimated the long term prognosis as a final endpoint and concluded that viable myocardium was related to the improvement in myocardium function. Magnetic resonance is able to assess myocardial viability through a number of different techniques and methods. These techniques can assess metabolic, functional and morphological changes and tissue properties as well as cellular viability. The most widely used and with the greatest clinical application potential is delayed myocardial amplification. This technique is able to easily and objectively identify areas of the hyperintensive signal in the myocardium after administration of the contrast agent, with excellent histological correlation to characterize areas with myocardial infarction/fibrosis.
Conclusion
Magnetic resonance is able to assess myocardial viability through a number of different techniques and procedures and methods. These techniques can assess metabolic, functional, and morphological alterations and tissue characteristics, in addition to evaluating cellular viability. Moreover MRI costs less and has easy availability as compared to PET CT.
Limitation
As our sample size was small further studies including larger patient cohorts undergoing viability imaging are required for further evaluation.
Grants
This study has been supported by an unrestricted grant from GE Healthcare.
References
- Shan K, Constantine G, Sivananthan M, Flamm SD (2004) Role of cardiac magnetic resonance imaging in the assessment of myocardial viability. Circulation 109: 1328-1334.
- Mahrholdt H, Klem I, Sechtem U (2007) Cardio vascular MRI for detection of myocardial viability and ischemia. Heart 93: 122-129.
- Raj V, Agrawal SK (2010) Ischemic heart disease assessment by cardiovascular magnetic resonance imaging. Postgrad Med J 86: 532-540.
- Kim RJ, Wu E, Rafael A, Chen EL, Parker MA, et al. (2000) The use of contrast-enhanced magnetic resonance imaging to identify reversible myocardial dysfunction. N Engl J Med 343: 1445-1453.
- Kwong RY, Sattar H, Wu H, Vorobiof G, Gandla V, et al. (2008) Incidence and prognostic implication of unrecognized myocardial scar characterized by cardiac magnetic resonance in diabetic patients without clinical evidence of myocardial infarction. Circulation 118: 1011-1020.
- Arai AE (2011) The cardiac magnetic resonance (CMR) approach to assessing myocardial viability. J Nucl Cardiol 18: 1095-1102.
- Bettencourt N, Chiribiri A, Schuster A, Nagel E (2009) Assessment of myocardial ischemia and viability using cardiac magnetic resonance. Curr Heart Fail Rep 6: 142-153.
- Kühl H P, Beek A M, van der Weerdt A P. et al (2003) Myocardial viability in chronic ischemic heart disease: comparison of contrastâ€Âenhanced magnetic resonance imaging with (18)Ffluorodeoxyglucose positron emission tomography. J Am Coll Cardiol 41: 1341–1348.
- Bettencourt N, Chiribiri A, Schuster A, Nagel E (2009) Assessment of myocardial ischemia and viability using cardiac magnetic resonance. Curr Heart Fail Rep 6: 142-153.
- Weinsaft JW, Klem I, Judd RM (2007) MRI for the assessment of myocardial viability. Cardiol Clin 25: 35-56.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi