Case Report, Res Rep Gastroenterol Vol: 1 Issue: 1
Crohns Colitis with Marked Peripheral Eosinophilia
Matar K1*, Helal A1, Yaacoub A2 and Mari A3
1European Gaza Hospital, Khanyounis city- Alfukhari, Gaza Strip, Palestine
2Rambam Campus, Affiliated to Ruth and Rappaport Faculty of Medicine, Haifa, Israel
3Hillel Yaffe Medical Center, Hadera, Israel
*Corresponding Author : Khaled Matar
Gastroenterology Unit, European Gaza Hospital, Khanyounis city- Alfukhari, Gaza strip-Palestine
Tel: +972 592155123
E-mail: Aboayman2001@hotmail.com
Received: November 06, 2017 Accepted: November 21, 2017 Published: November 27, 2017
Citation: Matar K, Helal A, Yaacoub A, Mari A (2017) Crohn’s Colitis with Marked Peripheral Eosinophilia. Res Rep Gastroenterol 1:1
Abstract
Crohn’s disease (CD) is a disorder of multifactorial etiology characterized by trans-mural inflammation of the gastrointestinal tract. CD may involve the entire gastrointestinal tract and causes extra-intestinal manifestations. Eosinophils are granulocytic leukocytes that play a key role in mucosal innate host defense and play role in the pathogenesis chronic inflammatory mucosal disorders, including inflammatory bowel disease (IBD) We are reporting a case of Crohn’s disease associated with marked peripheral eosinophilia. A 25-year old, asymptomatic male patient referred from hematology clinic to our gastroenterology clinic, in the European Gaza Hospital, for diagnostic work-up for his marked peripheral eosinophilia. Extensive Hematologic workup revealed no cause for his eosinophilia. During follow up, he reported having bouts of intermittent abdominal pain and diarrhea. Colonoscopy was carried out which showed the right colon showing inflamed mucosa along with deep linear ulcerations. Histopathology showed a picture consistent with Crohn’s disease. We would like to highlight the possible relationship between eosinophilia and Crohn’s disease. Taking that point in consideration during eosinophilia work up leads to earlier diagnosis and prevent unnecessary invasive and expensive diagnostic procedures.
Keywords: Eosinophilia; Crohn’s disease; Colonoscopy
Case Presentation
25-year old male patient referred to gastroenterology clinic from hematology department for diagnostic work-up for his persistent leukocytosis mainly eosinophilia. During the follow up course, he started complaining of bouts of abdominal pain. The patient denied NSAID’s consumption fever, diarrhea or any acute illness recently. Abdominal examination was unremarkable except mild right iliac fossa tenderness.
Lab tests showed leukocytosis with predominance of eosinophils, normal albumin, normal Internationalized Normalization Ratio (INR), normal total bilirubin and normal liver enzymes but ESR was high. Autoimmune and infectious serological work up was negative.
CT scan Enterography revealed a thickened enhancing right colon including the Cecum. Terminal Ileum reported to be normal. Bone marrow aspirate and biopsy and peripheral blood smear: Hypercellular bone marrow with eosinophilia. No evidence of acute leukemia.
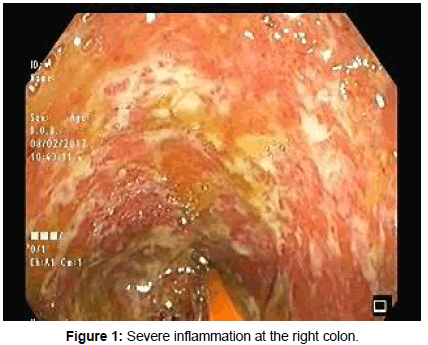
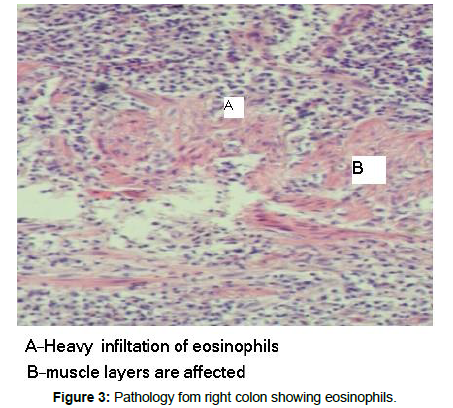
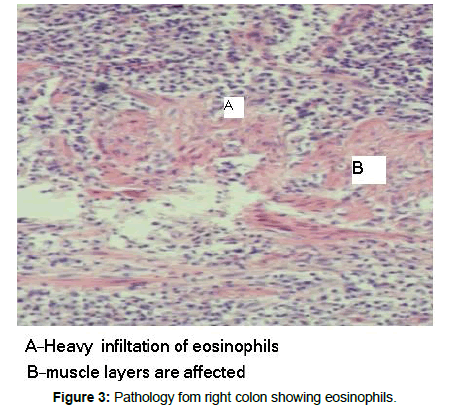
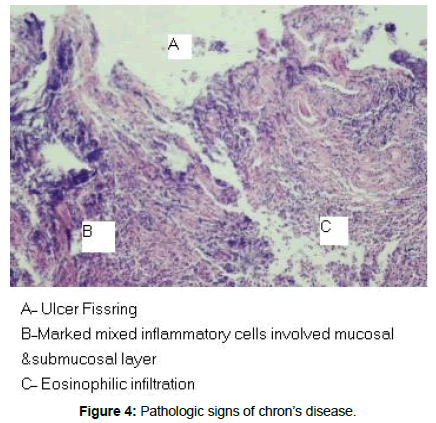
Colonoscopy revealed a severely inflamed right colonic mucosa (Figures 1 and 2), with deep linear ulcerations along with excess exudates. Right colonic biopsy was obtained and reported to be compatible with Crohn’s disease (Figures 3 and 4). Terminal ileum was normal. The patient was commenced on steroids and Mesalamine, followed by dramatic clinical and laboratory improvement.
Discussion
Eosinophils are leucocytes that have an essential role in immune reactions, inflammation, allergy and other critical physiological cellular and systemic mechanisms. Under physiological conditions, most of these cells are located in in the gastrointestinal tract, mainly, the stomach and intestine lamina propria. Eosinophils differentiate in the bone marrow from progenitor cells by the stimulation of several interleukins, mainly (IL)-3, IL-5, and granulocyte-macrophage colony stimulating factor [1]. The involvement of eosinophils in inflammatory bowel diseases pathogenesis is gaining more concern and investigation enthusiasm in the last decades. IBD pathogenesis is multifactorial, includes genetic causes, autoimmunity, infectious agents, environmental factors and many other possible factors. The cellular complexity and the multifactorial nature of inflammatory bowel diseases is well known and involves many inflammatory cells lymphocytes, macrophages, neutrophils, eosinophils [2].
Possible role of eosinophils in IBD pathogenesis is a proinflammatory cell and another important act is motility stimulation, the net pathological manifestations attributed to eosinophils activity may include diarrhea, inflammation, fibrosis and even strictures formation [3]. The whole inflammatory process probably initiated by an unknown antigenic stimulus which leads to amplified creation in the intestinal tract of leukotriens and chemoattractants to multiple inflammatory cells, including eosinophils [4,5]. Eosinophils contribute to the inflammatory process in the intestinal mucosa by the release of toxic proteins and cytokines that enhances the inflammatory process.
As the reported case showed dramatic improvement both clinically and laboratory including the complete blood count, this case highlights the importance of possible Eos/IBD association in cases of unexplained investigations peripheral eosinophilia, thereby obviating the need for further unwarrented investigations. Marked eosinophilia may be the presenting laboratory sign of inflammatory bowel diseases, and that important differential diagnosis should be taken in consideration during the work up process. The relationship between eosinophils and inflammatory bowel diseases pathogenesis should be further studied and assessed in order to better understand IBD pathogenesis and hopefully open new horizons for therapeutic targets.
References
- Mishra A, Hogan SP, Lee JJ, Foster PS, Rothenberg ME (1999) Fundamental signals that regulate eosinophil homing to the gastrointestinal tract. J Clin Invest 103: 1719-1727.
- Lampinen M, Carlson M, Håkansson LD, Venge P (2004) Cytokine-regulated accumulation of eosinophils in inflammatory disease. Allergy 59: 793-805.
- Lampinen M, Rönnblom A, Amin K, Kristjansson G, Rorsman F et al. (2005) Eosinophil granulocytes are activated during the remission phase of ulcerative colitis. Gut 54: 1714-1720.
- Forbes E, Murase T, Yang M, Matthaei KI, Lee JJ et al. (2004) Immunopathogenesis of experimental ulcerative colitis is mediated by eosinophil peroxidase. J Immunol 172: 5664-5675.
- Powrie F (1995) T cells in inflammatory bowel disease: protective and pathogenic roles. Immunity 3: 171-174.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi