Research Article, Int J Cardiol Res Vol: 12 Issue: 3
Diagnostic Value of Low Density Lipoprotein 4 in Patients with Documented Coronary Artery Disease
Ahmed Mordi Gaber Hammad*, Ahmed Abdlla Moustafa, Ghada Mahmoud Soltan, Ahmed Mokhtar Elkersh and Abdlla Moustafa Kamal
Department of Cardiology, Menoufia University, Al Minufiyah, Egypt
- *Corresponding Author:
- Ahmed Mordi Gaber Hammad
Department of Cardiology,
Menoufia University,
Al Minufiyah,
Egypt;
E-mail: dr.ahmedhammad01@yahoo.com
Received date: 02 January, 2020, Manuscript No. ICRJ-23-6112;
Editor assigned date: 07 January, 2020, PreQC No. ICRJ-23-6112 (PQ);
Reviewed date: 21 January, 2023, QC No. ICRJ-23-6112;
Revised date: 14 June, 2023, Manuscript No. ICRJ-23-6112 (R);
Published date: 12 July, 2023, DOI: 10.4172/2324-8602.1000508
Citation: Hammad AMG, Moustafa AA, Soltan GM, Elkersh AM, Kamal AM (2023) Diagnostic Value of Low Density Lipoprotein 4 in Patients with Documented Coronary Artery Disease. Int J Cardiol Res 12:3.
Abstract
Background: Hyperlipidemia is a well-established risk factor for Coronary Artery Disease (CAD). Small dense LDL particle subtypes (LDL 3 and LDL 4) have been observed to be more oxidizable and atherogenic. We aimed to identify the role of cholesterol particle subtypes in predicting CAD severity. Objective: The aim of this study was to identify novel biomarker (LDL 4) to predict severity of CAD on extended lipid profile compared to traditional cholesterol measurements. Methods: This is a cross sectional study which was conducted on 100 CAD patients admitted for elective coronary angiography. All patients were subjected to detailed history, physical examination, electrocardiography, echocardiography, laboratory investigations including total and differential cholesterol measurement and elective coronary angiography. Conclusion: Cholesterol subtype (LDL 4) is significantly correlated with severity of coronary artery disease. It is also a strong independent predictor of severity of CAD than traditional cholesterol measurements.
Keywords: Coronary artery disease, LDL 4; Cholesterol, subtypes, Cardiovascular, Hyperlipidemia
Introduction
Cardiovascular diseases are expected to be the main cause of death globally within the next 15 years owing to a rapidly increasing prevalence in developing countries and the rising incidence of obesity and diabetes. Cardiovascular diseases cause 38 percent of all deaths in North America and are the most common cause of death in European men under 65 years of age and the second most common cause in women [1]. Hyperlipidemia is a well-established risk factor for CAD. However, the term “hyperlipidemia” has been noted to be too broad given the varied roles played by different lipoproteins in the pathogenesis of CAD. Whereas LDL levels were found to correlate positively with the severity of CAD, HDL was noted to serve in a protective capacity [2].
On further exploration of LDL composition, it was observed that increasing LDL density (accompanied by a reduction in size) was associated with an increase in its pro-atherogenic potential and was subdivided and fractioned into four subtypes: LDL 1 to LDL 4 with increasing density from 1 through 4. Most risk scores only utilizes total cholesterol and HDL level for risk stratification of patients while ignoring the utility of lipoprotein sub-particles in the prediction of CAD, Whereas recent evidence suggests that the ‘quality’ rather than only the ‘quantity’ of LDL exerts a direct influence on the cardiovascular risk. Lipoprotein subclass profiles have been shown to identify CHD patients at higher risk for progression of coronary atherosclerosis [3].
Materials and Methods
Patient population
This study is a cross sectional study conducted on a convenient sample of 100 patients admitted at Menoufia university hospital for suspected coronary artery disease for either positive stress test for ischemia or history of acute coronary syndrome. The patients were classified into 2 groups according to Gensini score into group 1, low Gensini score including 42 patients and group 2, high gensini score including 58 patients [4]. The study protocol was formally reviewed and approved by the ethics committee for human research at Menoufia faculty of medicine with informed consent obtained from all participants prior to commencement of the study after thorough explanation of the study objectives [5].
Inclusion criteria
Adult male or female >18 years old with suspected CAD undergoing elective cardiac catheterization [6].
Exclusion criteria
Patients with pregnancy, acute infection blood donation within 8 weeks; any coagulopathy or bleeding disorder; on-going treatment for neoplastic, autoimmune or connective tissue disease or patients with any abnormal laboratory value or physical finding that may interfere with interpretation of the study results were excluded from our study. After exclusion of non-responders, drop out participants and those with exclusion criteria, 100 patients completed the study (this number was considered suitable enough sample for statistical analysis with significant results and correlations) [7].
Methods
All patients were subjected to detailed history, including CAD risk factors, physical examination, Electrocardiography (ECG), echocardiography and laboratory investigations included, complete blood picture, liver and kidney function, total and differential cholesterol measurement [8].
Some patients-who did not have history of CAD performed a stress ECG test. The protocol we used consisted of 2-min stages with 25 W incremental workload. Digital 12-lead Electrocardiograms (ECG) were acquired during the whole stress ECG test. The test was considered positive in the setting of ≥ 1 mm horizontal or downwardsloping ST depression 80 m. sec after J-point [9].
Blood samples were collected before cardiac catheterization. Patients fasted for >12 hours before cardiac catheterization. Blood was collected either from the antecubital vein or indwelling catheter into two 3.2% trisodium citrate tube after discarding the initial 3 ml of blood. Serum was separated by centrifugation at 2000 g for 15 minutes and stored at 70°C. Serum samples were batched and stored on dry ice and analyzed for The Vertical Auto Profile (VAP) cholesterol testing for LDL 4 [10].
Selective coronary angiography was performed using the percutaneous femoral approach. CAD severity was assessed by Gensini score as giving a severity score to each coronary stenosis as follows: 1 point for ≤ 25% narrowing, 2 points for 26% to 50% narrowing, 4 points for 51% to 75% narrowing, 8 points for 76% to 90% narrowing, 16 points for 91% to 99% narrowing, and 32 points for total occlusion [11]. Thereafter, each lesion score is multiplied by a factor that takes into account the importance of the lesion's position in the coronary circulation (5 for the left main coronary artery, 2.5 for the proximal segment of the left anterior descending coronary artery, 2.5 for the proximal segment of the circumflex artery, 1.5 for the midsegment of the left anterior descending coronary artery, 1.0 for the right coronary artery, the distal segment of the left anterior descending coronary artery, the posterolateral artery, and the obtuse marginal artery, and 0.5 for other segments) [12].
Finally, the Gensini score was calculated by summation of the individual coronary segment scores. The patients were classified into 2 groups according to Gensini score [13].
Statistical analysis
Statistical analysis was performed using statistical package for the social sciences version 22 (IBM Corp., Armonk, NY, USA). Quantitative data are expressed as means and standard deviations [14].
P-value ≤ 0.05 was considered to indicate significance. Correlation analysis assesses the strength of association between two variables. Multiple logistic regression analysis was used to detect the associations between lipid profile and both maternal and neonatal complications [15].
Results
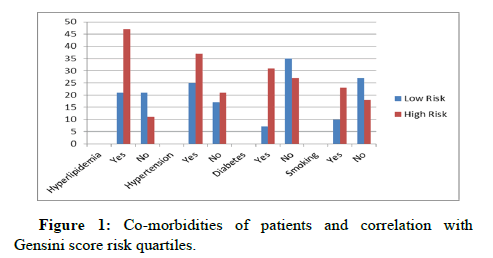
There was a significant difference in between the studied groups as regard to risk factors of CAD (hyperlipidemia, DM, smoking), with p values 0.001, 0.0001, 0.004 respectively, with non-significant difference as regarding hypertension between the two groups with p value 0.4 (Table 1 and Figure 1).
| Characteristics | All participants | Low risk | High risk | P-value | |||
|---|---|---|---|---|---|---|---|
| N=100 | N=42 | N=58 | |||||
| Yes | 68 | 68% | 21 | 50% | 47 | 81% | 0.001 |
| No | 32 | 32% | 21 | 50% | 11 | 19% | |
| Yes | 38 | 38% | 25 | 59.5% | 37 | 63.7% | 0.4 |
| No | 62 | 62% | 17 | 40.5% | 21 | 36.3% | |
| Yes | 38 | 38% | 7 | 16.6% | 31 | 53.4% | 0.0001 |
| No | 62 | 62% | 35 | 83.4% | 27 | 46.6% | |
| Ex-smoker | 22 | 22% | 5 | 11.9% | 17 | 29.3% | 0.004 |
| Yes | 33 | 33% | 10 | 24% | 23 | 39.7% | |
| No | 45 | 45% | 27 | 64.1% | 18 | 31% | |
Table 1: History of patients and correlation with Gensini score risk quartiles.
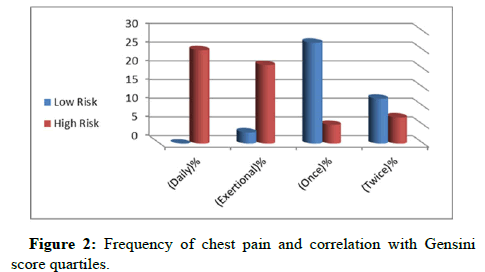
In Table 2 and Figure 2, patient presented with ACS in group I was 54.7% and in group II was 67.2% while patient presented with PST in group I was 45.3% and in group II was 32.8% with statistically nonsignificant difference, p value 0.14. As regarding frequency of chest pain, the results showed a significant difference between the groups p value 0.036 [16]. Table 3 shows non-significant correlation between the two groups as regarding all laboratory investigations (blood indices, liver and renal functions) (Table 3).
| Characteristics | All participants | Low risk | High risk | P-value | |||
|---|---|---|---|---|---|---|---|
| N=100 | N=42 | N=58 | |||||
| Patient presentation | N | F% | N | F% | N | F% | |
| ACS | 62 | 62% | 23 | 54.7% | 39 | 67.2% | 0.14 |
| PST | 38 | 38% | 19 | 45.3% | 19 | 32.8% | |
| Frequency of chest pain per week | |||||||
| (Daily)% | 25 | 25% | 0 | 0% | 25 | 43.1% | 0.036 |
| (Exertional)% | 24 | 24% | 3 | 7.1% | 21 | 36.2% | |
| (Once)% | 32 | 32% | 27 | 64.2% | 5 | 8.6% | |
| (Twice)% | 19 | 19% | 12 | 28.5% | 7 | 12% | |
Table 2: Patient presentation and frequency of chest pain.
| LABS | All participants | Low risk | High risk | P-value |
|---|---|---|---|---|
| N=100 | N=42 | N=58 | ||
| HB | 13.2 ± 2.07 | 13.4 ± 2.4 | 13.08 ± 1.7 | 0.33 |
| WBCS | 6.9 ± 1.9 | 6.7 ± 1.8 | 7 ± 1.9 | 0.409 |
| Platelets | 235.6 ± 69.6 | 225.2 ± 72.4 | 243.1 ± 67.2 | 0.2 |
| BUN | 20.6 ± 7.1 | 21.3 ± 9.6 | 20.2 ± 4.7 | 0.45 |
| Creat | 1 ± 25 | 99 ± 22 | 1 ± 26 | 0.508 |
| SGOT | 38.5 ± 22.6 | 41.2 ± 26.2 | 36.5 ± 20.6 | 0.28 |
| SGPT | 39.5 ± 23.7 | 44.2 ± 23.2 | 36.1 ± 20.7 | 0.09 |
Table 3: Labs of patients and correlation with Gensinin score risk.
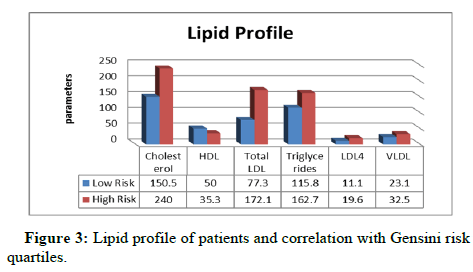
Total cholesterol, in group I, the mean was 150.5 ± 34.7 while in group II it was 240 ± 52.7 with P value=0.001. Total HDL, in group I, the mean was 50 ± 10.3 while in group II it was 35.3 ± 12.9 with P value=0.001. For total LDL, in group I, the mean was 132.3 ± 69.3 while in group II the mean was 77.3 ± 39.5 with P value=0.001. Triglycerides, in group I, the mean was 115.8 ± 80.4 while in group II the mean was 162.7 ± 113 with P value=0.02, (Table 4 and Figure 3).
| Lipid profile | All Participants | Low risk | High risk | P-value |
|---|---|---|---|---|
| N=100 | N=42 | N=58 | ||
| Total cholesterol | 202.4 ± 63.7 | 150.5 ± 34.7 | 240 ± 52.7 | 0.001 |
| Total HDL | 41.5 ± 13.9 | 50 ± 10.3 | 35.3 ± 12.9 | 0.001 |
| Total LDL | 132.3 ± 69.3 | 77.3 ± 39.5 | 172.1 ± 58.2 | 0.001 |
| Triglycerides | 143 ± 102.7 | 115.8 ± 80.4 | 162.7 ± 113 | 0.02 |
| LDL 4 | 16 ± 6 | 11.1 ± 4.9 | 19.6 ± 3.7 | 0.001 |
| Total VLDL | 28.6 ± 20.5 | 23.1 ± 16 | 32.5 ± 22.5 | 0.02 |
| Ratio (LDL 4/LDL) | 153 ± 1 | 12 ± 05 | 18 ± 13 | 0.003 |
| Score | 35 ± 30.8 | 6.1 ± 2.9 | 56 ± 23 | 0.001 |
Table 4: Lipid profile of patients and correlation with Gensini risk quartiles.
Regarding LDL 4, the mean in group I was 11.1 ± 4.9 while in group II it was 19.6 ± 3.7 with statistically significant p value=0.001. (LDL 4/LDL) Ratio, the mean in group I was 0.12 ± 0.05 while in group II the mean was 0.18 ± .13 with statistically significance P value=0.003 as shown in Table 4.
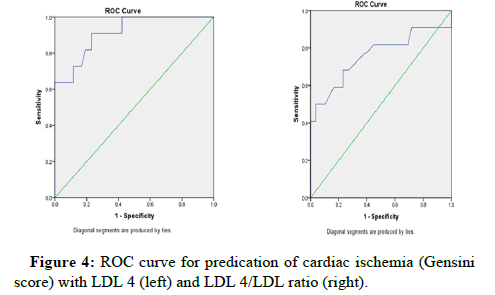
ROC curve analysis was done to pick up the best cut off value of LDL 4 in predication of severity of cardiac ischemia which was 16.7 for LDL 4 with sensitivity 90.9% and specificity 74.4% Area under the curve 0.914 p value 0.02. It was 0.163 for LDL 4/LDL ratio with sensitivity 86% and specificity 87% Area under the curve 0.902 p value 0.001, Table 5 and Figure 4.
| Best cutoff of LDL 4 | AUC | Sensitivity | Specificity | PPV | NPV | Accuracy |
|---|---|---|---|---|---|---|
| 16.7 | 0.914 | 90.9% | 74.4% | 65 | 97% | 78% |
| 0.163 | 0. 902 | 86% | 87% | 65% | 95% | 87% |
Table 5: Validity of LDL 4 and LDL 4/LDL ratio in predication of cardiac ischemia.
Finally, Table 6 shows the correlation of LDL 4 and LDL 4/LDL ratio in predication of cardiac ischemia at gensini score 37.05, it was significant with p values 0.02 and 0.001 respectively (Table 6).
Mean |
R-value |
P-value |
|
|---|---|---|---|
| LDL4/LDL ratio | 16 ± 1 | 0.617 | 0.001 |
| LDL4 | 16.05 ± 6 | 0.91 | 0.02 |
Table 6: Correlation of LDL 4 in predication of cardiac ischemia.
Discussion
Lipids can be a cause of inflammation especially with regards to the development of atherosclerotic plaque and their subsequent rupture that leads to heart attacks and Strokes Low-density lipoprotein has been identified in human atherosclerotic lesions and when complexed has been implicated as a pro-atherothrombotic antigen. Our study was conducted on 100 patients admitted at Shebin-Elkom university cathlab for coronary angiography divided into two groups according to their Gensini score. According to age in our study conducted on 100 patients with mean age 58.8 ± 8.5 years. The difference between the two groups was statistically non-significant (P-value= 0.77). This was against who study the relation between oxidized low-density lipoprotein and the presence and severity of coronary artery disease.
In our study, there was a statistical significant difference regarding hyperlipidemia (21 patients in group I and 47 patients in group II with p value 0.001) and smoking (10 patients in group I and 23 patients in group II with p value 0.004) between the two groups and nonsignificant difference regarding hypertension (25 patients in group I and 37 patients in group II with p value 0.4). This was against with who study low-density lipoprotein cholesterol as a predictor for future cardiovascular events in patients with stable coronary artery disease who underwent coronary angiography and found a statistical significant difference regarding hypertension (p value 0.012) and nonsignificant difference regarding hyperlipidemia (p value 0.486) and Smoking (p value 0.575).
In our study, there was a statistical significant difference regarding diabetes (7 patients in group I and 31 patients in group II with p value 0.0001) which was agreement with who found statistical significant difference (p value 0.001). Regarding WBCS and Blood urea nitrogen in our study there was non-significant difference (p value 0.409 and 0.45 respectively). This was agreement with who study LDL 4 as a novel predictor of coronary artery disease severity and divided 179 patients with CAD after coronary angiography to Minor to moderate CAD group and Severe CAD group and found non-significant difference between the group regarding WBCS and Blood urea nitrogen with p value 0.88 and 0.12 respectively.
Regarding platelet count and creatinine level in our study there was non-significant difference (p value 0.2 and 0.508 respectively). This was against with who divided 179 patients with CAD after coronary angiography to Minor to moderate CAD group and Severe CAD group and found significant difference between the group regarding Platelet count and creatinine level with p value<0.05 and <0.05 respectively. In our study, there was a statistical significant difference regarding Total Cholesterol (p value=0.001) and total LDL (p value=0.001).
This was against in which Blood samples were obtained immediately prior to cardiac catheterization in patients with suspected CAD. Detailed lipid profiling was performed to detect the efficacy of LDL 4 as a novel predictor of coronary artery disease severity and found a statistical non-significant difference regarding Total cholesterol (p value=0.30) and total LDL (p value=0.77). They also found a statistical significant difference regarding total HDL (p value=0.0004) and Triglycerides (p value=0.03).
This was agreement with our study in which a statistical significant difference regarding Total HDL (p value=0.001) and Triglycerides (p value=0.02) was obtained. studied the role of oxidized low-density lipoprotein in prediction of cardiac event in patients with coronary artery disease and coronary artery disease severity after diagnostic coronary angiography and found a statistical non-significant difference regarding total cholesterol (p value=0.31) and Triglycerides (p value=0.31) which was against our study results. Also found a statistical significant difference regarding total cholesterol (p value <0.0001) which was concordant with our study results.
Who study lipoprotein sub-fractions in relation with the severity of coronary artery disease assessed by gensini score and found a statistical significant difference regarding total LDL (p value=0.018) and total cholesterol (p value=0.044) which was concordant with our study results. While they found a statistical non-significant difference regarding total HDL (p value=0.531) and triglycerides (p value=0.155) which was against our study results. In our study, there was a statistical significant difference regarding LDL 4 (p value =0.001). This was agreement with who found a statistical significant difference regarding LDL 4 (p value 0.02). ROC curve analysis was done to pick up the best cut off value of LDL 4 in predication of severity of cardiac ischemia which revealed LDL 4=16.7 with sensitivity 90.9% and specificity 74.4% area under the curve 0.914 (P-value 0.02)
This was agreement with who found that patients with severe CAD had a significantly higher LDL 4, higher triglycerides and lower total HDL. They also found that LDL cholesterol analysis a cut point of >12.7 mg/dl (AUC=0.63, p=0.006) was most predictive of severe CAD by LDL 4. ROC curve analysis was done to pick up the best cut off value of LDL 4/LDL ratio in predication of Severity of Cardiac Ischemia which revealed LDL 4/LDL ratio=0.163 with sensitivity 86% and specificity 87% area under the curve 0.902 (P-value 0.001). This was agreement with who found Patients with severe CAD had significantly higher LDL 4 and triglycerides, and lower total HDL compared to patients with no/minor CAD (p<0.05 for all). Multivariate analysis showed high LDL 4 as an independent predictive of severe CAD. ROC analysis showed an area under the curve of 0.62 (p<0.0001) with a cut-point of >16.9 mg/dL to predict severe CAD with a sensitivity of 53% and specificity of 79%.
Conclusion
Cholesterol subtype (LDL 4) is significantly correlated with severity of coronary artery disease. LDL 4 is a strong independent predictor of severity of CAD than traditional cholesterol measurements. Analyzed lipoprotein particle subtraction’s and their association with angiographic progression of coronary artery disease and found a statistical significant difference regarding LDL 4 (p value=0.008) which was agreement with our study results.
Limitations
In our study, the definition of coronary arteries disease was based on angiographic views y 2 D X-ray, we did not use IVUS or FFR which may interfere with the decision of the interpretation of coronary angiography.
Recommendations
Further studies on a large number are more needed. We can use LDL 4 at the given cutoff value to predict severity of CAD.
References
- Laslett LJ, Alagona P, Clark BA, Drozda JP, Saldivar F, et al. (2012) The worldwide environment of cardiovascular disease: Prevalence, diagnosis, therapy, and policy issues: A report from the American college of cardiology. J Am Coll Cardiol 60: 1-49.
[Crossref] [Google Scholar][PubMed]
- Rehman H, Kamal AK, Morris PB, Sayani S, Merchant AT, et al. (2017) Mobile health (mHealth) technology for the management of hypertension and hyperlipidemia: Slow start but loads of potential. Curr Atheroscler Rep 19: 1-8.
[Crossref] [Google Scholar] [PubMed]
- Karathanasis SK, Freeman LA, Gordon SM, Remaley AT (2017) The changing face of HDL and the best way to measure it. Clin Chem 63: 196-210.
[Crossref] [Google Scholar] [PubMed]
- Libby P, Ridker PM, Maseri A (2002) Inflammation and atherosclerosis. Circulation 105: 1135-1143.
[Crossref] [Google Scholar][PubMed]
- Rizzo M, Pernice V, Frasheri A, Di Lorenzo G, Rini GB, et al. (2009) Small dense Low‐Density Lipoproteins (LDL) are predictors of cardio‐and cerebro‐vascular events in subjects with the metabolic syndrome. Clin Endocrinol 70: 870 875.
[Crossref] [Google Scholar] [PubMed]
- Rosenson RS, Wolff D, Tangney CC (2004) Statins reduce oxidized low-density lipoprotein levels, but do not alter soluble intercellular cell-adhesion molecule-1 and vascular cell-adhesion molecule-1 levels in subjects with hypercholesterolaemia. Clin Sci 106: 215-217.
[Crossref] [Google Scholar] [PubMed]
- Christov II, Bortolan G, Simova II, Katova T (2010) T wave and QRS complex alternans during standard diagnostic stress ECG test. Comput Cardiol 1039-1042.
- Neeland IJ, Patel RS, Eshtehardi P, Dhawan S, McDaniel MC, et al. (2012) Coronary angiographic scoring systems: An evaluation of their equivalence and validity. Am Heart J 164: 547-552.
[Crossref] [Google Scholar][PubMed]
- Gregersen I, Holm S, Dahl TB, Halvorsen B, Aukrust P (2016) A focus on inflammation as a major risk factor for atherosclerotic cardiovascular diseases. Expert Rev Cardiovasc Ther 14: 391-403.
[Crossref] [Google Scholar] [PubMed]
- Bliden KP, Chaudhary R, Lopez LR, Damrongwatanasuk R, Guyer K, et al. (2016) Oxidized low-density lipoprotein-β 2-glycoprotein I complex but not free oxidized LDL is associated with the presence and severity of coronary artery disease. Am J Cardiol 118: 673-678.
[Crossref] [Google Scholar] [PubMed]
- Nishikura T, Koba S, Yokota Y, Hirano T, Tsunoda F, et al. (2014) Elevated small dense low-density lipoprotein cholesterol as a predictor for future cardiovascular events in patients with stable coronary artery disease. J Atheroscler Thromb 21: 755-767.
[Crossref] [Google Scholar] [PubMed]
- Chaudhary R, Mathew D, Bliden K, Tantry US, Sharma T, et al. (2017) Low-density lipoprotein 4: A novel predictor of coronary artery disease severity. Curr Med Res Opin 33: 1979-1984.
[Crossref] [Google Scholar] [PubMed]
- Bliden KP, Tantry US, Pandya S, Rafeedheen R, Toth PP, et al. (2014) LDL 4-a novel predictor of coronary artery disease severity. Circulation 130: 16886-16886.
- Shimada K, Mokuno H, Matsunaga E, Miyazaki T, Sumiyoshi K, et al. (2004) Circulating oxidized low-density lipoprotein is an independent predictor for cardiac event in patients with coronary artery disease. Atherosclerosis 174: 343-347.
[Crossref] [Google Scholar] [PubMed]
- Xu RX, Li S, Li XL, Zhang Y, Guo YL, et al. (2015) High-density lipoprotein subfractions in relation with the severity of coronary artery disease: A Gensini score assessment. J Clin Lipidol 9: 26-34.
[Crossref] [Google Scholar] [PubMed]
- Williams PT, Zhao XQ, Marcovina SM, Otvos JD, Brown BG, et al. (2014) Comparison of four methods of analysis of lipoprotein particle subfractions for their association with angiographic progression of coronary artery disease. Atherosclerosis 233: 713-720.
[Crossref] [Google Scholar] [PubMed]
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi