Research Article, Androl Gynecol Curr Res Vol: 5 Issue: 4
Evaluating the Outcome of Conventional Tese from Clinical Presentation in Patients with Non-Obstructive Azoospermia
Marialva CF*, Ramos NA, Rosa JP, Metello JL, Ramos SI and Melo PS
Department of Urology, Infertility and Medically Assisted Reproduction Center, Garcia de Orta Hospital, Almada, Portugal
*Corresponding Author : Marialva CF
Department of Urology, Infertility and Medically Assisted Reproduction Center, Garcia de Orta Hospital, Almada, Portugal
Tel: +351-963048519
E-mail: celsomarialva@gmail.com
Received: December 04, 2017 Accepted: December 18, 2017 Published: December 23, 2017
Citation: Marialva CF, Ramos NA, Rosa JP, Metello JL, Ramos SI (2017) Evaluating the Outcome of Conventional Tese from Clinical Presentation in Patients with Non-Obstructive Azoospermia. Androl Gynecol: Curr Res 5:4. doi: 10.4172/2327-4360.1000159
Abstract
Context: Several etiologies have been identified and some clinical factors might predict the probability of finding sperm in nonobstructive azoospermia (NOA). Aims: Find and correlate the clinical findings to the success of testicular sperm extraction (TESE). Settings and Design: Retrospective review of patients with NOA undergoing TESE in our department between 2012 and 2015. Methods and Material: We analyzed the sperm retrieval rate (SRR) based on testicular size, Follicle-Stimulating Hormone (FSH), Luteinizing Hormone (LH), total testosterone and prolactin levels as well as on the karyotype findings. We also report the results of ICSI based on clinical features. Statistical analysis used: Mann-Whitney U test; chi-square test; receiving operating characteristic and area under the curve; binary logistic regression. Results: 54 patients, mean age of 34, 57 years. The overall SRR was 51, 9%. Difference between negative and positive SRR regarding mean FSH (p=0,002) and mean LH (p=0,007) was found. No difference in SRR based on karyotype findings (p=0.127) or testicular size (p=0,336) was identified. A multivariate binary regression concluded that only FSH could be used as a predictor for TESE+. A FSH value <11,0UI/L was associated with an OR of 19 for TESE+ result (95% CI 4.1-87.6). With FSH <11,0UI/L the probability of TESE+ increases to 85% and if FSH>11,0UI/L the probability of TESE+ will be 24%. 28 patients proceeded to ICSI with clinical pregnancy and live birth rates of 20,7% and 17,2%. Conclusions: NOA patients should be fully assessed and informed about the probability of TESE+; FSH levels alone might be useful to do that. Furthermore those with normal FSH and normal testicular size can expect higher rates of sperm retrieval and live birth after ICSI.
Keywords: Azoospermia; FSH; Primary infertility; Sperm retrieval rate; Intracytoplasmic sperm injection
Introduction
Azoospermia affects 1% of the male population [1,2]. Nonobstructive azoospermia (NOA) is diagnosed in 60% of azoospermic men and represents the absence of spermatozoa in semen because of minimal or no spermatogenesis [2,3]. Several etiologies for NOA were recognized like genetic disorders, cryptorchidism, testicular torsion, radiation and toxins [4-10]. Testicular volume, FSH and inhibin B levels have been used in prediction models but none was validated externally [11-19]. It would be of great value to estimate an individual’s chance of sperm retrieval to empower patients in their decision-making. We report the results of c-TESE and the SRR, correlating them to the anatomical, laboratory and karyotype findings in the patients studied. Additionally we analyze the results of ICSI in the c-TESE positive cases.
Materials and Methods
Patients
The study consisted of a retrospective review of 54 patients with NOA who underwent TESE in our department between January 2012 and December 2015. These cases presented to a single consultant urological surgeon with a single senior clinical embryologist. Each patient underwent physical examination, semen analysis, and endocrinologic evaluation. Physical examination was performed during the first examination of each patient. Due to the lack of orchidometers in every doctor’s office of our department, we measured the long axis of the testes as reference. To standardize the evaluation we considered as small testis all the reports where the major axis of testes was less than 4 cm long.
Semen analyses were performed on at least two separate occasions for each patient, and the evaluation was performed according to the methods described in the World Health Organization guidelines of 1999. Endocrinologic evaluation included assays of serum FSH, LH, total testosterone and prolactin levels. Chromosomal analysis was performed using peripheral blood lymphocyte cultures, and following the standard protocol of Giemsa banding. Additional chromosome banding (other than Giemsa banding) and fluorescent in situ hybridization were performed to analyze mosaicism. Screening for azoospermia factor (AZF) microdeletions was performed in all patients. We also report the fertilization cycles, clinical pregnancies and live birth rates based on the medical records of the infertility center for these patients. Approval of the ethics committee for the conduction of the present study was obtained.
Tese procedure
A TESE procedure was performed in 1-day surgery clinic under general anesthesia. A prophylactic antibiotic treatment was given and 1 week later the patients were all rechecked at outpatient clinic. A small (3.5 cm) incision was made longitudinally on the median raphe, and the incision carried down through the fascia over the largest testicle or, in case of equal volume, the testicle with the better consistency. Thereafter, the tunica vaginalis was opened and, if necessary, the testis luxated outside the scrotum. The tunica albuginea was longitudinally incised; the length of each tunica albuginea incision was 0,5cm. A longitudinal biopsy over the whole length was taken and immediately transported to the fertility laboratory. The biopsy was then subjected to mechanical dissection and cells present in the lumen of the tubules were extracted. The obtained cell suspension was directly examined for the presence of spermatozoa. One other site of testis was similarly biopsied, while the first biopsy has been evaluating.
Second side biopsy was performed if first side sperm harvest was negative. In two patients we found sperm on the second side after a negative first side biopsy. Only with two negative biopsies in each testis allowed us to say that the TESE result was negative. When the yielding spermatozoa biopsy site has been identified, additional tissue was harvested, their number and motility were noted, and the cell suspension was cryopreserved.
Statistical analysis
Statistical evaluation was performed using the Statistical Package for the Social Sciences (SPSS Inc; Chicago, IL, USA) software program version 22.0, and p<0.05 was considered to be statistically significant. Data of statistical analysis is presented as mean ± standard deviation (min-max). In pairwise intergroup comparisons between hormones values Mann-Whitney U test was used. In the evaluation of data concerning testicular size and karyotype findings chi-square test was used. To find the best cut off value of FSH to predict the TESE result we plotted the variable based on TESE results. Additionally ROC (Receiving Operating Characteristic) and area under the curve were calculated and a binary logistic regression was performed and analyzed.
Results
When patients with obstructive type azoospermia and/or those could not be diagnosed as NOA because of missing data were ruled out, presumptive initial diagnosis of NOA was made and the patients were included in this study. Obstructive azoospermia was ruled out by physical exam: vas deferens gross consistency and diameter; and also by semen analysis based on sperm volume and pH. In our laboratory normal FSH levels were accepted as 1,5-10,0 IU/L, while mean FSH level of the patients in our study group was relatively higher: 15,59 ± 13,71 (1,60-78,7) IU/L. The same was observed in LH, with normal values accepted as 1,7-8,6 IU/L and the mean LH level in our sample lightly increased: 9,00 ± 9,27 (1,8- 54,4) IU/L. Mean values for prolactin, and free testosterone were within normal limits.
All demographic data is shown in Table 1. We found statistical difference between negative vs. positive SRR regarding mean FSH (19,88 vs 11,81 IU/L; p = 0,002) and mean LH (10,83 vs 7,39 IU/L; p=0,007) as shown below (Table 2). No statistical difference was observed in other variables. Karyotype analysis and comparative values are shown in Table 3. No statistical significance was found in terms of SRR based on karyotype findings in our patients (p=0.127). There was no difference in sperm retrieval rate between normal and small testes (p=0,336) (Table 4).
| Patients (n) | 54 |
| Age, years; mean ± SD (min-max) | 34,57 ± 4,14 (26-45) |
| Sperm retrieval rate, % | 51,9 (28/54) |
| FSH, IU/L; mean ± SD (min-max) | 15,59 ± 13,71 (1,60-78,7) |
| LH, IU/L; mean ± SD (min-max) | 9,00 ± 9,27 (1,8-54,4) |
| Testosterone, ng/dL; mean ± SD (min-max) | 331,36 ± 192,89 (1,70-900,0) |
| Prolactine, ng/mL; mean ± SD (min-max) | 11,33 ± 6,59 (4,10-33,90) |
| Patients with history of varicocele; n (%) | 3 (5,9%) |
| Patients with small testes; n (%) | 6 (11,1%) |
| Patients with karyotype abnormality; n (%) | 7 (13,0%) |
Table 1: Demographic data and baseline characteristics of enrolled patients.
| TESE Negative | TESE Positive | P | |
|---|---|---|---|
| FSH, UI/L | 19,88 ± 9,30 (1,7-37,6) | 11,81 ± 15,90 (1,6-78,7) | 0,002 |
| LH, UI/L | 10,83 ± 7,69 (2,4-35,6) | 7,39 ± 10,35 (1,8-54,4) | 0,007 |
| Testosterone, ng/dL | 295,11 ± 203,00 (4,9-900,00) | 362,88 ± 182,22 (1,7-752,0) | 0,233 |
| Prolactine, ng/mL | 11,34 ± 3,01 (6,6-14,9) | 11,33 ± 8,43 (4,1-33,9) | 0,261 |
| Age, years | 34,31 ± 3,66 (27-40) | 34,82 ± 4,60 (26-45) | 0,917 |
Table 2: Comparison of hormonal levels and age within TESE positive and negative cases.
| Patients, n (%) n=54 | Patients with positive SRR, n (%) | ||
|---|---|---|---|
| AZFc microdeletion | 1 (1,9%) | 1 (100) | X2=4,130 p=0,127 |
| Klinefelter (47,XXY) | 6 (11,1) | 1 (16,7) | |
| Normal (46,XY) | 47 (87,0) | 27 (56,2) |
Table 3: Sperm retrieval rates based on patient karyotype.
| Patients, n (%) n=54 | Patients with positive SRR, n (%) | ||
|---|---|---|---|
| Atrophic | 6 (11,1) | 2 (33,3) | X2=0,927 p=0,336 |
| Normal | 48 (88,9) | 24 (50,0) |
Table 4: Sperm retrieval rates based on testes size.
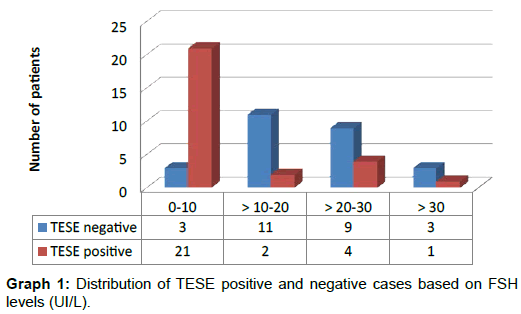
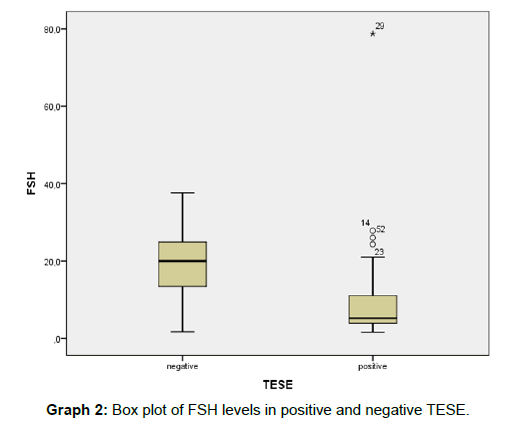
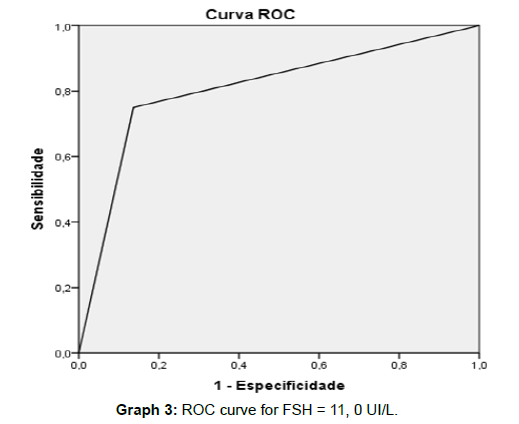
Distribution of TESE results with respect to follicle stimulating hormone levels is shown in Graph 1. We plotted the FSH values based on the TESE result (Graph 2): Based on the analysis of this graph we calculated the best cut off value for FSH to predict the positivity of TESE and we obtained 11,0 UI/L. With this cut off value we have a sensitivity of 75% and a specificity of 86% to predict the TESE result with area under the curve equals to 0,807 (Graph 3). Then a binary logistic regression was calculated with FSH variable categorized in ≤11UI/L and >11UI/L with statistical significance explored in the discussion chapter (Table 5). A total of twenty eight patients proceeded to ICSI, and 29 cycles were performed. We divided them in 4 groups based on FSH levels and testes size. There were 6 clinical pregnancies, a clinical pregnancy rate (CPR) per cycle of 26% in the highest SRR group. Two pregnancies (33,3%) resulted in miscarriage. There were 5 live births, including 2 twin births, a live birth rate (LBR) per ICSI cycle of 17,2% (Table 6). In this study, no severe complications, such as acute epididymitis, scrotal haematoma and testicular hydrocele were reported, and, at this time of follow-up, no patients required hormone replacement therapy for post-operative hypogonadism.
| B | S.E. | Wald | df | Sig. | Exp(B) | 95% C.I. to Exp(B) | ||
|---|---|---|---|---|---|---|---|---|
| Inferior | Superior | |||||||
| FSH | 2,944 | 0,780 | 14,255 | 1 | 0,000 | 19,000 | 4,120 | 87,614 |
| Constant | -1,153 | 0,468 | 6,059 | 1 | 0,014 | 0,316 | ||
Table 5: Binary logistic regression with categorical FSH (=11UI/L vs. >11UI/L).
| Patients | Adequate sperm retrieval | ICSI cycles | Clinical Pregnancy | Live births | |
|---|---|---|---|---|---|
| Normal FSH, normal testes | 23 | 87,0% (20/23) | 19 | 5 | 5 |
| Increased FSH, normal testes | 25 | 24,0% (6/25) | 6 | 1 | 0 |
| Normal FSH, atrophic testes | 1 | 100% (1/1) | 2 | 0 | 0 |
| Increased FSH, atrophic testis | 5 | 20% (1/5) | 2 | 0 | 0 |
| Total | 54 | 51,9% (28/54) | 29 | 6 | 5 |
Table 6: Sperm retrieval rates, clinical pregnancies and live births for clinical subgroups of patients with normal and abnormal FSH or testicular size. Normal testicular size was considered to be ≥ 4 cm, and normal FSH ≤10 IU/L.
Discussion
To date, NOA subjects may retrieve spermatozoa through TESE, giving the chance for an assisted reproductive technology process [20-22]. TESE combined with ICSI is the first-line treatment in NOA patients. In various studies performed, an average sperm retrieval rate of 59% has been reported using TESE similar to our study (51, 9%) [23]. Micro-TESE was developed with the aim to minimize testicular tissue loss and increase the rate of sperm retrieval [24]. Successful SRR in TESE ranges between 16.7 and 62%, whereas in micro-TESE positive SRR varies between 43 and 63% [25]. Therefore, there is still a debate in literature between these techniques, and, to date, no significantly robust data sustain the micro-TESE superiority. There are different SRRs between c-TESE and micro-TESE based on testis histology with significant difference for micro-TESE in hypospermatogenesis [19]. However, in that group sperm can be found by conventional biopsy since there are sperm distributed throughout the testes. In the Sertoli Cell only group mTESE has a significant advantage because spermatogenesis may be very focal.
Nevertheless, it should be considered that mTESE requires magnification equipment, which means higher costs, longer operative times and it is associated with a significant learning curve. Therefore, considering the overall SRR, multiple c-TESE might still represent the first-line approach to selected NOA patients. The most appropriate number of biopsies to be performed still remains controversial. To increase the chance of finding a focus of sperm production, it is advisable to take multiple samples from different sites of the testis. Furthermore, the multiple TESE approach is related to a significantly higher SRR, when compared with single TESE (49% vs. 37.5%) [26]. As no specific location in the testis was more likely to contain spermatozoa, multiple TESE has been recommended, as we perform in our center, with two biopsies of each testis [22]. Nowadays, there is still no possibility to predict the TESE outcome in NOA on the basis of simple clinical non-invasive parameters [27]. At the initial consultation, couples often want to know the preoperative likelihood of SRR success achieved by TESE [4-6]. In a recent metaanalysis, inhibin B was investigated as non-invasive marker of active spermatogenesis. Inhibin B resulted the most predictive of the spermatozoa presence, as higher level of specificity and sensibility, but not enough to be considered as one independent marker of spermatogenesis in men with NOA [28]. Diagnostic testicular biopsy has been the prognostic marker with the highest predictive value. Presence of mature spermatids has been defined as the best marker for the presence of mature spermazoa [29]. As histology is rarely obtained prior to treatment in current practice, there is a need for clinical parameters that can be used to predict the success of SSR.
FSH and testicular size are both associated with maturation arrest, and testicular failure [30]. FSH concentration has been shown to be inversely proportional to the spermatogonial population and is associated with NOA [31]. It is, therefore, not surprising that patients in this study with either small testes or elevated FSH had a significantly worse outcome than those with normal parameters.
SRR was poorer in small testes group and elevated FSH, although not formally recommended; we could suggest that this group may benefit to underwent mTESE instead of conventional biopsy. The hormonal relationship with spermatogenesis is certainly not straightforward, with neither FSH, nor inhibin, able to predict successful sperm retrieval [32]. This is manifest by the range of levels of FSH seen in our study, and in particular the successful retrieval in 1 patient with an FSH of over 30 IU/L. Conversely, men with both normal testicular volume and normal FSH and yet late stage maturation arrest may be clinically indistinguishable from those with rete testis obstruction, particularly as FSH is normal in almost a third of those with defective spermatogenesis [4]. We calculated the best FSH level to predict the TESE result. Based on the analysis of the distribution of FSH levels in TESE positive and negative cases, and defining ROC curve we achieved 11, 0 UI/L as the best cut off value. A binary logistic regression was then taken considering the categorized FSH variable (greater or less than 11, 0 UI/L) and was statistically significant (p <.001). The model explained 45% (Nagelkerke R2) of the variance, correctly classifying 80.4% of the cases. An FSH value < 11, 0 UI/L was associated with an OR 19-fold higher for TESE+ result (95% CI 4.1-87.6). In practice and according to this model, an FSH value <11, 0 UI/L has a probability of TESE+ of 85% and if FSH> 11, 0 UI/L the probability of a TESE+ will be 24%. Further prospective studies with larger samples are needed to confirm this finding. Detection of Y chromosome micro-deletion occurred in 1, 9% of the cases and klinefelter karyotype in 11, 1% of patients. In the literature micro-deletion rates change between 8 and 18 percent [29]. It is known that the best TESE outcomes have been obtained in the AZFc group [33]. In compliance with this information, also in our study, in the only case with this deletion spermatozoa could be retrieved using TESE. As previously described in the literature patients with nonmosaic Klinefelter syndrome have sperm recovery and pregnancy rates comparable with patients having non-obstructive azoospermia and normal karyotype [34]. In our study only 16, 7% of patients with Klinefelter syndrome had sperm retrieved compared to 50% in the normal karyotype group. There was no statistical significance because the number of patients enrolled was small. We observed a clinical pregnancy and live birth rates of 26% in the best prognostic group (normal FSH and normal testis) in accordance with the previously published [35,36]. Unfortunately we weren’t able to achieve any live birth in the other prognostic groups, probably due to the restricted number of patients enrolled. Although the retrospective design and the restricted number of patients involved in the study we consider it as a useful example for all the urologists involved in the treatment of azoospermic patients. The possibility to advise patients about the positive sperm retrieval based on the FSH level (greater or less than 11, 0 UI/L) is an important clinical tool presented in this study. As goals to future studies in our center we plan to confirm these findings with an increased sample, have a detailed volumetric evaluation of testis, as well as inhibin B measurement in all patients.
Conclusion
In this study we achieved a SRR with multiple c-TESE of 51, 9% supporting this low-cost technique associated with ICSI as the first line treatment of NOA patients. These patients should always be fully assessed, and informed about the probability of positive TESE. FSH levels alone might be predictive as presented in this study. Furthermore those with normal FSH and normal testicular size can expect higher rates of sperm retrieval and live birth after ICSI.
References
- Lamb DJ (1999) World Health Organization. WHO Laboratory Manual for the Examination of Human Semen and Sperm-cervical Mucus Interaction. (4th edtn), Cambridge University Press, Cambridge, United Kingdom.
- Jarow JP, Espeland MA, Lipshultz LI (1989) Evaluation of the azoospermic patients. J Urol 142: 62-65.
- Matsumiya K, Namiki M, Takahara S, Kondoh N, Takada S, et al. (1994) Clinical study of azoospermia. Int J Androl 17: 140-142.
- Schlegel PN, Su LM (1997) Physiological consequences of testicular sperm extraction. Hum Reprod 12:1688-1692.
- Su LM, Palermo GD, Goldstein M, Veeck LL, Rosenwaks Z, et al. (1999) Testicular sperm extraction with intracytoplasmic sperm injection for nonobstructive azoospermia: testicular histology can predict success of sperm retrieval. J Urol 161: 112-116.
- Ezeh UI (2000) Beyond the clinical classification of azoospermia: opinion. Hum Reprod 15: 2356-2359.
- Donoso P, Tournaye H , Devroey P (2007) Which is the best sperm retrieval technique for non-obstructive azoospermia? A systematic review. Hum Reprod Update 13: 539-549.
- Tournaye H, Verheyen G, Nagy P, Ubaldi F, Goossens A, et al. (1997) Are there any predictive factors for successful testicular sperm recovery in azoospermic patients? Hum Reprod. 12: 80-86.
- Deruyver Y, Vanderschueren D, Van der Aa F (2014) Outcome of microdissection TESE compared with conventional TESE in non-obstructive azoospermia: a systematic review. Andrology 2: 20-24.
- Bernie AM, Mata DA, Ramasamy R, Schlegel PN (2015) Comparison of microdissection testicular sperm extraction, conventional testicular sperm extraction, and testicular sperm aspiration for nonobstructive azoospermia: a systematic review and meta-analysis. Fertil Steril. 104: 1099-1103.
- Chen SC, Hsieh JT, Yu HJ, Chang HC (2010) Appropriate cut-off value for follicle-stimulating hormone in azoospermia to predict spermatogenesis. Reprod Biol Endocrinol 8:108.
- Toulis KA, Iliadou PK, Venetis CA, Tsametis C, Tarlatzis BC, et al. (2010) Inhibin B and anti-Mullerian hormone as markers of persistent spermatogenesis in men with non-obstructive azoospermia: a meta-analysis of diagnostic accuracy studies. Hum Reprod Update 16: 713-724.
- Bryson CF, Ramasamy R, Sheehan M, Palermo GD, Rosenwaks Z, et al. (2014) Severe testicular atrophy does not affect the success of microdissection testicular sperm extraction. J Urol 191: 175-178.
- Yildirim ME, Koc A, Kaygusuz IC, Badem H, Karatas OF, et al. (2014) The association between serum follicle-stimulating hormone levels and the success of microdissection testicular sperm extraction in patients with azoospermia. Urol J 11: 1825-1828.
- Yang Q, Huang YP, Wang HX, Hu K, Wang YX, et al. (2015) Follicle-stimulating hormone as a predictor for sperm retrieval rate in patients with nonobstructive azoospermia: a systematic review and meta-analysis. Asian J Androl 17: 281-284.
- Samli MM, Dogan I (2004) An artificial neural network for predicting the presence of spermatozoa in the testes of men with nonobstructive azoospermia. J Urol 171: 2354-2357.
- Tsujimura A, Matsumiya K, Miyagawa Y, Takao T, Fujita K, et al. (2004) Prediction of successful outcome of microdissection testicular sperm extraction in men with idiopathic nonobstructive azoospermia. J Urol 172: 1944-1947.
- Boitrelle F, Robin G, Marcelli F, Albert M, Leroy-Martin B, et al. (2011) A predictive score for testicular sperm extraction quality and surgical ICSI outcome in non-obstructive azoospermia: a retrospective study. Hum Reprod 26: 3215-3221.
- Ramasamy R, Padilla WO, Osterberg EC, Srivastava A, Reifsnyder JE, et al. (2013) A comparison of models for predicting sperm retrieval before microdissection testicular sperm extraction in men with nonobstructive azoospermia. J Urol 189: 638-642.
- Silber SJ (2000) Microsurgical TESE and the distribution of spermatogenesis in non-obstructive azoospermia. Hum Reprod 15: 2278-2284.
- Hessel M, Ramos L, Hulsbergen AF, D’Hauwers KW, Braat DD, et al (2013) A novel cell-processing method ‘AgarCytos’ in conjunction with OCT3/4 and PLAP to detect intratubular germ cell neoplasia in non-obstructive azoospermia using remnants of testicular sperm extraction specimens. Hum Reprod 28: 2608-2620.
- Silber SJ, Nagy Z, Devroey P, Camus M, Van Steirteghem AC (1997) The effect of female age and ovarian reserve on pregnancy rate in male infertility: treatment of azoospermia with sperm retrieval and intracytoplasmic sperm injection. Hum Reprod 12: 2693-2700.
- Schlegel PN (1999) Testicular sperm extraction: microdissection improves sperm yield with minimal tissue excision. Hum Reprod 1999: 131-135.
- Turunc T, Gul U, Haydardedeoglu B, Bal N, Kuzgunbay B, et al. (2010) Conventional testicular sperm extraction combined with the microdissection technique in nonobstructive azoospermic patients: a prospective comparative study. Fertil Steril 94: 2157-2160.
- Saccà A, Pastore AL, Roscigno M, Naspro R, Pellucchi F, et al. (2016) Conventional testicular sperm extraction (TESE) and non-obstructive azoospermia: is there still a chance in the era of microdissection TESE? Results from a single non-academic community hospital. Andrology 4: 425-429.
- Adamopoulos DA, Koukkou EG (2009) Value of FSH and inhibin-B measurements in the diagnosis of azoospermia’-a clinician’s overview. Int J Androl 33: e109-e113.
- Çagri G, Turgut A, Lütfi T (2016) Effects of clinical, laboratuary and pathological features on successful sperm retrieval in non-obstructive azoospermia Turk J Urol 42: 168-177.
- Bohring C, Krause W (1999) Serum levels of inhibin B in men with different causes of spermatogenic failure. Andrologia 31: 137-141.
- Verheyen G, Popovic BT, Tournaye H (2017) Processing and selection of surgically-retrieved sperm for ICSI: a review Basic Clin Androl 27: 6.
- Boitrelle F, Robin G, Marcelli F, Albert M, Leroy-Martin B, et al. (2011) A predictive score for testicular sperm extraction quality and surgical ICSI outcome in non-obstructive azoospermia: a retrospective study. Hum Reprod 26: 3215-3221.
- Cissen M, Meijerink AM, D'Hauwers KW, Meissner A, van der Weide N, et al. (2016) Prediction model for obtaining spermatozoa with testicular sperm extraction in men with non-obstructive azoospermia. Hum Reprod 31: 1934-1941.
- Van Peperstraten AM, Proctor M, Johnson N, Philipson G (2008) Techniques for surgical retrieval of sperm prior to intra-cytoplasmic sperm injection (ICSI) for azoospermia Cochrane Database Syst Rev 16.
- Edwards RG, Tarin JJ, Dean N, Hirsch A, Tan SL (1994) Are spermatid injections into human oocytes now mandatory? Hum Reprod 9: 2217-2219.
- Yarali H, Polat M, Bozdag G, Gunel M, Alpas I, et al. (2009) B TESE-ICSI in patients with non-mosaic Klinefelter syndrome: a comparative study. Reprod Biomed Online 18:756-760.
- Kahraman S, Ozg€ur S, Alatas C, Aksoy S, Balaban B, et al. (1996) High implantation and pregnancy rates with testicular sperm extraction and intracytoplasmic sperm injection in obstructive and non-obstructive azoospermia. Hum Reprod 11: 673-676.
- Bromage SJ, Falconer DA, Lieberman BA, Sangar V, Payne SR (2007) Sperm retrieval rates in subgroups of primary azoospermic males. Eur Urol 51: 534-540.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi