Research Article, Int J Cardiovasc Res Vol: 9 Issue: 7
Conscious Sedation with Local Anesthesia Versus General Anesthesia for Patients Undergoing Transcatheter Aortic Valve Implantation: A Randomized Controlled Trial
Omar S.M. Abdel-Hafez, Ayman M Kamaly, Eman M.K. Abo-Seif and Amr M Hilal Abdou*
Department of Anesthesia, Intensive Care and Pain Management, Ain Shams University, Cairo, Egypt
*Corresponding Author:Dr. Amr M Hilal Abdou Department of Anesthesia, Intensive Care, and Pain Management Ain Shams University, Cairo, Egypt Tel: 01001479037 E-mail: amr_hilal@med.asu.edu.eg.
Received: October 09, 2020 Accepted: November 09, 2020 Published: November 16, 2020
Citation: Abdel-Hafez OSM, Kamaly AM, Abo-Seif EMK, Abdou AMH (2020) Conscious Sedation with Local Anesthesia Versus General Anesthesia for Patients Undergoing Transcatheter Aortic Valve Implantation: A Randomized Controlled Trial. Int J Cardiovasc Res 9:7.
Abstract
Objectives: Transcatheter Aortic Valve Implantation (TAVI) procedure is usually performed under General Anesthesia (GA), Conscious Sedation Associated with Local Anesthesia (CSLA) or local anesthesia alone. There have been limited studies to determine which plan of anesthesia is associated with better results. The aim of the study is to assess the role of CSLA in outcome, complications, mortality, and quality of life in immediate post-procedural period (ICU and hospital stay). Design: Participants: Seventy cases of moderate to severe aortic stenosis planned for TAVI were randomized into two groups. Interventions: Group-GA: received general anesthesia and Group- CSLA: received conscious sedation combined with local anesthesia. Measurements: We recorded the intraoperative hemodynamic changes, pH, PaO2, PaCO2, need for inotropic support and need for blood products. Post-operative measurements included the need of inotropic support, prolonged respiratory support, renal dialysis, and incidence of stroke, heart block, aortic regurge as well as mortality. Results: The CSLA group showed more incidence of respiratory acidosis manifested by the increase of PaCO2 (p=0.024), less decrease in mean arterial blood pressure (p=0.028), less need for inotropic support in both intraoperative (p=0.001) and post-operative period (p=0.005). The CSLA patients showed less hospital Length of Stay (LOS) (p=0.006) and less prolonged respiratory support more than 24h (p=0.001) compared to the GA group patients. However, there was no significant difference regarding the blood products consumption (p=0.587) and incidence of complications. Conclusion: The current study showed better intraoperative hemodynamic stability, less need for Perioperative inotropic support and less hospital stay despite the presence of mild acceptable respiratory acidosis in patients receiving CSLA for TAVI procedure.
Keywords: Aortic; Sedative, Minimal; Invasive
Keywords
Aortic; Sedative, Minimal; Invasive
Introduction
The field of interventional cardiology is becoming more developed and complex, the number of cardiac diseases being managed by interventional cardiology is increasing by time. Cardiologists have gained more experience in the field of interventional procedures for treatment of structural cardiac pathologies limiting the role of openheart surgeries. The idea of interventional cardiology replacing open heart surgery is a very attractive thought for further research, being much less invasive, especially after the success of transcutaneous closure of some forms of congenital heart diseases such as Atrial Septal Defect (ASD), Ventricular Septal Defect (VSD) and Patent Ductus Arteriosus (PDA), and also the success of Mitral Clipping as a treatment for Mitral Regurgitation, turning an open heart surgery into a sort of a day case surgery [1].
The invention of TAVI as an alternative to open aortic valve replacement got worldwide acceptance and interest, especially that many of the patients are old enough with severe aortic stenosis associated with multiple comorbidities and who are considered high risk for open heart surgery [2]. After many years of trials in animals, the first-in-man TAVI procedure was performed in Rouen on April 16th, 2002. Since then tens of thousands of procedures were successfully performed worldwide [3]. The first procedure done in Egypt was in 2011 [4].
Interventional cardiology offers the chance for several anesthetic plans to be performed. For TAVI cases we are given the chance to perform CSLA [5] or Local Anesthesia alone (LA) [6] rather than General Anesthesia (GA). Much research has been done to compare the outcomes of both plans of anesthesia to prove that CSLA is safer, and to measure the extent of its safety compared to GA. Some evidence showed that CSLA provide better outcomes [7,8] and some references showed no difference [9].
In our center at Ain Shams University; Cardiothoracic and interventional cardiology unit, A center with high volume of Aortic diseases; TAVI procedure is getting more popularity and interest for all the physicians working in that field. The choice of the anesthetic technique varies among institutions. It is recommended that GA be the preferred anesthetic technique in low-volume institutions and/or until institutions gain experience [10], this recommendation is based on the regular use of trans-esophageal echocardiography during the procedure in addition to the lengthy procedure rendering CSLA a not feasible method for growing institutions.
In the current study, we compared the difference between CSLA and GA on post procedural outcomes of patients undergoing TAVI, to improve success, outcomes and quality of life among patients suffering from aortic valve disease, to assess the role of CSLA in improving outcome and minimizing complications, improving mortality rates and to assess quality of life in immediate postprocedural period (ICU and hospital stay). This hypothesis needed to be investigated, that’s why this study and other similar studies were done. Also, the incidence for more than mild paravalvular aortic regurge was measured; regurge is expected in CSLA because TEE use in a conscious patient is difficult.
Methods
After approval of the Ethical Committee of Ain Shams University with FWA 000017585, FMASU MD 247/2017 according to the declaration of Helsinki, we enrolled 70 patients of both sexes, above 40 years old, diagnosed with aortic disease candidates for TAVI.
This interventional clinical trial study was performed at Ain Shams University Hospitals registered with number 247/2017. Patients suffering from uncooperative mental illness and patients suffering from severe respiratory disease rendering the use of sedatives and analgesics too risky were excluded.
Patients were admitted to hospital the night before the procedure. Demographic and vital data were collected and EUROSCORE II (for assessment of surgical cardiac patients) were calculated for each patient, preoperative full labs, ECG and transthoracic echocardiography, with the optimization of blood pressure, Heart Rate (HR). Chest condition and body temperature should be stable prior to intervention.
Intraopertively all patients received a wide bore venous cannula, an invasive arterial cannula for monitoring and sampling, a Central Venous Line (CVL) under local anesthesia and a urinary catheter.
The patients were randomized into the GA group that received conventional general anesthesia using fentanyl (2-3 μg/kg), Midazolam (50-100 μg/kg), Propofol (0.5 mg/kg) and maintenance inhalational anesthesia (Sevoflurane) on 0.5 MAC and muscle relaxation (atracurium) with endotracheal intubation and mechanical ventilation and extubated in the Cath. Lab. or shortly after transfer to CCU, and the CSLA group received anxiolysis with a Midazolam (10-30 μg/kg) and maintenance on fentanyl infusion (1-2 μg/kg/h) and Propofol infusion (0.5-2 mg/kg/h) with O2 supplementation via face mask on 8-10 L/m connected to the end-tidal CO2 sample line. The depth of anesthesia was not monitored; assessment of the level of sedation was done on clinical basis of the level of consciousness, frequent communication with the patient, respiratory pattern (presence of airway obstruction) and heart rate. Radial artery cannulation, CVL insertion and femoral puncture were done under local anesthesia infiltration. Intraoperative data to be collected were: hemodynamic measurements represented in Mean Arterial Blood Pressure (MAP) and HR collected before induction (time 0), just after induction (time 1), one hour after the start of the procedure (time 2), two hours after the start of the procedure (time 3) and before transfer (time 4), arterial Blood Gases (pH, PaCO2, PaO2 and SpO2) collected three times before induction (time 0), during the procedure (time 1) and before transfer (time 2); and intraoperative need for inotropic support. As shown in Table 1 the illustration to the inotropic and vasopressive support given. After the procedure we recorded the need for inotropic support, prolonged respiratory support (>24h), renal dialysis, cerebro-vascular accidents, Length of Hospital Stay (LOS), number of units of blood products needed, mortality rate.
| Epinephrine | <50 ng→1 |
| 50-100 ng→2 | |
| 100–150 ng→3 | |
| >150 ng→4 | |
| Norepinephrine | <50 ng→1 |
| 50 -100 ng→2 | |
| 100 – 150 ng→3 | |
| >150 ng→4 | |
| Dobutamine | <5 μg→1 |
| 5-10 μg→2 | |
| 10–15 μg→3 | |
| >15 μg→4 | |
| Milrionone | 0.3 µg →1 |
| 0.3-0.5 µg→2 | |
| >0.5 µg→3 |
Table 1: Inotropic support score.
The TAVI procedure
The procedure is done after coronary angiography and excluding coronary lesions that might affect the flow, if a lesion is diagnosed the procedure is cancelled, access route for TAVI is trans-femoral approach. Deployment of the valve (Sapien 3® or Evolut R®) after mapping of the position of the aortic valve and ventricular pacing of 16-200 beats per minute, optimization of the hemodynamic parameters.
Study Endpoints
Our study endpoints were shifting to GA during the procedure, length of hospital stay (LOS), in-patient mortality.
Statistical Analysis: Sample size was calculated using PASS version 11 program setting the type 1 error (alpha) at 0.05 and the power (1- ß) at 0.8 results from previous study [11] showed that the mean postoperative hospital stay in GA was 5.7±2.5 while for patients in CSLA group it was 6.3± 3.5 based on this and as non-inferiority study a sample size of 32 patients will be needed in each group. Data were processed and analyzed using SPSS (Statistical Package for Social Science) software version 20.0. Descriptive statistics was performed using means and standard deviations for quantitative variables, and frequencies and proportions for categorical variables. Differences between-group comparisons were performed using t-test for two independent samples or, the equivalent non-parametric, Mann-Whitney U test. For all tests, the level of significance was set at p-value≤0.05.
Results
We enrolled seventy patients candidates for TAVI, 37 patients received CSLA 5 (7.4%) patients converted to GA and were excluded from the study, the remaining 33 patients received GA, their demographic data described all patients had EUROSCORE II less than 20%) (Table 2). No reported cases of awareness during general anesthesia.
| CSLA (n= 32) | GA (n= 33) | p | sig | |
|---|---|---|---|---|
| EUROSCORE II (SD) | 3.34 ± 1.99 | 7.6 ± 13.31 | 0.078‡ | NS |
| Age (SD) | 73.6 ± 8.4 | 73.0 ± 8.0 | 0.80‡ | NS |
| Gender: male | 19 (59.3%) | 18 (54.5%) | 0.69* | NS |
| Weight (SD) | 88.4 ± 23.4 | 72.7 ± 17.4 | 0.003‡ | HS |
| Creatinine (SD) | 1.1 ± 0.34 | 1.4 ± 0.8 | 0.039‡ | S |
| Creatinine Clearance (SD) | 70 ± 32.5 | 59 ± 28.1 | 0.03‡ | S |
| On dialysis | 0 | 3 (9.1%) | 0.23† | NS |
| Extracardiac arteriopathy | 0 | 2 (6.1%) | 0.49† | NS |
| Poor mobility | 8 (25%) | 9 (27.3%) | 0.83* | NS |
| Previous cardiac surgery | 2 (6%) | 2 (6.1%) | 0.97† | NS |
| Chronic lung disease | 16 (50%) | 8 (24.2%) | 0.03* | S |
| Active endocarditis | 0 | 0 | ---- | |
| Critical state on inotropes | 0 | 4 (12.1%) | 0.11† | NS |
| Diabetes on insulin | 6 (18.8%) | 5 (15.2%) | 0.69* | NS |
| EF (SD) | 62% ± 7.9 | 54% ± 12.6 | 0.02‡ | S |
| Angina at rest | 0 | 2 (6.1%) | 0.49† | NS |
| Recent MI | 3 (9.4%) | 2 (6.1%) | 0.67† | NS |
| Pulmonary Hypertension | 7 (21.9%) | 14 (42.4%) | 0.07* | NS |
| Urgency | 0 | 4 (12.1%) | 0.114† | NS |
| Hypertension | 17 (53.1%) | 18 (54.5%) | 0.9* | NS |
| Liver disease | 3 (9.4%) | 3 (9.1%) | 1.0† | NS |
| Neurological disease | 3 (9.4%) | 4 (12.1%) | 1.0† | NS |
*Chi square test, †Fisher's Exact Test, ‡Student t test, HS=Highly Significant, S=Significant, NS=Nonsignificant.
Table 2: Description of preoperative conditions of patients in both groups, represented as number and percentage.
There was a significant difference between the CSLA and the GA groups as regard intraoperative MAP, pH and PaCO2 (Table 3) (P=0.28, 0.024, 0.005).
| Group | p |
sig |
|||||
|---|---|---|---|---|---|---|---|
| CSLA | GA | ||||||
| N | % | N | % | ||||
| Mean arterial blood pressure | <20% change | 24 | 75.00% | 16 | 48.50% | .028* | S |
| >20% change | 8 | 25.00% | 17 | 51.50% | |||
| Heart rate | <20% change | 32 | 100.00% | 31 | 93.90% | .492† | NS |
| >20% change | 0 | 0.00% | 2 | 6.10% | |||
| pH | <20% change | 27 | 84.40% | 33 | 100.00% | .024† | S |
| >20% change | 5 | 15.60% | 0 | 0.00% | |||
| PaCO2 | <20% change | 25 | 78.10% | 33 | 100.00% | .005† | HS |
| >20% change | 7 | 21.90% | 0 | 0.00% | |||
| PaO2 | <20% change | 30 | 93.80% | 28 | 84.80% | .427† | NS |
| >20% change | 2 | 6.30% | 5 | 15.20% | |||
*Chi-Square Tests, †Fisher's Exact Test, HS = Highly Significant, S =Significant, NS = Nonsignificant.
Table 3: Intraoperative vital data and arterial blood gases.
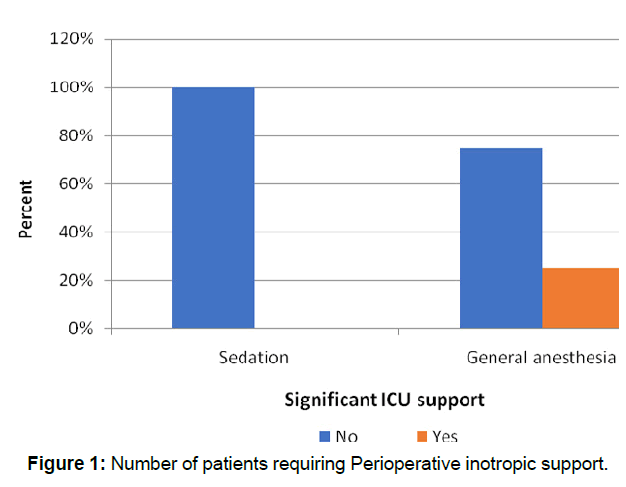
Perioperative inotropic support (Table 4 and Figure 1) was more significant among the GA; we measured the dose at two different stages, during the procedure (Pt=0.001) and during ICU stay (P=0.005) according to the inotropic scoring provided in Table 1.
| Group | p |
Sig |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CSLA | GA | |||||||||||
| Mean | ±SD | Median | IQR | Mean | ±SD | Median | IQR | |||||
| Intra operative Inotropic support | 0.31 | 0.59 | 0 | 0 | 0 | 1.91 | 2 | 1 | 0 | 4 | 0.001* | HS |
| ICU Inotropic support | 0.22 | 0.61 | 0 | 0 | 0 | 1.5 | 2 | 1 | 0 | 2.5 | 0.001* | HS |
*Mann-Whitney Test, HS = Highly Significant.
Table 4: Peri-opertive inotropic support.
Among CSLA group, only 9.4% of cases had respiratory support. The mean ICU respiratory support duration was 56 hours ±34.6 with a median of 36 h. And among the GA group, about 53% of the cases had respiratory support. The mean ICU respiratory support duration was 48.8 hours ±23.0 with a median of 36 h, with significant difference in favor to CSLA (P=0.001) (Table 5).
| Group | p |
Sig |
|||||
|---|---|---|---|---|---|---|---|
| CSLA | GA | ||||||
| Mean | ±SD | Mean | ±SD | ||||
| Respiratory support | No | 29 | 90.60% | 15 | 46.90% | 0.001* | HS |
| Yes | 3 | 9.40% | 17 | 53.10% | |||
*Chi-Square Tests, HS = Highly Significant.
Table 5: Need for respirtory support in the form of ventiltion (invsive or Non-invsive).
The mean hospital stay duration in CSLA was 5.5 days ± 6.37 with a median of 4 days and 6.2 ± 2.6 days among the GA group with median 6 (P=0.006).Only 12.4% of the CSLA cases received more than 2 blood units and 6.3% of the GA cases received more than 2 blood units (P=0.587) (Table 6).
Group |
p |
sig |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
CSLA |
GA |
||||||||||||
| Mean | ±SD | Median | IQR | Mean | ±SD | Median | IQR | ||||||
| Hospital LOS | 5.53 | 6.37 | 4 | 3 | 5 | 6.22 | 2.61 | 6 | 4 | 7 | 0.006* | HS | |
| No of units of blood products | 0.84 | 1.3 | 0 | 0 | 1 | 0.63 | 0.98 | 0 | 0 | 1 | 0.587* | NS | |
| No of units of blood | No | 19 | 59.40% | 21 | 65.60% | ||||||||
| 1-2 unit | 9 | 28.10% | 9 | 28.10% | |||||||||
| >2 unit | 4 | 12.50% | 2 | 6.30% | |||||||||
*Mann-Whitney Test, †Fisher exact Test, HS = Highly Significant, NS = Non significant.
Table 6: Hospitl Length of Sty (LOS).
Post procedure complications (Table 7) showed CSLA group; 22% of the cases had heart block, no mortality recorded. 37.5% had mild aortic regurge. Among the GA group, 13% had renal dialysis, 19% of cases had heart block, and 9.1% of cases died. 6.1% had moderate AR, 48.5% had mild AR.
| Group | p | sig | |||||
|---|---|---|---|---|---|---|---|
| CSLA | GA | ||||||
| N | % | N | % | ||||
| Renal dialysis | No | 32 | 100.00% | 28 | 87.50% | 0.113† | NS |
| Yes | 0 | 0.00% | 4 | 12.50% | |||
| Cerebrovascular accidents | No | 32 | 100.00% | 32 | 100.00% | ---- - |
---- |
| Yes | 0 | 0.00% | 0 | 0.00% | |||
| Heart Block | No | 25 | 78.10% | 26 | 81.30% | 0.756* | NS |
| Yes | 7 | 21.90% | 6 | 18.80% | |||
| Aortic Regurge | No | 20 | 62.50% | 15 | 45.50% | 0.168* | NS |
| Yes | 12 | 37.50% | 18 | 54.50% | |||
| Mild | 12 | 37.50% | 16 | 48.50% | 0.193† | NS | |
| Moderate | 0 | 0.00% | 2 | 6.10% | |||
| Severe | 0 | 0.00% | 0 | 0.00% | |||
| Outcome | Discharged | 32 | 100.00% | 30 | 90.90% | 0.238† | NS |
| Died | 0 | 0.00% | 3 | 9.10% | |||
*Chi-Square Tests, †Fisher's Exact Test, NS = Nonsignificant
Table 7: Post-opertive complictions nd outcome.
Discussion
The current study illustrates our center’s experience with the conscious sedation in TAVI procedures. Limited resources proved the efficacy and safety of CSLA in TAVI. We proved that this procedure could be done with CSLA leading to decrease in the hospital stay, lower mortality rate and post-operative complications compared to patients under GA. These results were associated with lower inotropic and respiratory support during the post-procedural period.
To date the largest meta-analysis was done by Villablanca et al. [8] included 10,572 patients from 26 studies [8], this meta-analysis showed significant advantage of CSLA. The use of CSLA was associated with a decrease in 30-day mortality (p=0.01), hospital LOS (p<0.001) and use of vasopressors/inotropes (p< 0.001). Other studies [11,12] reported also that patient selection for CSLA was more biased towards less risky cases and that generally in most institutions, there is a tendency at the beginning of the learning curve to go for the more familiar GA, these results were consistent with our study apart from the mortality which showed more number (9.1%) in the GA group and (0%) in the CSLA no statistical difference may be due to our single center study and smaller sample size.
Safety recordings is the most crucial point in our study; there was highly significant difference in PaCO2 in which CSLA group showed higher levels (p=0.005), which is expected due to the higher prevalence of chronic lung disease within the CSLA group and due to the hypoventilation caused by the sedatives, the sedatives that inhibit the respiratory center and inhibit the reflex tachypnea caused by hypoxia and hypercapnea. This hypercapnea is expected and tolerated if the rise is not severe and with experience it can be avoided by careful titration of sedation and meticulous monitoring of the patient. The decision to go for CSLA for patients with chronic lung disease is expected because of fear to worsen the lung disease by intubation and ventilation during GA, intraoperative MAP was lower>20% (p=0.028). In the GA group reflected by the more increased use of inotropes. The explanation of this event is definitely the Vasodilatory and negative inotropic effect of general anesthetics. These safety measures recording was supported by several studies [13,14].
LOS was reduced in CSLA group (P=0.006), which is debatable in most of the literature as some studies conclude that there is less LOS while other studies conclude that there is no difference. Examples of those who conclude that there is less LOS are: Villablanca P et al. [8] (p < 0.001), Maas et al. [9] (a systematic review and meta-analysis comparing 10 non-randomized studies from 2002 to 2015 on 5,919 patients) (p = 0.02), Petronio et al. [15] (p < 0.001), Oguri et al.[16] (p = 0.03) and O’Sullivan et al. [13] (p = 0.018). Brecker and colleagues claimed that there is no difference [17] (A Multicenter 5-year propensity score-matched analysis of 245 pairs of patients in the ADVANCE study, a prospective, non-randomized study) (p = 0.95).
Incidence of post-operative complications such as; AKI, Stroke, Heart block and mortality showed no differences between both group, which merges with several studies [14,15], this results were recorded despite the use of contrast dye in CSLA patients similar to Bagur et al. [18] study.
In our study, 37.5% of patients in the CSLA group had “mild” Aortic Regurge (AR) and the rest had none. 6.1% of the GA group had “moderate” AR, 48.5% had “mild” AR and the rest had none. This is against most studies that showed more AR with CSLA, but still in our study all AR was mild except 2 (9.1%) who had moderate AR in the GA group. All are statistically insignificant (p=0.193). Most studies [8,19] showed more incidence of Aortic Regurge with CSLA, probably due to lack of TEE during the procedure.
There was no difference in mortality (p=0.238) despite the presence of 2 cases having EUROSCORE II more than 20% in the GA group. This lack of difference is consistent with all the studies except Villablanca et al. [8] that showed less mortality with CSLA (p=0.01) which happen to be the largest meta-analysis to date on 10,572 patients from 26 studies.
An important caveat to keep in mind when analyzing the literature is to recognize that because GA is typically used when an institution is at the bottom of the learning curve, that differences noted in outcomes between GA and sedation, especially when compared at different time points, maybe biased by the procedural list’s learning curve, not the type of anesthetic [20].
Conclusion
CSLA showed better intraoperative hemodynamic stability, less need for inotropic support and less hospital stay. Further studies are needed to assess the financial benefits and cost-effectiveness.
Limitations of the Study
Being a single center study and lack of TEE guidance in patients with CSLA added some limitation to the study.
Competing Interests
Nothing to declare.
References
- Gross WL, Weiss MS (2015) Non-operating room anesthesia. miller’s anesthesia Chapter 90(2nd edition). 2646-2673.
- Thourani VH, Kodali S, Makkar RR, Herrmann HC, Williams M, et al. (2016) Transcatheter aortic valve replacement versus surgical valve replacement in intermediate-risk patients: A propensity score analysis. Lancet 87: 2218-2225.
- Cribier A (2012) Development of Transcatheter Aortic Valve Implantation (TAVI): A 20-year odyssey. Arch Cardiovasc Dis 105: 146-152.
- Khashaba AA, Adel W, Roshdi A, Gafar A, Essam S, et al. (2014) First egyptian experience of transcatheter aortic valve implantation: immediate results and one year follow up. Egypt Hear J. 66: 17-21.
- Wiegerinck EM, Eberl S, Boerlage-van Dijk K, Koch KT, Yong ZY, et al. (2013) TCT-719 Clinical Outcomes after Transcatheter Aortic Valve Implantation Under Local Analgesia. J Am Coll Cardiol. 62: B219.
- Wiegerinck EMA, Boerlage-Van Dijk K, Koch KT, Yong ZY, Vis MM, et al. (2014) Towards minimally invasiveness: Transcatheter aortic valve implantation under local analgesia exclusively. Int J Cardiol. 176: 1050-1052.
- Guarracino F, Landoni G (2012) Con: Transcatheter aortic valve implantation should not be performed under general anesthesia. J Cardiothorac Vasc Anesth. 26: 736-739.
- Villablanca PA, Mohananey D, Nikolic K, Bangalore S, Slovut DP, et al. (2018) Comparison of local versus general anesthesia in patients undergoing transcatheter aortic valve replacement: A meta-analysis. Catheter Cardiovasc Interv. 91: 330-342.
- Fassl J. (2012) Pro: Transcatheter aortic valve implantation should be performed with general anesthesia. J Cardiothorac Vasc Anesth. 26: 733-735.
- Maldonado Y, Baisden J, Villablanca PA, Weiner MM, Ramakrishna H, et al. (2018) General anesthesia versus conscious sedation for transcatheter aortic valve replacement—an analysis of current outcome data. J Cardiothorac Vasc Anesth. 32: 1081-1086.
- Palermo C, Degnan M, Candiotti K, Salerno T, de Marchena E, et al. (2016) Monitored anesthesia care versus general anesthesia: experience with the medtronic corevalve. J Cardiothorac Vasc Anesth. 30: 1234-1237.
- Noyez L, Kievit PC, van Swieten HA, de Boer MJ. (2012) Cardiac operative risk evaluation: The EuroSCORE II, does it make a real difference?. Netherlands Hear J. 20: 494-498.
- O’ Sullivan KE, Bracken-Clarke D, Segurado R, Barry M, Sugrue D, et al. (2014) Is local anesthesia the optimum strategy in retrograde transcatheter aortic valve implantation? A systematic review and meta-analysis. Thorac Cardiovasc Surg 62: 489-497.
- D’Errigo P, Ranucci M, Covello RD, Biancari F, Rosato S, et al. (2016) Outcome after general anesthesia versus monitored anesthesia care in transfemoral transcatheter aortic valve replacement. J Cardiothorac Vasc Anesth. 30: 1238-1243.
- Petronio AS, Giannini C, De Carlo M, Bedogni F, Colombo A, et al. (2016) Anaesthetic management of transcatheter aortic valve implantation: results from the Italian CoreValve registry. EuroIntervention 12: 381-388.
- Oguri A, Yamamoto M, Mouillet G, Gilard M, Laskar M, et al. (2014) Clinical outcomes and safety of transfemoral aortic valve implantation under general versus local anesthesia subanalysis of the French aortic national CoreValve and Edwards 2 registry. Circ Cardiovasc Interv. 7: 602-610.
- Brecker SJ, Bleiziffer S, Bosmans J, Gerckens U, Tamburino C, et al. (2016) Impact of anesthesia type on outcomes of transcatheter aortic valve implantation (from the multicenter advance study). Am J Cardiol. 117: 1332-1338.
- Bagur R, Rodés-Cabau J, Doyle D, De Larochellière R, Villeneuve J, et al. (2011). Usefulness of TEE as the primary imaging technique to guide transcatheter transapical aortic valve implantation. JACC Cardiovasc Imaging 4: 115-124.
- De Brito FS, Carvalho LA, Sarmento-Leite R, Mangione JA, Lemos P, et al. (2015) Outcomes and predictors of mortality after transcatheter aortic valve implantation: results of the Brazilian registry. Catheter Cardiovasc Interv. 85: E153-162
- Hutchinson N (2011) Sedation vs general anaesthesia for the ‘high-risk’ patient-what can TAVI teach us? ‘Hypothesis. Anesthesia. 66: 968-972.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi