Research Article, Androl Gynecol Curr Res Vol: 6 Issue: 1
Dysthyroidism in Diabetic Pregnant Women
Nadia Ben Amor*, Chaïma Jemaï, Hajer Tertek, Aroua Temesk, Meriem Zarrouk and Faïka Ben Mami
Department C, National Institute of Nutrition and Food Technologies, Tunis, Tunisia
*Corresponding Author : Nadia Ben Amor
Department C, National Institute of Nutrition and Food Technology, Tunis, Tunisia
Tel: (+216) 98425170
E-mail: bestnadou@yahoo.fr
Received: January 04, 2018 Accepted: January 24, 2018 Published: January 30, 2018
Citation: Ben Amor N, Jemaï C, Tertek H, Temesk A, Zarrouk M, et al. (2018) Dysthyroidism in Diabetic Pregnant Women. Androl Gynecol: Curr Res 6:1. doi: 10.4172/2327-4360.1000160
Abstract
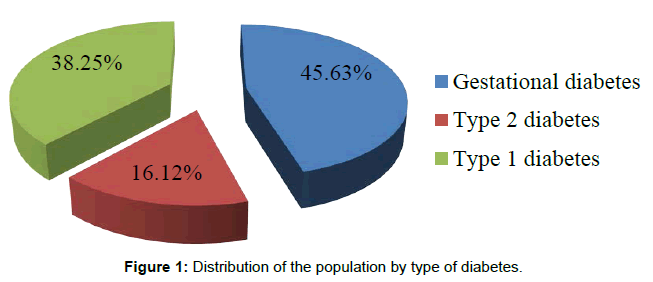
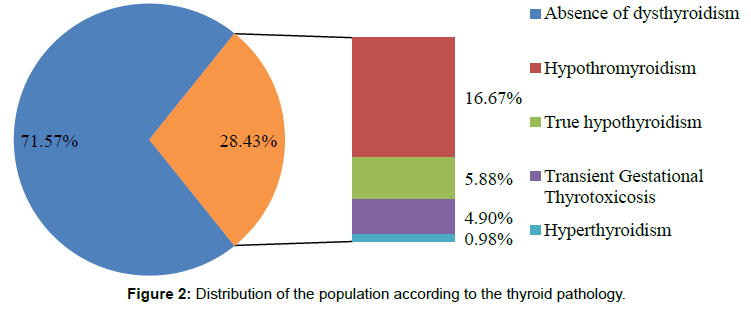
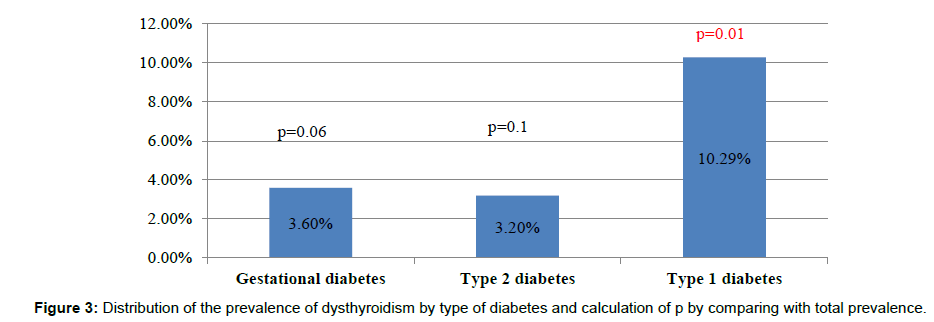
Introduction: Dysthyroidism is more commonly found in pregnant women, especially diabetic parturients. The purpose of this study was to evaluate the prevalence of thyroid pathologies in diabetic pregnant patients. Patients and methods: A descriptive study that included 204 diabetic parturients (type 1 diabetes, type 2 diabetes and gestational diabetes) who received a systematic TSH and FT4 assay. Results: Mean age of the population = 31.4 ± 4.6 years. Type 1 diabetes = 16.12%; Type 2 diabetes = 38.25% and gestational diabetes = 45.63%. The total prevalence was 28.43%. Subclinical hypothyroidism was present in 16.67% of cases, true hypothyroidism in 5.88%, transient gestational thyrotoxicosis in 4.90% and hyperthyroidism in 0.98%. Conclusions: The most common pathology is mild hypothyroidism and type 1 diabetics are those with the most dysthyroidism. There remains the question of systematic screening among other diabetic parturients.
Keywords: Diabetic pregnancy; Dysthyroidism; Screening
Abbreviations
TSH: Thyroid Stimulating Hormone; FT4: Free Thyroid Hormone 4; Hcg: Human Chorionic Gonadotropin Hormone; ATPO: Anti-Thyroid Peroxidase Antibodies
Introduction
Thyroid diseases are the most common endocrine pathologies in women of childbearing age. Their prevalence is significantly increased during pregnancy, especially in diabetic patients [1]. Indeed, pregnancy is characterized by different hormonal adaptations with particular elevation of different hormones. In addition, there is an increase in metabolic needs and changes in the immune system that may be a factor of deregulation or revelation of these thyroid diseases, the lack of correct management can lead to deleterious maternal-fetal consequences [2]. The purpose of our work is to systematically screen for dysthyroidism in diabetic patients followed in our department to assess the prevalence of thyroid diseases during diabetic pregnancy.
Patients and Methods
This is an observational descriptive study of 204 diabetic pregnant patients followed in the C department of the National Institute of Nutrition and Food Technologies from January 2013 until October 2017.
Inclusion criteria
Pre-Pregnancy Diabetes, Gestational Diabetes.
Criteria for non-inclusion
Thyroid pathology known before pregnancy, taking medications that may interfere with the thyroid. All patients had systematically benefited from a thyroid test (FT4/TSH). The evaluation of thyroid status referred to the 2012 recommendations made by the American Association of Clinical Endocrinologists in cooperation with the American Thyroid Association [3]. The statistical analysis of the results was carried out by the SPSS software version 20. The comparison of two qualitative variables was carried out by the Chi-square test with a significance threshold retained at 0.05.
Results
The mean age of our patients was 31.4 ± 4.6 years with extremes ranging from 20 to 41 years (Figure 1). Mean diabetes progression was 14.8 ± 3.5 years with extremes ranging from 2 to 17 years. Diabetic retinopathy was found in 7.84% (n = 16) of our patients; nephropathy in 5.39% (n = 11) and neuropathy in 0.98% (n = 2). No macroangiopathy was noted (Figure 2). Family history of thyroid pathologies was noted in 14.71% of our total population (n = 30 of 204) and in 17.24% of parturient with dysthyroidism (n = 10 of 58) with a statistically insignificant difference (p = 0.06) (Figure 3).
Discussion
The physiological changes in thyroid status observed during pregnancy are a transient and relative increase in FT4 in parallel with the increase in hCG in the first trimester and then an average decrease in FT4 levels. Approximately 15% which can be amplified in case of iodine deficiency [4]. The TSH assay is the first-line test considered to be the most effective for determining the thyroid status of a pregnant patient. The elevation of hCG in early pregnancy leads to a decrease in TSH or even its physiological suppression (around the tenth week of amenorrhea) in about 20% of pregnant women [5]. It is therefore necessary for the pregnant woman to have reference intervals adapted to the stage of pregnancy [6]. US recommendations suggest these normality values: 1st quarter 0.1-2.5 mIU/L, 2nd quarter 0.2-3.0 mIU/L and 3rd quarter 0.3-3.0 mIU/L [3]. In our study, 28.43% was the total prevalence of thyroid diseases in 204 diabetic parturients (gestational diabetes, type 1 diabetes, and type 2 diabetes). This high prevalence is consistent with many studies, such as Moreno-Reyes, which had detected all thyroid pathology in first trimester pregnant women in 55 obstetrical clinics and found 18.6% [7].
In order of decreasing frequency, the dysthyroidism found in our work was crude hyperthyroidism, then true hypothyroidism, then transient gestational thyrotoxicosis, and lastly, frank hyperthyroidism. Hypothyroidism was noted in our study in 16.67% and 5.88% respectively for the infra-clinical form and the frank form. In the literature, during diabetic pregnancy, the prevalence of hypothyroidism varies between 5 and 16%. In type 1 diabetics in the Netherlands, it is 4.9% and that of subclinical hypothyroidism is 18.3% [8]. Indeed, the recent modification of the higher standards of TSH during pregnancy, results in a significant increase in this prevalence. Similarly, iodine deficiency in the mother may explain hypothyroidism. As a result, the World Health Organization recommends 200 to 300 μg daily for iodine and 250 μg for the Endocrine Society [9,10]. Transient gestational thyrotoxicosis was found in 4.90% of our patients. This pathology is related to excessive stimulation of the hCG receptor by the TSH at concentrations at least greater than 200 000 IU/L [11]. In the literature, its prevalence is on average 3% [12]. As for free hyperthyroidism, 0.98% of our parturient had Graves’ disease, the main symptomatology of which was sweating, severe vomiting and weight loss or lack of weight gain. The diagnosis was confirmed by collapsed TSH, increased free thyroid hormones and the presence of anti-TSH receptor antibodies. This prevalence is consistent with many other studies that showed that hyperthyroidism was found in 1.7% of type 1 diabetics and 0.3% of type 2 diabetics (0.1% to 0.6% excluding diabetes) [13]. Following these percentages obtained on a series of 204 diabetic parturients, the dysthyroidies seem to be a pathology rather found during the pregnancy, in particular the subclinical forms. In addition, these thyroid diseases were more frequently present in type 1 diabetic parturients than type 2 or in gestational diabetes with a significant difference (p = 0.01). This is due, among other things, to the disruption of the immune system, particularly in women with autoimmune diabetes. Therefore, it is recommended to dose before and at the beginning of pregnancy with type 1 diabetes, TSH and ATPO antibodies [3]. For type 2 diabetes and gestational diabetes, the risk is lower and screening is not currently recommended.
Conclusions
Our results showed an increased prevalence of silent thyroid disorders during diabetic pregnancy, particularly hypothyroidism in type 1 diabetics. Systematic screening of these patients is well established by international recommendations. However, the question still arises in other diabetic and non-diabetic parturients. It would be necessary to carry out other studies of the prevalence of dysthyroidism in all pregnant women, diabetic or not, and whatever the type of diabetes, in order to lay down the screening procedures during pregnancy.
Conflict of Interest
There is no conflict of interest.
References
- Caron P (2009) Prevention of thyroid disorders in pregnant women. J Gynecol Obstet Biol Reprod 38: 574-579.
- Glinoer D, De Nayer P, Bourdoux P, Lemone M, Robyn C, et al. (1990) Regulation of maternal thyroid during pregnancy. J Clin Endocrinol Metab 71: 276-287.
- Garber JR, Cobin RH, Gharib H, Hennessy JV, Klein I, et al. (2012) Clinical Practice Guidelines for Hypothyroidism in Adults: Cosponsored by the American Association of Clinical Endocrinologists and the American Thyroid Association. Endocr Pract 18: 988-1028.
- Ducarme G, Bertherat J, Vuillard E, Polak M, Guibourdenche J, et al. (2007) Pregnancy and thyroid disorders. Rev Med Interne 28: 314-321.
- Negro R, Stagnaro-Green A (2014) Clinical aspects of hyperthyroidism, hypothyroidism, and thyroid screening in pregnancy. Endocr Pract 20: 597-607.
- Stricker R, Echenard M, Eberhart R, Chevailler M-C, Perez V, et al. (2007) Evaluation of maternal thyroid function during pregnancy: the importance of using gestational age-specific reference intervals. Eur J Endocrinol 157: 509-514.
- Moreno-Reyes R, Glinoer D, Van Oyen H, Vandevijvere S (2013) High prevalence of thyroid disorders in pregnant women in a mildly iodine-deficient country: a population-based study. J Clin Endocrinol Metab 98: 3694-3701.
- Gallas EDM, Stolk RP, Bakker K, Endert E, Wiesinga WM (2002) Thyroid dysfunction during pregnancy and in the first year postpartum in women with diabetes mellitus type 1. Eur J Endocrinol 147: 443-451.
- De Groot L, Abalovich M, Alexander EK, Amino N, Barbour L, et al. (2012) Management of thyroid dysfunction during pregnancy and postpartum: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 97: 2543-2565.
- WHO Secretariat, Andersson M, de Benoist B, Delange F, Zupan J (2007) Prevention and control of iodine deficiency in pregnant and lactating women and in children less than 2-years-old: conclusions and recommendations of the technical consultation. Public Health Nutr 10: 1606-1611.
- Lockwood CM, Grenache DG, Gronowski AM (2009) Serum human chorionic gonadotropin concentrations greater than 400,000 IU/L are invariably associated with suppressed serum thyrotropin concentrations. Thyroid 19: 863-868.
- Negro R, Stagnaro-Green A (2014) Clinical aspects of hyperthyroidism, hypothyroidism, and thyroid screening in pregnancy. Endocr Pract 20: 597-607.
- Vérier-Mine O, Dorey F, Bacri JL, Quiquempois H (2012) Diabète et grossesse. EMC - Endocrinologie-Nutrition 9: 1-9.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi