Case Report, Int J Cardiovasc Res Vol: 8 Issue: 4
Hybrid Myocardial Revascularization or Multivessel Minimally Invasive Direct Coronary Artery Bypass: Two Case Reports
Van den Eynde J1, Johan Bennett2, Keir McCutcheon2, Tom Adriaenssens2, Tom Verbelen1, Steven Jacobs1 and Wouter Oosterlinck1*
1Department of Cardiovascular Diseases, Research Unit of Cardiac Surgery, University Hospitals Leuven, Belgium
2Department of Cardiovascular Medicine, University Hospitals Leuven, Belgium
*Corresponding Author: Prof. W Oosterlinck, MD, PhD.
Department of Cardiovascular Diseases, University Hospitals Leuven, KU Leuven, Herestraat 49, 3000 Leuven, Belgium
Tel: +32 16 344260
Fax: +32 16 344616
E-mail: wouter.oosterlinck@uzleuven.be
Received: July 18, 2019 Accepted: July 31, 2019 Published: August 07, 2019
Citation: Van den Eynde J, Bennett J, McCutcheon K, Adriaenssens T, Verbelen T, et al. (2019) Hybrid Myocardial Revascularization or Multivessel Minimally Invasive Direct Coronary Artery Bypass: Two Case Reports. Int J Cardiovasc Res 8:4.
Abstract
Since the first introduction of direct grafting of the Left Anterior Descending artery (LAD) by Kolessov in 1967, the tendency in myocardial revascularization has been towards less invasive techniques. New developments are increasingly making it possible to extend the indication for Robotically Assisted Minimally Invasive Direct Coronary Artery Bypass (RAMIDCAB) surgery to patients with triple vessel disease. Here, we present two cases in which complete revascularization was successfully achieved. The first patient underwent a hybrid procedure involving RA-MIDCAB followed by Percutaneous Coronary Intervention (PCI); the other patient received RA-MIDCAB in which bilateral internal mammary arteries were used as a conduit for grafting. The implications, limitations and challenges of these interventional strategies are discussed. Furthermore, it is suggested that minimally invasive strategies might have important benefits especially for high-risk patients, and that these strategies should be included in decisionmaking by the Heart Team if available.
Keywords: Coronary artery bypass grafting; Hybrid revascularization; Minimally invasive direct coronary artery bypass grafting; Minimally invasive surgery; Myocardial revascularization; Percutaneous coronary intervention
Background
Since the first introduction of direct grafting of the Left Anterior Descending artery (LAD) by Kolessov, [1] the tendency in myocardial revascularization has been towards less invasive techniques. Robotically Assisted Minimally Invasive Direct Coronary Artery Bypass (RA-MIDCAB) surgery is a technique that permits revascularization without the need for cardiopulmonary bypass and median sternotomy. The anastomosis is performed through a left anterior small thoracotomy and the internal mammary artery is harvested using the da Vinci® Surgical System (Intuitive Surgical, Sunnyvale, CA, USA). MIDCAB has shown to have a similar safety and efficacy profile to conventional on-pump and off-pump Coronary Artery Bypass Grafting (CABG), with the additional advantages of reduced need for blood transfusion, early intubation, and shorter hospital stay [2,3].
Initially, the application of MIDCAB has been limited to the LAD and its diagonal branches, for which it is the preferred revascularization strategy [4,5]. However, new possibilities have become available to extend its use and to consider MIDCAB as a strategy in patients with extensive triple vessel disease. First, in hybrid MIDCAB-PCI, grafting of the LAD and/or its diagonal branches is combined with Percutaneous Coronary Intervention (PCI) of non-LAD vessels, either during one visit to a hybrid operating theatre or in a staged fashion including two procedures in different locations and time points. Secondly, MIDCAB using Bilateral Internal Mammary Artery (BIMA) grafts allows grafting of additional coronary arteries, such as the Left Circumflex Artery (LCX). Here, we present two cases that illustrate the applicability of both strategies in patients with triple vessel disease.
Case 1
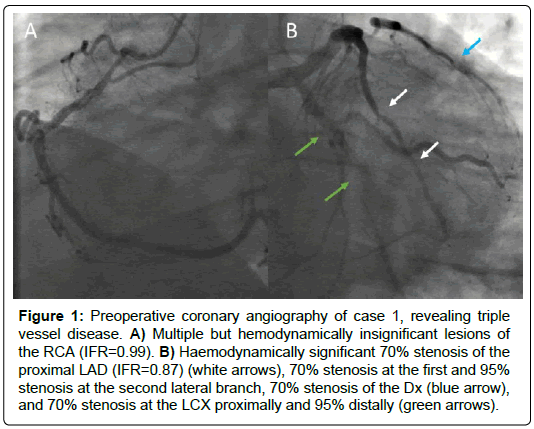
A 39-year old man was admitted to our tertiary-care centre with new onset angina pectoris. The patient had a Body Mass Index (BMI) of 33 kg/m2, a history of smoking (17 pack-years), and was known with hypercholesterolemia for which he was treated with 20 mg simvastatin daily. After the onset of symptoms, 80 mg aspirin and 1.25 mg bisoprolol daily were started. Resting electrocardiogram was normal. Transthoracic echocardiography showed normal left ventricular systolic function and a stress cardiac Magnetic Resonance Imaging (MRI) revealed inducible ischemia in the inferior and inferolateral walls. Coronary angiography revealed triple vessel disease with a haemodynamically significant 70% stenosis of the proximal LAD (instantaneous wave-free ratio, iFR=0.87), a 70% stenosis of the first diagonal branch (Dx), a 70% stenosis in the LCX proximally and 95% distally, a 70% stenosis in the first Obtuse Marginal (OM) and a 95% stenosis in the second OM, and multiple but hemodynamically insignificant lesions of the Right Coronary Artery (RCA) (iFR=0.99) (Figure 1).
Figure 1: Preoperative coronary angiography of case 1, revealing triple vessel disease. A) Multiple but hemodynamically insignificant lesions of the RCA (IFR=0.99). B) Haemodynamically significant 70% stenosis of the proximal LAD (IFR=0.87) (white arrows), 70% stenosis at the first and 95% stenosis at the second lateral branch, 70% stenosis of the Dx (blue arrow), and 70% stenosis at the LCX proximally and 95% distally (green arrows).
During Heart Team discussion, MIDCAB BIMA or a hybrid MIDCAB-PCI approach were both considered to be appropriate. In consultation with the patient, the decision was made to schedule elective hybrid revascularisation involving RA-MIDCAB for the construction of LIMA-Dx-LAD, and a PCI of the LCX during a second admission four weeks later.
Following the surgery, the patient was monitored for one day in the Intensive Care Unit (ICU), after which he was transferred to the general ward. Here, the patient developed a left lower lobe pneumonia which was successfully treated with antibiotics, permitting discharge 12 days after surgery.
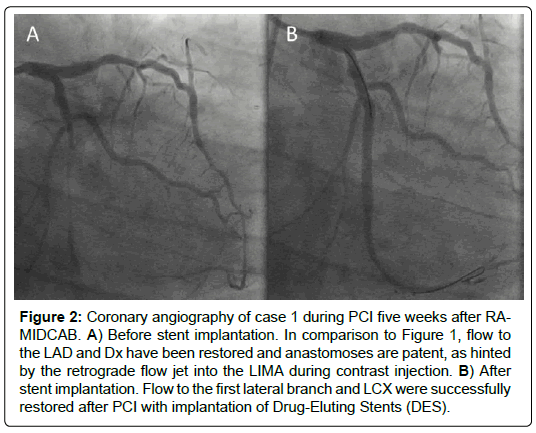
Five weeks after surgery, PCI was successfully performed with the implantation of two Drug-Eluting Stents (DES), one in the first lateral branch and one in the distal LCX (Figure 2). Clopidogrel was initiated at a dose of 75 mg daily for 12 months.
Figure 2: Coronary angiography of case 1 during PCI five weeks after RAMIDCAB. A) Before stent implantation. In comparison to Figure 1, flow to the LAD and Dx have been restored and anastomoses are patent, as hinted by the retrograde flow jet into the LIMA during contrast injection. B) After stent implantation. Flow to the first lateral branch and LCX were successfully restored after PCI with implantation of Drug-Eluting Stents (DES).
Five months after the surgery, the patient was doing well and had no complaints of ischemia or exercise intolerance. Aerobic performance had increased to 110% of the mean sedentary values for age and gender, compared to 78% at the start cardiac of rehabilitation.
Case 2
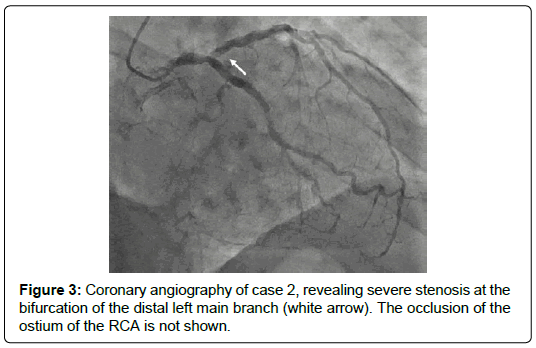
The second patient was a 70-year old man with a history of arterial hypertension, obesity and hyperlipidemia. One month before admission to our hospital, he had received a bilateral Percutaneous Trans-luminal Angioplasty (PTA) for revascularization of the distal femoral arteries, after which 80 mg aspirin and 75 mg clopidogrel daily had been initiated. He was admitted because of symptomatic angina. Electrocardiography showed ST elevation in V2 and V3, and T inversion on V6, I and aVL, as well as a positive cyclo-ergometry. Echocardiography revealed near-normal LV function with mild dilatation and hypertrophy, as well as mild diastolic dysfunction. Coronary angiography revealed severe stenosis at the bifurcation of the distal left main coronary artery and occlusion of the ostium of the RCA but with complete collateral supply (Figure 3). Carotid artery Doppler ultrasound showed moderate (<70%) stenosis of the right carotid artery and severe (>70%) stenosis of the left carotid artery.
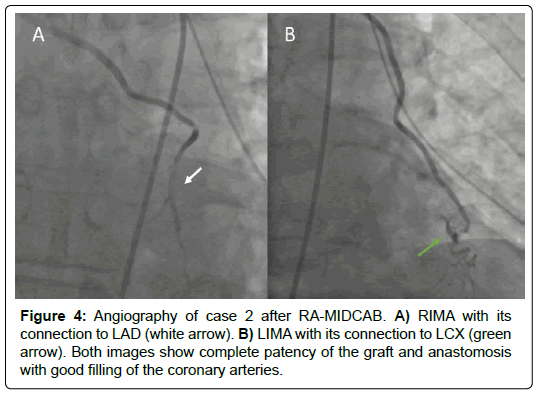
The patient was scheduled for RA-MIDCAB involving construction of RIMA-LAD and LIMA-LCX. On the ICU was uncomplicated, with only mild increases in the J-shaped STelevations in V2 and V3 on electrocardiography, suggestive for pericarditis. Postoperative angiography was performed to further investigate this, and confirmed patency of the grafts and anastomoses with good filling of the coronaries to their distal ends (Figure 4). One day after surgery, the patient was transferred to the ward. The patient was discharged 7 days after surgery.
Discussion
We described two cases of triple vessel disease in which RAMIDCAB was performed as a revascularization strategy, either combined with PCI of non-LAD vessels in a hybrid approach, or by using both mammary arteries as a conduit for grafting. The first patient was a young man who received RA-MIDCAB for the construction of LIMA-Dx-LAD and a PCI of the LCX. The second patient, an elderly man with pronounced peripheral artery disease, underwent RA-MIDCAB involving construction of RIMA-LAD and LIMA-LCX. In both cases, successful revascularization was achieved. This suggests that MIDCAB, either alone or in combination with PCI, can be considered in patients with triple vessel disease.
In hybrid procedures, the best of both worlds are combined: both the excellent patency rates for the LAD after MIDCAB, and the early recovery and reduced morbidity after PCI for non-LAD lesions. The hybrid strategy, with PCI of non-LAD lesions, also means that the right internal mammary artery is still available for possible futures redo MIDCAB in the case of graft failure or restenosis. This might be an important consideration in younger patients, such as our first case, where the need for repeat revascularization is plausible.
Several aspects of hybrid revascularization remain to be further elucidated, such as the ideal timing between surgery and PCI, as well as the order in which the procedures should be performed [6]. Often, the order is determined based on the culprit lesion, which is treated first. However, if PCI is to be performed first or at the same time of surgery, it is currently unknown what effect dual antiplatelet therapy has on the course of surgery itself or complications after surgery [7]. On the other hand, performing PCI after surgery introduces the opportunity to check for graft patency on coronary angiography; in the event of graft defects, these can either be addressed immediately via PCI, or scheduled for revision surgery.
The extension of MIDCAB to vessels other than the LAD and its diagonal branches has in the past been hampered by two major challenges. First, in contrast to open surgery, manipulation of the heart through a thoracotomy is far more challenging. This has put an anatomical limitation to the extent of target vessels that can be reached, especially on the lateral and posterior sides of the heart. However, stabilization devices have now become widely available that allow better exposure of the LAD, as well as other vessels. Secondly, the limited accessibility of the aorta during MIDCAB makes it difficult to perform proximal anastomoses for additional grafts. However, BIMA grafts combined with radial Y-grafts have been reported as an alternative to achieve revascularization with multiple grafts [8,9].
The usual candidate population for myocardial revascularization is increasingly presenting with anatomically complex coronary artery disease, as well as multiple comorbidities and frailty [10]. Interventional procedures are therefore bound to become both more effective and less invasive. The development of PCI and MIDCAB in recent years should be seen from this perspective, as they reduce procedure-related risk, which might be especially beneficial for highrisk populations such as those suffering from chronic obstructive pulmonary disease, severe liver disease, or carotid artery disease. Among others, hybrid approaches are associated with shorter hospital stay, reduced disturbance of homeostasis, and faster recovery. Currently, these procedures are only offered to carefully selected patients. However, continuous effort should be spent to further develop these procedures, making them available for a large population of patients.
Conclusion
Hybrid approaches combining MIDCAB and PCI, and MIDCAB with BIMA grafts can both be used as a revascularization strategy in patients with triple vessel disease. If available in the hospital, these strategies should be included in decision-making by the Heart Team.
Acknowledgement
None.
Conflict of Interest
No Conflict of Interest.
References
- Kolessov VI (1967) Mammary artery-coronary artery anastomosis as method of treatment for angina pectoris. J Thorac Cardiovasc Surg 54: 535-544.
- Groh MA, Sutherland SE, Burton HGIII, Johnson AM, Ely SW (1999) Port-access coronary artery bypass grafting: Technique and comparative results. Ann Thorac Surg 68: 1506-1508.
- Lapierre H, Chan V, Sohmer B, Mesana TG, Ruel M (2011) Minimal invasive coronary artery bypass grafting via a small thoracotomy versus off-pump: A case-matched study. Eur J Cardiothorac Surg 40: 804-810.
- Neumann FJ, Sousa-Uva M, Ahlsson A, Alfonso F, Banning AP, et al. (2019) 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J 40: 87-165.
- Wang XW, Qu C, Huang C, Xiang XY, Lu ZQ (2016) Minimally invasive direct coronary bypass compared with percutaneous coronary intervention for left anterior descending artery disease: A meta-analysis. J Cardiothorac Surg 11: 125.
- Green KD, Lynch DR Jr, Chen TP, Zhao D (2013) Combining PCI and CABG: the role of hybrid revascularization. Curr Cardiol Rep 15: 351.
- Gao P, Xiong H, Zheng Z, Li L, Gao R, et al. (2010) Evaluation of antiplatelet effects of a modified protocol by platelet aggregation in patients undergoing "one-stop" hybrid coronary revascularization. Platelets 21: 183-190.
- Calafiore AM, Contini M, Vitolla G, Di Mauro M, Mazzei V, et al. (2000) Bilateral internal thoracic artery grafting: long-term clinical and angiographic results of in situ vs. Y grafts. J Thorac Cardiovasc Surg 120: 990-996.
- Weerasinghe A, Bahrami T (2005) Bilateral MIDCAB for triple vessel coronary disease. Interact Cardiovasc Thorac Surg 4: 523-525
- Kirtane AJ, Doshi D, Leon MB, Lasala JM, Ohman EM, et al. (2016) Treatment of higher-risk patients with an indication for revascularization: Evolution within the field of contemporary percutaneous coronary intervention. Circulation 134: 422-431.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi