Research Article, Int J Cardiovasc Res Vol: 8 Issue: 2
Dietary Salt Reduction in Indian Hypertensives: An Awareness Survey among Practitioners
B Krishnakumar1*, Maneesha Khalse1, Sneha Thakur2, JC Mohan3, Mainak Mukhopadhyaya4 and Bhaskar Shah5
1Department of Cardiology, Government Medical College, Trivandrum, India
2Medical Services, Medical Affairs Division, Lupin Limited, Mumbai, India
3Department of Cardiology, Jaipur Golden Hospital, New Delhi, India
5Jupiter Hospital, Mumbai, India
*Corresponding Author : B. Krishnakumr
Uthratathi House no. 2, Kailas Gardens Sreekaryam, 695017, Trivandrum, India
Tel: 91 9447345013
E-mail: 3kpillai@gmail.com
Received: February 04, 2019 Accepted: February 22, 2019 Published: February 26, 2019
Citation: Krishnakumar B, Khalse M, Thakur S, Mohan JC, Mukhopadhyaya M, Shah B (2019) Dietary Salt Reduction in Indian Hypertensives: An Awareness Survey among Practitioners. Int J Cardiovasc Res 8:2. doi: 10.417/2324-8602.1000374
Abstract
Background: There has been a considerable debate over dietary salt reduction. The objective of this survey was to understand Indian medical practitioners’ knowledge and perception on benefits of dietary salt restriction in real life setting.
Materials and methods: A prospective, cross sectional, observational, questionnaire-based survey was conducted among registered Indian practitioners. The questionnaire consisted of questions based on practitioners’ knowledge regarding the salt intake in their patients, perception on laws regarding salt restriction and awareness of their patients’ knowledge regarding salt restriction. Data was summarized by percentage graphs.
Results: A total of 674 practitioners participated in survey across India. Majority of the participants (67.8%) stated that their patients were aware of the harmful consequences of excessive dietary sodium intake. Almost 43% of doctors stated that salt added during cooking or table salt was the main source of salt in the Indian diet whereas 29% of doctors responded that salt from processed foods such as breads, noodles, etc. is the main source of salt in the Indian diet. Most doctors (49%) were aware of the WHO recommendation for dietary salt intake for an Indian adult i.e. 5 g/day. About 52% of the doctors agreed that their patients should reduce the salt intake. About 24% of doctors stated that there are no major barriers to discussing ways to reduce dietary sodium intake with hypertensive or pre-hypertensive adult patients. Approximately 40% stated lack of patient awareness, paucity of scientific evidence and non-compliance as some of the major barriers for dietary salt reduction.
Conclusion: The overall results from this survey strongly support the current public health policy for a reduction in salt intake. Another fact highlighted by this survey was that there is a paucity of well-planned education campaigns and dietary salt reduction programs in India.
Keywords: Dietary salt; Hypertensives; India; Awareness survey
Introduction
Salt is one of the most important determinants of blood pressure and cardiovascular risk across diverse geographies, ethnicities and age range. A high salt intake has other adverse effects beyond those involving the cardiovascular system, so that there is renewed interest in the relationships between high salt intake and overall human health. Cohort studies have suggested a 17% reduction in cardiovascular disease and 23% reduction in stroke when salt intake is lowered to 5 g/day or less [1].
Recent reports suggest that hypertension is one of the leading causes of global disability. [2] Meta-analysis of multiple prevalence studies, conducted by Kearney et al, stated that approximately 25% of adults worldwide suffer from hypertension [3]. It is estimated that this number will rise to 29% by 2025. Prospective Studies collaboration of a million subjects noted a direct relationship between blood pressure levels, cardiovascular and cerebrovascular mortality [4]. This finding was confirmed by the Framingham study as well [5].
An important risk factor for increased risk of hypertension documented in literature is excessive consumption of salt [6-8]. The recommended value by World Health Organization (WHO) for daily dietary salt intake is 5 g/day and <2000 mg sodium per day [9]. A sodium intake of <2300 mg/d is suggested by Canada’s 2010 Sodium Working Group [10] whereas the American Heart Association suggests sodium intake of <1500 mg/d [11]. A sodium restriction of <2300 is recommended by the recently published 2015 Dietary Guidelines for Americans [12]. The dietary food guidelines for Indians published by the Food and Agricultural Organization of the United Nations recommended that the dietary salt intake should be <2400 mg/d [13].
It is known for years that the relationship of blood pressure and salt intake is direct and progressive. Scientific literature suggests a consistent dose-response relation between blood pressure and salt intake and the range is thought to be within 3 to 12 g of salt per day. [14,15] Previously published data also suggests that a reduction of only 3 g/d may reduce blood pressure by 3.6 to 5.6/1.9 to 3.2 mmHg in hypertensive subjects and 1.8 to 3.5/0.8 to 1.8 mmHg in normotensive subjects. An ordinary reduction of 6 g in daily salt intake for around 4 weeks may decrease blood pressure by 7.11/3.88 mmHg in hypertensive individuals and 3.57/1.66 mmHg in normotensive individuals [14,15].
Scientific evidence further points out that a minute reduction of 2 g in daily salt intake over 18 months in normotensive individuals, led to a 35% reduced the incidence of hypertension at 7-year follow-up [14,16]. Whereas, for hypertensive individuals, a reduction by 4.6 g/d of salt demonstrated an average reduction in blood pressure of 5.06/2.70 mmHg [14,16].
There is limited data about knowledge, perception about benefits of dietary salt restriction in hypertensive patients among medical practitioners in India. Present survey was undertaken to explore Indian medical practitioners’ knowledge and perception on benefits of dietary salt restriction in real life setting.
Materials and Methods
Survey design and Setting
The present survey was a prospective, cross sectional, observational, questionnaire-based survey conducted across India from May 2018 to June 2018.
Survey participants
Registered medical practitioners with recognized qualification in cardiology or endocrinology (MS/MD/DM) working in public and private clinics/hospitals participated in this survey.
Survey instrument
The survey questionnaire was the main survey instrument. The questions were specially designed and structured for self-completion which was filled by the clinical practitioners based on their prior clinical experience and knowledge of salt restriction benefits in hypertensive patients. The survey assessed the practitioners’ knowledge, attitude and perception towards dietary salt restriction in hypertensive patients. The questionnaire consisted of questions based on practitioners’ knowledge regarding the salt intake in their patients, perception on laws regarding salt restriction and awareness of their patients’ knowledge regarding salt restriction.
Data analysis
Data was summarized categorically by number ‘N’ and percentage (%) in each category where ‘N’ represents total number of participants responding to each question. Data was interpreted and summarized in graphs. A few participants have responded to more than one option for some of the questions and some participants did not answer all the questions.
Ethical considerations
As this was a survey where no patient related data was captured hence ethics committee approval was not essential and so not obtained. Likewise, since this was not a clinical trial, clinical trial registration was not needed.
Results
A total of 674 practitioners participated in survey across India. Final data of 674 participants’ responses were evaluated and analyzed as follows:
Majority of the participants (67.8%) stated that their patients were aware of the harmful consequences of excessive dietary sodium intake; whereas only 24.9% practitioners were of the opinion that their patients were unaware of consequences of excessive sodium intake (Figure 1).
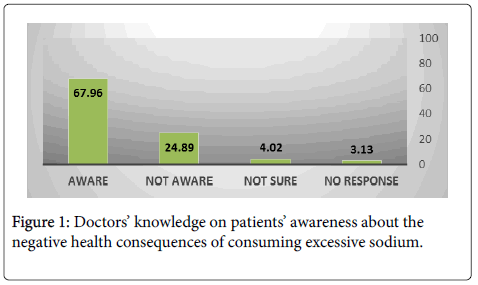
Figure 1: Doctors’ knowledge on patients’ awareness about the negative health consequences of consuming excessive sodium.
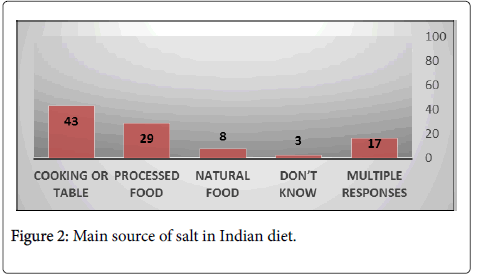
Figure 2: Main source of salt in Indian diet.
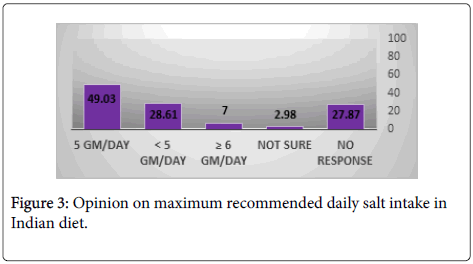
Figure 3: Opinion on maximum recommended daily salt intake in Indian diet.
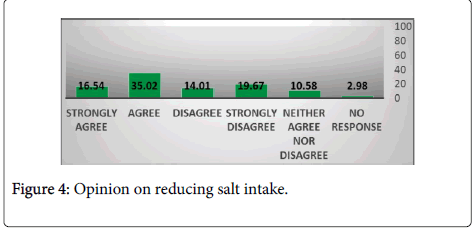
Figure 4: Opinion on reducing salt intake.
About 24% of doctors stated that there are no major barriers to discussing ways to reduce dietary sodium intake with hypertensive or pre-hypertensive adult patients. Approximately 23% doctors stated lack of patient awareness, 15% stated paucity of scientific evidence and 12% mentioned non-compliance as some of the major barriers for dietary salt reduction (Figure 5).
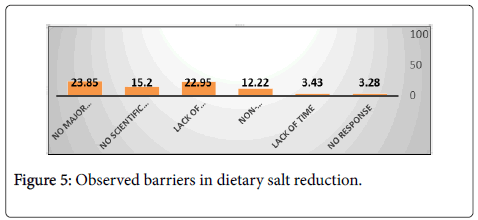
Figure 5: Observed barriers in dietary salt reduction.
Approximately 53% doctors were in agreement with the fact that there should be laws governing addition of salt in manufactured foods (Figure 6). Total 49% of doctors agreed that it is difficult to understand sodium information displayed in food labels (Figure 7). Almost 68% doctors were of the opinion that when eating out at restaurants/cafes/ pubs, lower salt options are not readily available or available only in limited variety (Figure 8).
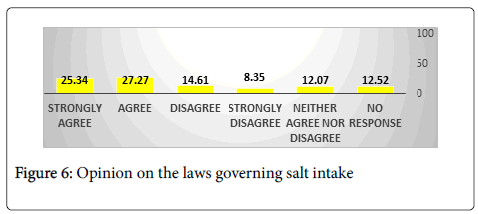
Figure 6: Opinion on the laws governing salt intake
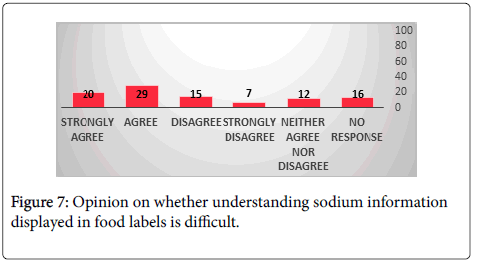
Figure 7: Opinion on whether understanding sodium information displayed in food labels is difficult.
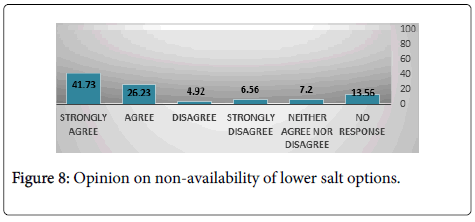
Figure 8: Opinion on non-availability of lower salt options.
Discussion
To the best of our knowledge, no randomized controlled trials have studied the effect of reducing the salt intake of populations on cardiovascular disease and overall mortality. However, the link is strong and generally accepted by the physicians and regulatory authorities. Although, the argument for reduction in salt intake to prevent cardiovascular disease is strong, physicians’ attitude towards salt intake plays a major role. This study focuses on the knowledge, attitude and practices of the physicians with regard to reducing salt intake in their patients.
Over years, there has been a considerable debate on dietary salt reduction leading to what is known as ‘salt controversy’. Clear evidence indicates that reduction of salt intake lowers blood pressure and reduces the risk of hypertension and other cardiovascular disease (CVD). The WHO has recommended a population-wide target of reducing intake of salt from present level of 10 g daily to <5 g per day [17]. This recommendation has been challenged by several studies, including cohort studies, which have suggested a J-shaped relationship between salt intake and CVD risk [17]. However, these studies were associated with several methodological problems, like reverse causality and assessment of salt intake by spot urine which led to measurement errors [17]. In light of the available evidence, measured and continuous salt reduction as recommended by the WHO remains a feasible and effective method to prevent the risk of hypertension.
There is limited data on dietary salt reduction in the Indian scenario. Therefore, present survey was undertaken to understand current knowledge, attitude and practices of Indian practitioners related to dietary salt reduction. To the best of our knowledge, this is the first ever survey on dietary salt reduction in hypertensive in Indian scenario.
Majority of the participants stated that their patients were aware of the harmful effects of excessive dietary salt consumption. According to most participants, salt added during cooking or table salt is the main source of salt in the Indian diet whereas few of the participants responded that salt from processed foods such as breads, noodles, etc. is the main source of sat in the Indian diet. This finding is in agreement with previous reports of dietary salt in Indian scenario [18,19].
As regards to the opinion of practitioners towards dietary salt reduction, almost half of study participants were in agreement with the WHO recommendation of dietary salt reduction whereas a third of participants did not support dietary salt reduction. This finding may be due to the existing salt controversy misleading practitioners and patients. However, one must consider results from previously published reports that have demonstrated a direct relationship between a reduction in salt intake and a fall in systolic BP [19-21]. The entirety of the scientific evidence strongly encourages a reduction in salt intake and the salt controversy must not discourage patients from reducing dietary salt [19].
Major barriers for reducing the salt intake reported in the present survey were lack of strong evidence, lack of patient education tools, poor patient compliance. These barriers could be overcome by conceptualizing and executing various salt reduction programs thereby creating a platform for patient education and motivate them to restrict dietary salt.
The UK has pioneered a successful salt-reduction program undertaken under joint leadership of Consensus Action on Salt and Health (CASH; a nongovernmental organization) and the Food Standards Agency (a quasi-governmental organization). This deal warrants a ‘level playing field’ for the food industry as all the major food and nutrition companies would have to aim for the similar targets. A sizeable progress has been made since the program was initiated, and the salt content in many foods has been reduced by 20–50% [19].
A similar 3-year initiative called ‘A National Salt Reduction Program for India’ has been undertaken to develop the awareness required to design a nation-wide dietary salt reduction program. The program is structured to develop an elaborate policy response and action plan by the Indian government, covering stores, street vendors, chain restaurants, food manufacturers and consumers. The sodium content would be reduced and the information on the labels would be easier to understand [22].
Conclusion
The overall evidence strongly supports the current public health policy for a reduction in salt intake. The result from the present survey is in accordance with this finding. An interesting fact highlighted by this survey was that there is a paucity of well-planned education campaigns and dietary salt reduction programs to overcome the barriers in achieving the WHO recommended daily salt intake. This makes it extremely important to have more robust initiatives in collaboration with the food industry dedicated to dietary salt reduction.
References
- Strazzullo P, D’Elia L, Kandala NB, Cappuccio FP (2009) Salt intake, stroke, and cardiovascular disease: meta-analysis of prospective studies. BMJ 339: b4567.
- DiNicolantonio JJ, Mehta V, O'Keefe JH (2017) Is salt a culprit or an innocent bystander in hypertension? A hypothesis challenging the ancient paradigm. Am J Med 130: 893-899.
- Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, et al. (2005) Global burden of hypertension: analysis of worldwide data. Lancet 365: 217-223.
- Lewington S, Clarke R, Qizilbash N, Peto R, Collins R (2002) Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 360: 1903-1913.
- Vasan RS, Larson MG, Leip EP, Evans JC, O'Donnell CJ, et.al. (2001) Impact of high-normal blood pressure on the risk of cardiovascular disease. N Engl J Med 345: 1291-1297.
- Frohlich ED, Varagic J (2005) Sodium directly impairs target organ function in hypertension. Curr Opin Cardiol 20: 424-429.
- Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, et.al. (2001) Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med 344: 3-10.
- Meneton P, Jeunemaitre X, de Wardener HE, MacGregor GA (2005) Links between dietary salt intake, renal salt handling, blood pressure, and cardiovascular diseases. Physiol Rev 85: 679-715.
- Amine EK, Baba NH, Belhadj M, Deurenberg-Yap M, Djazayery A (2002) Diet, Nutrition and the prevention of chronic diseases. WHO.
- Hutchinson H, Campbell N, L’Abbe ML, Tanaka P (2010) Sodium reduction strategy for Canada: recommendations of the Sodium Working Group. Canada.
- Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, et.al. (2010) Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic Impact Goal through 2020 and beyond. Circulation 121: 586-613.
- US Department of Agriculture and US Department of Health and Human Services (2015) Dietary Guidelines for Americans, 2015-2020. 8th ed. Washington, DC: US Government Printing Office, USA.
- National Institute of Nutrition (1998) Dietary Guidelines for Indians: a manual, India.
- Frisoli TM, Schmieder RE, Grodzicki T, Messerli FH (2012) Salt and hypertension: is salt dietary reduction worth the effort? Am J Med. 125: 433-439.
- He FJ, MacGregor GA (2002) Effect of modest salt reduction on blood pressure: a meta-analysis of randomized trials. Implications for public health. J Hum Hypertens 16: 761.
- He FJ, Li J, MacGregor GA (2013) Effect of longer term modest salt reduction on blood pressure: Cochrane systematic review and meta-analysis of randomised trials. Bmj 346: f1325.
- He FJ, MacGregor GA (2018) Role of salt intake in prevention of cardiovascular disease: controversies and challenges. Nat. Rev. Cardiol 15: 371-377.
- Dhemla S, Varma K (2015) Salt intake in India-an alarming situation. Int J Food Agric Vet Sci 5:1-0.
- Mushoriwa F, Rath S, Mabika N, Bosman SJ, Srinivas SC (2016) Dietary Salt Reduction: A Glance at India and South Africa. IJOPP 9: 107.
- Aburto NJ, Ziolkovska A, Hooper L, Elliott P, Cappuccio FP, et al. (2013) Effect of lower sodium intake on health: systematic review and meta-analyses. BMJ 346: f1326.
- Mozaffarian D, Fahimi S, Singh GM, Micha R, Khatibzadeh S, et.al. (2014) Global sodium consumption and death from cardiovascular causes. N Engl J Med 371: 624-634.
- Kannan Krishnaswamy (2014) A National Salt Reduction Program for India. The George Institute For Global Health. India.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi 



