Research Article, Int J Cardiovasc Res Vol: 6 Issue: 5
Coronary Flow Parameters Assessed by Transesophageal Echocardiography in Patients with Coronary Artery Ectasia Baseline Measurements and the Effects of Intravenous Verapamil
Hany Awadalla* and Hazem Khorshid
Department of Cardiovascular Medicine, Ain Shams University Hospitals and Medical School, Egypt
*Corresponding Author : Hany Awadalla, MD, FSCAI
Department of Cardiovascular Medicine, Ain Shams University Hospitals and Medical School, Abbassia, Cairo, 11566, Egypt
Tel: +201000778707
E-mail: Hany.Awadalla@med.asu.edu.eg
Received: October 06, 2017 Accepted: October 16, 2017 Published: October 23, 2017
Citation: Awadalla H, Khorshid H (2017) Coronary Flow Parameters Assessed by Transesophageal Echocardiography in Patients with Coronary Artery Ectasia Baseline Measurements and the Effects of Intravenous Verapamil. Int J Cardiovasc Res 6:5. doi: 10.4172/2324-8602.1000327
Abstract
Background and rationale: Coronary artery ectasia (defined as luminal dilatation 1.5 to 2 times the adjacent healthy coronary artery or the diameter of the corresponding coronary artery in the control group in case of diffuse ectasia) is an uncommon disorder, usually associated with underlying myocardial ischemia. Micro-circulatory dysfunction has been demonstrated as one possible mechanism to explain ischemia in this disorder. Calcium antagonists have been proven to relieve microvascular spasm.
Aim of the study: To test the hypothesis that relieving microvascular spasm in patients with coronary artery ectasia, through intravenous administration of verapamil, may result in improvement of microvascular coronary flow as reflected by coronary flow parameters assessed by transesophageal echocardiography (TEE).
Patients and methods:
Thirty patients with angiographically documented coronary artery ectasia of the left anterior descending artery were prospectively enrolled in the current study. Ten patients with normal coronary arteries were included as controls. All forty patients underwent TEE using pulsed wave Doppler (PWD) to measure peak systolic and diastolic velocities (m/sec); systolic, diastolic and total velocity time integrals (cm); and the systolic, diastolic and total coronary blood flow (cm³/min) in the proximal LAD before and after intravenous injection of verapamil (0.1 mg/kg).
Results: Resting systolic, diastolic, and total coronary blood flow (cm³/min) were significantly higher in patients with ectasia compared to normal subjects (60.83 ± 27.7 cm³/min versus 25.31 ± 9.01 cm³/min, p<0.001; 126.89 ± 49.22 cm³/min versus 53.15 ± 18.30 cm³/min, p<0.001; and 188.02 ± 70.36 cm³/min versus 78.46 ± 25.97 cm³/min, p<0.001). There was a trend, not reaching statistical significance, towards higher basal peak velocities in normal subjects compared to patients with ectasia. In patients with coronary artery ectasia, intravenous injection of verapamil resulted in an increase in all observed coronary flow parameters including: peak systolic velocity (m/sec) from 0.19 ± 0.05 to 0.21 ± 0.04, p=<0.05, peak diastolic velocity (m/sec) from 0.39 ± 0.11 to 0.48 ± 0.15, p=<0.001, systolic velocity time integral (cm) from 3.0 ± 1.05 to 3.38 ± 0.78, p=<0.05, diastolic velocity time integral (cm) from 6.22 ± 1.97 to 8.42 ± 2.09, p=<0.001; total velocity time integral (cm) from 9.22 ± 2.73 to 11.8 ± 2.64, p=<0.001, systolic coronary blood flow (cm³/min) from 60.83 ± 27.7 to 69.0 ± 22.7, p=<0.05, diastolic coronary blood flow (cm³/min) from 126.89 ± 49.22 to 173.01 ± 62.4 p=<0.001, and total coronary blood flow (cm³/min) from 188.02 ± 70.36 to 242.0 ± 81.82, p=<0.001.
Conclusion: Intravenous administration of verapamil resulted in statistically significant improvement of coronary flow parameters in patients with coronary artery ectasia. Further studies are needed to confirm whether continued treatment with verapamil translates to symptomatic improvement in the clinical setting.
Keywords: Coronary artery ectasi; Micro-circulatory dysfunction; Coronary blood flow
Introduction
Coronary artery ectasia (CAE) is defined as luminal dilatation 1.5 to 2 times the adjacent healthy coronary artery or 1.5 to 2 times the diameter of the corresponding coronary artery in the control group in case of diffuse ectasia [1]. Previous reports have demonstrated microcirculatory dysfunction in patients with isolated coronary artery ectasia [2]. Previous studies have pointed out to the beneficial effect of verapamil on microvascular oxygen delivery in the experimental setting [3], as well as on coronary microvascular flow assessed by positron emission tomography (PET) [4]. Whether this beneficial effect extends to the underlying microcirculatory dysfunction observed in patients with isolated coronary artery ectasia remains unexplored. The current study examined the effect of intravenous verapamil on coronary flow parameters, measured by transesophageal echocardiography, in patients with isolated coronary artery ectasia.
Patients and Methods
The current study included thirty patients referred for elective coronary angiography and diagnosed with isolated coronary artery ectasia. Ten patients who had normal coronary arteries on elective coronary angiography were enrolled as controls.
All patients underwent Transesophageal Echocardiography (TEE) using a GE® Vivid Five system (Vingmed Technology, USA) cardiac ultrasound machine. A 5 MHz multiplane phased-array probe was used to obtain 2D views and Doppler measurements. After lubrication of the probe and local anesthesia using Xylocaine spray (10%), every patient was asked to swallow during probe introduction.
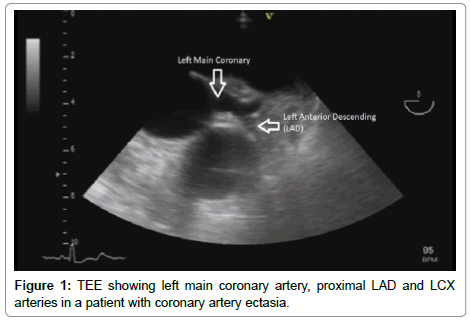
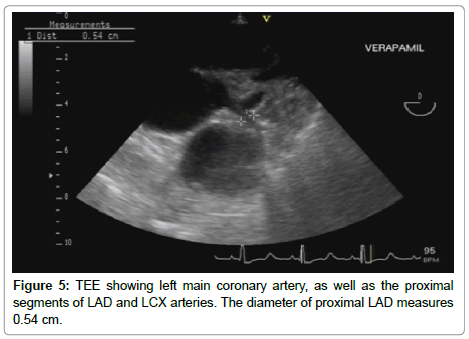
The probe was introduced till about 30 cm from the incisor teeth at which level the aortic cusps could be seen (basal short axis view at the level of the aortic valve). The probe was then withdrawn slowly till the opening of the left main coronary artery was clearly visible. Fine adjustments with rotation and flexion were made to obtain an optimal image of the left anterior descending coronary artery. The opening of the left main coronary artery could be seen at the 2 o’clock position of the aortic ring. The bifurcation of the left main coronary artery was observed as Y-shaped, with the left circumflex artery appearing as continuation of the left main coronary artery, and the left anterior descending coronary artery lying in a plane almost perpendicular to that of the left main and left circumflex coronary arteries.
Measurement of the diameter of the left anterior descending artery was documented in centimeters by two-dimensional mode.
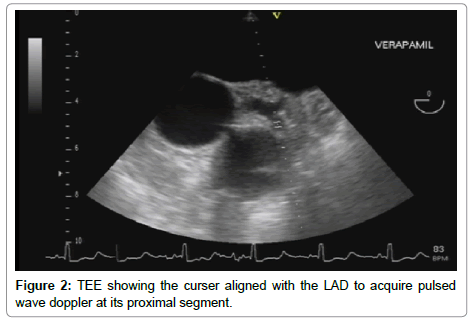
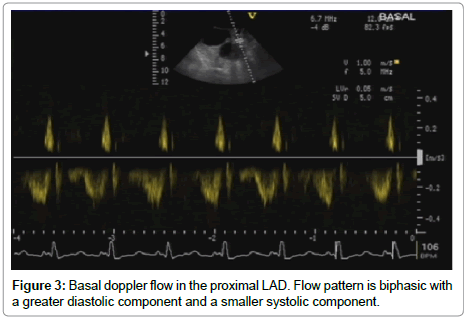
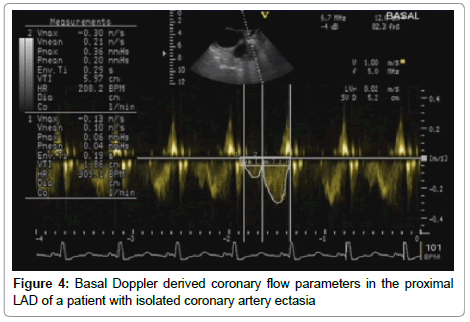
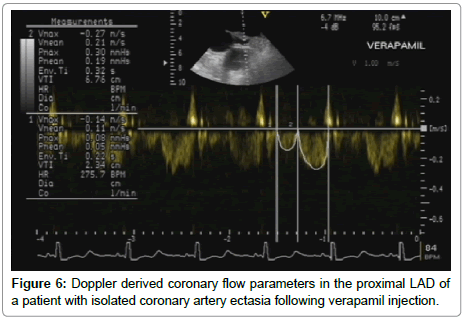
Pulsed Wave (PW) sample volume was placed over the proximal portion of the LAD, and the direction of the sample volume was made as parallel as possible to that of the LAD, followed by spectral recording of the flow velocity, with assessment of the following parameters: Peak systolic and diastolic velocities (m/sec); Systolic, diastolic, and total velocity time integrals (VTI) (cm). The coronary blood flow parameters (systolic, diastolic and total) were calculated using the following formula: Coronary flow (cm/min)=Coronary cross section area X Velocity time integral X heart rate. Following Intravenous injection of verapamil bolus in a dose of 0.1 mg/kg, heart rate, blood pressure and all the previously mentioned measurements were reassessed within 5 minutes of verapamil administration (Figures 1-6).
Data management
The data was collected, revised, verified then edited on PC. The data was then analyzed statistically using SPSS statistical package version 15. Comparisons were made between the 2 groups using the t-test for continuous variables and the chi square test (x2) for categorical variables. Comparison between continuous variables within each group before and after verapamil injection was done using paired samples t-test. Categorical variables were expressed as their absolute and relative frequencies (percentage), while continuous variables were presented as mean values ± standard deviation. Differences were considered statistically significant at a p value <0.05 level and highly significant at a p value<0.001.
Results
The current study included thirty patients with documented isolated coronary artery ectasia, and ten control subjects. There were no statistically significant differences between both groups in baseline clinical or demographic variables. Data are summarized in Table 1.
| VARIABLE | TOTAL COHORT Number=40 |
GROUP A Number=30 |
GROUP B Number=10 |
p-value |
|---|---|---|---|---|
| Age (y) | 51.03± 7.96 | 51.33 ± 7.76 | 50.1 ± 8.93 | >0.05 |
| Males | 26 (65%) | 22 (73.3%) | 4 (40%) | >0.05 |
| Hypertension | 24 (60%) | 19 (63.3%) | 5 (50%) | >0.05 |
| Diabetes Mellitus | 17 (42.5%) | 13 (43.3%) | 4 (40%) | >0.05 |
| Smoking | 19 (47.5%) | 16 (53.3%) | 3 (30%) | >0.05 |
| Dyslipidemia | 14 (35%) | 12 (40%) | 2 (20%) | >0.05 |
| Family history | 4 (10%) | 3 (10%) | 1 (10%) | >0.05 |
Table 1: Baseline clinical and demographic variables in patients with ectasia (Group A) and the control group (Group B).
Coronary doppler parameters
• Pulsed wave Doppler parameters, namely peak systolic and diastolic velocities (m/sec); systolic, diastolic and total velocity time integrals (cm); as well as systolic, diastolic and total coronary blood flow (cm³/min) in the LAD (before and five minutes after intravenous injection of verapamil) were recorded.
• Table 2 summarizes the baseline Doppler coronary flow parameters in both groups. Of interest is the observation that peak systolic and peak diastolic velocities were higher in the group B than in group A, however the difference was not statistically significant (p > 0.05). A highly significant greater systolic, diastolic and total coronary blood flow were observed in group A as compared to group B (60.83 ± 27.7 versus 25.31 ± 9.01, 126.89 ± 49.22 versus 53.15 ± 18.3 and 188.02 ± 70.36 versus 78.46 ± 25.97 cm³/min, respectively, p value<0.001).
| VARIABLE | GROUP A Number=30 |
GROUP B Number=10 |
t-test | |
|---|---|---|---|---|
| t | p-value | |||
| Peak systolic velocity (m/sec) | 0.19 ± 0.05 | 0.21 ± 0.07 | -1.13 | >0.05 |
| Peak diastolic velocity (m/sec) | 0.39 ± 0.11 | 0.43 ± 0.15 | -0.91 | >0.05 |
| Systolic velocity time integral (cm) | 3.0 ± 1.05 | 2.97 ± 1.12 | -0.09 | >0.05 |
| Diastolic velocity time integral (cm) | 6.22 ± 1.97 | 6.0 ± 1.57 | 0.33 | >0.05 |
| Total velocity time integral (cm) | 9.22 ± 2.73 | 8.96 ± 2.52 | 0.27 | >0.05 |
| Systolic coronary blood flow (cm³/min) | 60.83 ± 27.7 | 25.31 ± 9.01 | 3.96 | <0.001 |
| Diastolic coronary blood flow (cm³/min) | 126.89 ± 49.22 | 53.15 ± 18.30 | 4.60 | <0.001 |
| Total CBF (cm³/min) | 188.02 ± 70.36 | 78.46 ± 25.97 | 4.78 | <0.001 |
Table 2: Baseline Doppler coronary flow parameters in patients with ectasia (Group A) and the control group. (Group B).
• In group A, intravenous injection of verapamil resulted in a statistically significant increase in the peak systolic velocity, systolic VTI and systolic coronary flow (P<0.05) and a highly significant increase in the peak diastolic velocity, diastolic VTI, total VTI, diastolic coronary flow and total coronary flow (P<0.001) (Table 3).
| VARIABLE | GROUP A Basal |
GROUP A Verapamil |
Paired samples t-test |
|
|---|---|---|---|---|
| t | p-value | |||
| Peak systolic velocity (m/sec) | 0.19 ± 0.05 | 0.21 ± 0.04 | -3.4 | <0.05 |
| Peak diastolic velocity (m/sec) | 0.39 ± 0.11 | 0.48 ± 0.15 | -4.85 | <0.001 |
| Systolic velocity time integral (cm) | 3.0 ± 1.05 | 3.38 ± 0.78 | -3.23 | <0.05 |
| Diastolic velocity time integral (cm) | 6.22 ± 1.97 | 8.42 ± 2.09 | -10.13 | <0.001 |
| Total velocity time integral (cm) | 9.22 ± 2.73 | 11.8 ± 2.64 | -11.30 | <0.001 |
| Systolic coronary blood flow (cm³/min) | 60.83 ± 27.7 | 69.0 ± 22.7 | -2.93 | <0.05 |
| Diastolic coronary blood flow (cm³/min) | 126.89 ± 49.22 | 173.01 ± 62.4 | -8.78 | <0.001 |
| Total coronary blood flow (cm³/min) | 188.02 ± 70.36 | 242.0 ± 81.82 | -9.14 | <0.001 |
Table 3: Doppler coronary flow parameters at baseline and five minutes after intravenous injection of 0.1 mg/kg of verapamil in patients with ectasia (Group A).
• In group B, intravenous injection of verapamil resulted in a statistically significant increase in all doppler parameters with a highly significant increase in the diastolic VTI, systolic VTI and total VTI (p<0.001) (Table 4).
| VARIABLE | GROUP B Basal |
GROUP B Verapamil |
Paired samples t-test | |
|---|---|---|---|---|
| t | ρ value | |||
| Peak systolic velocity (m/sec) | 0.21 ± 0.07 | 0.24 ± 0.08 | -2.59 | <0.05 |
| Peak diastolic velocity (m/sec) | 0.43 ± 0.15 | 0.52 ± 0.22 | -3.1 | <0.05 |
| Systolic velocity time integral (cm) | 2.97 ± 1.12 | 3.71 ± 1.25 | -4.58 | <0.001 |
| Diastolic velocity time integral (cm) | 6.0 ± 1.57 | 8.07 ± 2.32 | -4.86 | <0.001 |
| Total velocity time integral (cm) | 8.96 ± 2.52 | 11.77 ± 3.27 | -6.26 | <0.001 |
| Systolic coronary blood flow (cm³/min) | 25.31 ± 9.01 | 32.57 ± 10.56 | -4.71 | <0.05 |
| Diastolic coronary blood flow (cm³/min) | 53.15 ± 18.30 | 73.62 ± 33.03 | -3.58 | <0.05 |
| Total coronary blood flow (cm³/min) | 78.46 ± 25.97 | 106.19 ± 41.55 | -4.72 | <0.05 |
Table 4: Doppler coronary flow parameters at baseline and five minutes after intravenous injection of 0.1 mg/kg of verapamil in the control group (Group B).
• Hemodynamic sequelae: Table 5 summarizes hemodynamic sequelae of verapamil injection in both groups. No statistically significant differences were observed.
| VARIABLE | GROUP A Number=30 |
GROUP B Number=10 |
t-test | |
|---|---|---|---|---|
| t | p value | |||
| BP before Verapamil (mmHg) | 130.33 ± 13.83 | 127.0 ± 13.38 | 0.67 | >0.05 |
| systolic | ||||
| diastolic | 81.83 ± 9.87 | 85.0 ± 9.72 | -0.88 | >0.05 |
| HR before Verapamil (bpm) | 96.2 ± 14.06 | 101.3 ± 23.41 | -0.83 | >0.05 |
| BP after Verapamil (mmHg) | 127.67 ± 14.78 | 128.5 ± 12.92 | -0.16 | >0.05 |
| systolic | ||||
| diastolic | 78.67 ± 9.19 | 81.5 ± 10.55 | -0.81 | >0.05 |
| HR after Verapamil (bpm) | 94.57 ± 13.06 | 99.7 ± 24.70 | -0.85 | >0.05 |
Table 5: Hemodynamic data of the two studied groups before and after Verapamil injection.
Discussion
Coronary artery ectasia (CAE) has been a challenging entity with respect to its etiology, clinical consequences, and treatment options. While there is no general agreement as to the exact etiology, observers consider ectasia to be a variant of coronary atherosclerosis [1]. Other potential etiologies include inflammatory and connective tissue disorders, and a possible congenital disorder [5]. Clinical presentations include stable angina pectoris, unstable angina pectoris [6], and possibly myocardial infarction secondary to thrombosis in an ectatic segment with consequent distal embolization [7,8].
The main coronary angiographic characteristics of CAE are impaired coronary blood flow, delayed antegrade coronary dye filling, segmental back flow phenomenon (milking phenomenon) and stasis with local deposition of dye in dilated coronary segments [9].
In patients with isolated CAE, occurrence of ischemia may be attributable to conversion of coronary flow from a laminar pattern to a turbulent pattern in the dilated segments [10], a decrease in the blood flow velocity [6], microcirculatory dysfunction (possibly autoregulatory dysfunction) with lower coronary flow reserve. In a study by Akyürek et al. [2], following intracoronary administration of papaverine (a potent hyperemic stimulus), the coronary flow reserve was 1.51 in CAE as compared with 2.67 in control arteries, suggesting microvascular dysfunction as the cause of myocardial ischemia.
The main findings of the current study include baseline coronary flow velocities that are not different, in terms of statistical significance, between ectatic and normal coronary arteries. These findings concur with findings reported by Akyürek et al., who demonstrated baseline peak velocities of coronary blood flow (obtained invasively by use of Doppler flow wire) that were not statistically different between both ectatic and normal vessels [2]. The resting volumetric blood flow in the current study was found to be significantly higher in patients with ectasia. This finding is concordant with Akyürek et al. [2] who reported that volumetric coronary blood flow was significantly higher in the ectatic arteries compared to normal arteries. This is attributed mainly to the statistically significant larger cross-sectional area (CSA) of the ectatic coronaries compared to normal coronaries, where the volumetric coronary flow is calculated as the product of the CSA of the examined coronary and velocity time integral (VTI) of the coronary flow.
In the current study intravenous injection of verapamil caused statistically significant increase in the epicardial coronary crosssectional area (CSA) in normal coronary arteries (p<0.05). This finding is consistent with the results of several studies that showed that verapamil induces a dose-dependent coronary vasodilatation in normal epicardial coronary vessels and markedly decreases the tone in these vessels [11,12].
On the other hand, intravenous verapamil injection in ectatic coronary arteries caused a mild, statistically insignificant, increase in the epicardial coronary CSA (p>0.05). This could be explained by the underlying histological changes in the wall of the ectatic coronary arteries which reveal grossly thickened and fibrotic intima with extensive lipid deposition and marked thinning of the media [13] leading to loss of the basal tone of the ectatic epicardial coronary vessels and failure to respond adequately to vasodilators.
Calcium channel blockers produce a dose-dependent increase in coronary blood flow [14-17]. Direct dilatory effects on the coronary circulation also improves the coronary perfusion particularly in cases of coronary spasm [18] and intravenous verapamil has been used successfully to treat isolated coronary artery spasm [19].
The therapeutic benefits of calcium channel blockers in treating coronary slow flow phenomenon have been well investigated [20-22]. Coronary slow flow phenomenon and CAE share a common pathophysiologic background of microvascular dysfunction as a cause of myocardial ischemia [2,23]. Both statements have lead the authors of the current study to rationally hypothesize a potential beneficial effect of verapamil on coronary flow parameters in patients with coronary artery ectasia.
In the present study, intravenous injection of verapamil in patients with coronary artery ectasia caused a statistically significant increase in all coronary hemodynamic parameters, namely the peak velocities (systolic, diastolic and total); velocity time integrals (systolic, diastolic & total); and coronary blood flow with a highly statistically significant increase in the peak diastolic velocity, diastolic VTI, total VTI, diastolic coronary flow and total coronary flow (P<0.001).
Although verapamil causes dilatation in normal epicardial coronaries [11], this effect cannot be the main factor responsible for the observed increase in the coronary flow parameters in patients with CAE. Despite observed epicardial coronary vasodilatation following verapamil administration, the degree of coronary dilatation was neither pronounced nor statistically significant (p>0.05). The observed increase in coronary flow parameters in the ectatic vessels following verapamil administration may be attributed to the vasodilatation of the small resistance coronary vessels and improvement of microvascular function. This explanation is supported by earlier findings of lower myocardial blush grade observed in patients with CAE despite brisk epicardial flow, thereby suggesting a disrupted microvascular network [24].
Chew et al. [4] reported that verapamil dilates the systemic and coronary small vessel resistance bed without apparently increasing the myocardial metabolic demand. Ishihara et al. [25] also reported that intracoronary verapamil produces a dose-dependent dilation of coronary resistance vessels. Several clinical studies have also demonstrated that slow coronary flow that is sometimes observed after coronary intervention despite the absence of a flow-restricting epicardial coronary lesion responds promptly to intracoronary verapamil [26-29].
Limitations
The current study has many limitations, including a small sample size, lack of intermediate and long-term follow-up of a potential beneficial effect of oral -rather than intravenous- verapamil on coronary flow parameters in patients with coronary artery ectasia. Whether the observed beneficial effects of intravenous verapamil on coronary flow parameters in patients with coronary artery ectasia would still be seen with oral verapamil administration, and whether this translates to improved exercise capacity and higher angina threshold remain to be tested in future studies.
References
- Swaye PS, Fisher LD, Litwin P, Vignola PA, Judkins MP, et al. (1983) Aneurysmal coronary artery disease. Circulation 67: 134-138.
- Akyürek O, Berkalp B, Sayin T, Kumbasar D, KervancioÄŸlu C, et al. (2003) Altered coronary flow properties in diffuse coronary artery ectasia. Am Heart J 145: 66-72.
- Hangai-Hoger N, Tsai AG, Friesenecker B, Cabrales P, Intaglietta M (2005) Microvascular oxygen delivery and consumption following treatment with verapamil. Am J Physiol Heart Circ Physiol 288: H1515-1520.
- Chew CY, Brown BG, Singh BN, Wong MM (1983) Effects of verapa mil on coronary hemodynamic function and vasomotility relative to its mechanism of antianginal action. Am J Cardiol 51: 699-705.
- Befeler B, Aranda JM, Embi A, Mullin FL (1977) Coronary artery aneurysms: study of their etiology, clinical course and effect on left ventricular function and prognosis. Am J Med 62: 597-607.
- Rath S, Har-Zahav Y, Battler A, Agranat O, Rotstein Z, et al. (1985) Fate of nonobstructive aneurysmatic coronary artery disease: angiographic and clinical follow-up report. Am Heart J 109: 785-791.
- Al-Harthi SS, Nouh MS, Arafa M, al-Nozha M (1991) Aneurysmal dilatation of the coronary arteries: diagnostic patterns and clinical significance. Int J Cardiol 30:191-194.
- Rab ST, Smith DW, Alimiurug BN, Rab R (1990) Thrombolytic therapy in coronary artery ectasia and acute myocardial infarction. Am Heart J 119: 955-957
- Kruger D, Stierle U, Herrmann G, Simon R, Sheikhzadeh A (1999) Exercise-induced myocardial ischemia in isolated coronary artery ectasias and aneurysms ("dilated coronopathy"). J Am Coll Cardiol 34: 1461-1470.
- Topaz O, DiSciascio G, Cowley MJ, Goudreau E, Soffer A, et al. (1991) Angiographic features of left main coronary artery aneurysms. Am J Cardiol 67: 1139-1142.
- Simonetti I, Trivella MG, Michelassi C, Parodi O, Denes DM, et al. (1986) Dose-response scrutiny of coronary vasodilation after intracoronary verapamil in man. A quantitative cineangiographic study. Eur Heart J 7: 848-858.
- Adachi H, Tomoike H, Nishijima H, Hayashi Y, Yamada A, et al. (1987) Effects of verapamil and nitroglycerin on coronary and systemic hemodynamics in conscious dogs. J Pharmacol Exp Ther 241: 1072-1078.
- Ramappa P, Kottam A, Kuivanemi H, Thatai D (2007) Coronary artery ectasia--is it time for a reappraisal? Clin Cardiol 30: 214-217.
- Engel HJ, Lichtlen PR (1981) Beneficial enhancement of coronary blood flow by nifedipine. Comparison with nitroglycerin and beta blocking agents. Am J Med 71: 658-666.
- Zacca NM, Verani MS, Chahine RA, Miller RR (1982) Effect of nifedipine on exercise-induced left ventricular dysfunction and myocardial hypoperfusion in stable angina. Am J Cardiol 50: 689-695.
- Serruys PW, Hooghoudt TE, Reiber JH, Slager C, Brower RW, et al. (1983) Influence of intracoronary nifedipine on left ventricular function, coronary vasomotility, and myocardial oxygen consumption. Br Heart J 49: 427-441.
- Pepine CJ, Lambert CR (1988) Effects of nicardipine on coronary blood flow. Am Heart J 116: 248-254.
- Kostuk WJ, Pflugfelder P (1987) Comparative effects of calcium entry-blocking drugs, beta-blocking drugs, and their combination in patients with chronic stable angina. Circulation. 75: V114-121.
- Nussmeier NA, Slogoff S (1985) Verapamil treatment of intraoperative coronary artery spasm. Anesthesiology 62: 539-541.
- Beltrame JF, Turner SP, Leslie SL, Solomon P, Freedman SB, et al. (2004) The angiographic and clinical benefits of mibefradil in the coronary slow flow phenomenon. J Am Coll Cardiol 44: 57-62.
- McIvor ME, Undemir C, Lawson J, Reddinger J (1995) Clinical effects and utility of intracoronary diltiazem. Cathet Cardiovasc Diagn 35: 287-291.
- Sütsch G, Oechslin E, Mayer I, Hess OM (1995) Effect of diltiazem on coronary flow reserve in patients with microvascular angina. Int J Cardiol 52: 135-143.
- Li L, Gu Y, Liu T, Bai Y, Hou L, et al. (2012) A randomized, single-center double-blinded trial on the effects of diltiazem sustained-release capsules in patients with coronary slow flow phenomenon at 6-month follow-up. PLoS One 7: e38851.
- Gibson CM, Cannon CP, Daley WL, Dodge JT Jr, Alexander B Jr, et al. (1996) TIMI frame count: a quantitative method of assessing coronary artery flow. Circulation 93: 879-888
- Ishihara M, Sato H, Tateishi H, Kawagoe T, Shimatani Y, et al. (1997) Effects of various doses of intracoronary verapamil on coronary resistance vessels in humans. Jpn Circ J 61: 755-761.
- Pomerantz R, Kuntz RE, Diver DJ, Safian RD, Baim DS (1991) Intracoronary verapamil for the treatment of distal microvascular coronary artery spasm following PTCA. Cathet Cardiovasc Diagn 24: 283-285.
- Feld H, Lichstein E, Schachter J, Shani j (1992) Early and late angiographic findings of the “no reflow” phenomenon following direct angioplasty as primary treatment for acute myocardial infarction. Am Heart J 123: 782–785.
- Piana RN, Paik GY, Moscucci M, Cohen DJ, Gibson CM, et al. (1994) Incidence and treatment of 'no-reflow' after percutaneous coronary intervention. Circulation 89: 2514-2518.
- Ito H, Okamura A, Iwakura K, Masuyama T, Hori M, et al. (1996) Myocardial perfusion patterns related to thrombolysis in myocardial infarction perfusion grades after coronary angioplasty in patients with acute anterior wall myocardial infarction. Circulation 93: 1993-1999.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi