Case Report, Vol: 13 Issue: 1
Impact of Environmental Toxins on Female Fertility: A Critical Review
Kovac TR*
Department of Biotechnology, Bharathiar University, Colombia
- *Corresponding Author:
- Kovac TR
Department of Biotechnology, Bharathiar University, Colombia
E-mail: Kovac123@yahoo.com
Received: 07-March-2025, Manuscript No. AGCR-25-168377, Editor assigned: 08-March-2025, PreQC No. AGCR-25-168377 (PQ), Reviewed: 15-March-2025, QC No. AGCR-25-168377, Revised: 22-March-2025, Manuscript No. AGCR-25-168377 (R), Published: 28-March-2025, DOI:10.4172/2325-9620.1000349
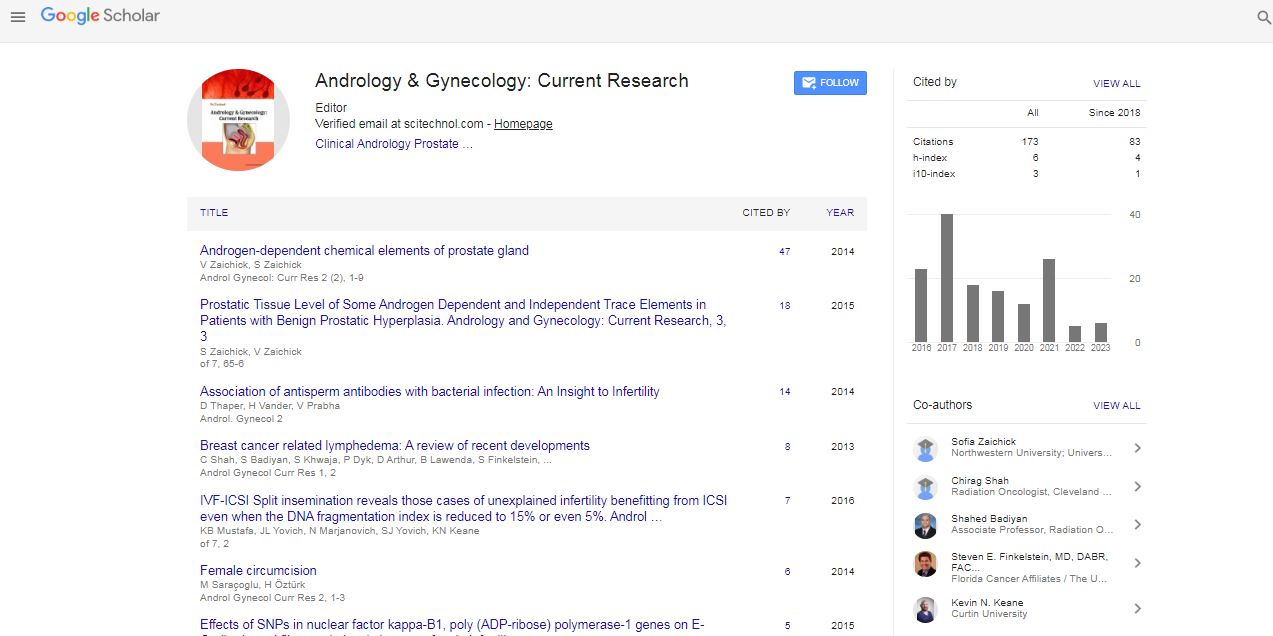
Citation: Kovac TR (2025) Impact of Environmental Toxins on Female Fertility: A Critical Review. Androl Gynecol: Curr Res 13:1.
Copyright: © 2025 Kovac TR. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited
Abstract
Introduction
Female fertility is influenced by a complex interplay of genetic, hormonal, lifestyle, and environmental factors. In recent decades, there has been growing concern about the impact of environmental toxins on reproductive health. Exposure to endocrine-disrupting chemicals (EDCs), heavy metals, pesticides, and air pollutants is increasingly recognized as a significant threat to female fertility worldwide. This editorial critically reviews current evidence linking environmental toxins with adverse effects on female reproductive function, emphasizing the need for further research and public health interventions [1]-5].
Environmental Toxins and Their Sources
Environmental toxins implicated in fertility disruption include:
- Endocrine-disrupting chemicals (EDCs): Bisphenol A (BPA), phthalates, polychlorinated biphenyls (PCBs), and dioxins commonly found in plastics, personal care products, and industrial waste.
- Heavy metals: Lead, cadmium, and mercury exposure occur through contaminated water, food, and air.
- Pesticides: Organophosphates, organochlorines, and herbicides used in agriculture can contaminate food and water.
- Air pollutants: Particulate matter, polycyclic aromatic hydrocarbons (PAHs), and other airborne toxins are linked to urban and industrial pollution.
Mechanisms of Toxicity Affecting Female Fertility
Environmental toxins affect female fertility through several mechanisms:
- Hormonal Disruption
Many EDCs mimic or block natural hormones, particularly estrogens and androgens, altering the hypothalamic-pituitary-ovarian axis and ovarian function. This disruption can lead to irregular menstrual cycles, anovulation, and impaired folliculogenesis.
- Ovarian Reserve Depletion
Exposure to certain toxins is associated with accelerated follicular atresia and decreased ovarian reserve, measurable by reduced anti-Müllerian hormone (AMH) levels and antral follicle counts.
- DNA Damage and Oxidative Stress
Toxins induce oxidative stress and DNA damage in oocytes and granulosa cells, potentially compromising oocyte quality and embryo development.
- Endometrial Receptivity Impairment
Some chemicals interfere with endometrial cell function, reducing implantation success and increasing miscarriage risk.
Evidence from Epidemiological and Experimental Studies
Multiple epidemiological studies have linked higher exposure to BPA, phthalates, and pesticides with reduced fertility rates, longer time to pregnancy, and higher miscarriage incidence. Animal models demonstrate dose-dependent ovarian toxicity and altered reproductive hormone profiles after toxin exposure.
However, inconsistencies exist due to variations in exposure assessment, population heterogeneity, and confounding factors. More longitudinal and mechanistic studies are needed.
Public Health and Clinical Implications
Recognition of environmental toxins as modifiable risk factors for female infertility highlights the importance of preventive strategies:
- Regulatory policies to limit or ban harmful substances
- Public education on reducing exposure (e.g., avoiding plastic containers with BPA, using organic produce)
- Screening and counseling women with infertility for environmental risk factors
- Incorporation of environmental exposure assessment into fertility workups
Conclusion
Environmental toxins pose a significant and often underappreciated risk to female reproductive health. Current evidence underscores the need for heightened awareness, stricter environmental regulations, and focused research to clarify mechanisms and guide effective interventions. Protecting reproductive potential requires a multidisciplinary approach involving clinicians, researchers, policymakers, and the public.
References
- Mujagic S, Kozic D, Huseinagic H, Smajlovic D. Symmetry, asymmetry and hypoplasia of intracranial internal carotid artery on magnetic resonance angiography. Acta Med Acad. 2016; 45:1- 9.
- Rusu MC, Vrapclu AD, Lazar M. A rare variant of accessory cerebral artery. Surg Radiol Anat. 2023; 45(5):523-526.
- Krause DA, Youdas JW. Bilateral presence of a variant subscapularis muscle. Int J Anat Var. 2017; 10(4):79-80.
- Mann MR, Plutecki D, Janda P, PÄ?kala J, Malinowski K, et al. The subscapularis muscleâ?a metaâ?analysis of its variations, prevalence, and anatomy.â?¯ Clin Anat. 2023; 36(3):527-541.
- Pillay M, Jacob SM. Bilateral presence of axillary arch muscle passing through the posterior cord of the brachial plexus. Int. J. Morphol., 27(4):1047-1050, 2009.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi