Research Article, Int J Cardiovasc Res Vol: 8 Issue: 4
Pattern of Lipid Profile in Pregnancy and its Impact on the Gestational Course
Ashraf Reda1, Awni Gamal1, Mohamed Rezk2 and Gehad Gamal3*
1Department of Cardiology, Faculty of Medicine, Menoufia University, Menoufia Governorate, Egypt
2Department of Obstetrics and Gynecology, Faculty of Medicine, Menoufia University, Menoufia Governorate, Egypt
3Department of Cardiology, Dar AlFouad Hospital, Giza, Egypt
*Corresponding Author: Gehad Gamal
Department of Cardiology, Dar AlFouad Hospital, Giza, Egypt
E-mail: gehadgamal83@gmail.com
Received: November 02, 2018 Accepted: February 13, 2019 Published: February 20, 2019
Citation: Reda A, Gamal A, Rezk M, Gamal G (2019) Pattern of Lipid Profile in Pregnancy and its Impact on the Gestational Course. Int J Cardiovasc Res 8:4.
Abstract
Background: Major changes in lipid profile occur during normal pregnancy with significant correlation could be detected with gestational complications.
Objective: We aimed to screen lipid profile in a sample of Egyptian pregnant and assess the correlation between second trimester maternal lipid profile and gestational outcome.
Methods: This cohort study included 94 women with maternal lipid profile assessed during the second trimester (16-18 weeks). Serial antenatal visits were conducted to record the development of maternal gestational hypertension, preeclampsia, gestational diabetes mellitus and low birth weight.
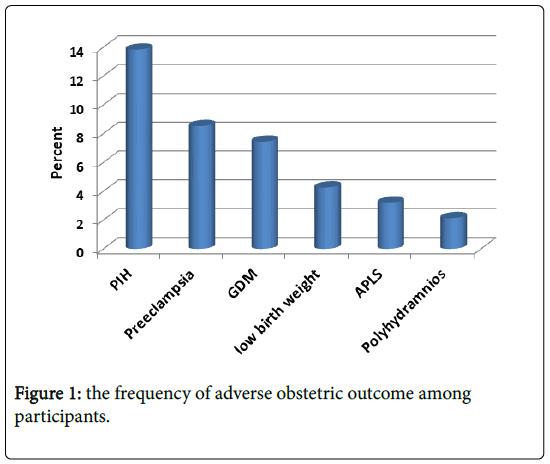
Results and discussion: Lipid profile components in pregnant is higher than normal references. Meanwhile, gestational hypertension (GH) was the most common complication in the study affecting 13 patients (13.8%) followed by preeclampsia (PE) in 8 patients (8.5%), gestational DM (GDM) in 7 patients (7.4%) and lastly low birth weight in 4 neonates (4.3%). Positive association between second trimester lipid profile components and GH, PE and GDM was found.
Conclusion: Measurement of lipid profile during the second trimester is highly recommended and could be a useful predictor of hypertensive disorders and GDM among Egyptian women.
Keywords: Lipid profile; Preeclampsia; Hypertensive disorders during pregnancy; Gestational diabetes mellitus
Introduction
Major changes in lipid profile occur during normal pregnancy with progressive increase in maternal plasma cholesterol and triglyceride levels during the late second and the third trimester, returning to normal after delivery [1-4].
Pregnancy-associated hyperlipidemia was linked with maternal morbidity with development of gestational diabetes mellitus and preeclampsia [5-7]. To the authors’ knowledge, there were no studies in the literature addressing lipid profile in pregnant women in Egypt. We aimed to screen the lipid profile pattern in the pregnant then assess the correlation between second trimester maternal lipid profile and adverse pregnancy outcome among cohort of Egyptian pregnant women.
Patients and Methods
Patient populations
This prospective study was conducted at the department of Cardiology in collaboration with the Obstetrics and Gynecology department, Menoufia University hospital, Menoufia governorate, Egypt during the period between June 2016 and June 2018. The study protocol was formally reviewed and approved by the ethics committee for human research at Menoufia Faculty of Medicine with informed consent obtained from all participants prior to commencement of the study after thorough explanation of the study objectives.
Inclusion criteria
Pregnant women attending the antenatal care clinic at Menoufia University hospital during early first trimester at 6-12 weeks gestation were invited to participate. Gestational age was based on the date of last menstrual period together with early obstetric ultrasound scan.
Exclusion criteria
• Women with preexisting medical disorders as diabetes mellitus and hypertension
• History of congenital fetal malformations or interrupted pregnancy (whether spontaneous or induced abortion)
• Pregnant with drug intake affecting lipid profile.
Methods
After exclusion of non-responders, drop out participants and those with exclusion criteria, 94 women completed the study (this number was considered suitable enough sample for statistical analysis with significant results and correlations).
Blood samples was drawn from all the subjects following a fast of 12 hours at 16-18 weeks’ gestation and analyzed for Serum Triglycerides (TG), Total cholesterol (TC), LDL cholesterol and HDL cholesterol (HDL-C) by enzymatic methods auto analyzer. Participants were followed up at the antenatal care clinic throughout pregnancy with frequency of visits of 5 visits and delivered at Menoufia University hospital.
Outcome measures
Maternal outcome development of gestational hypertension (elevation of blood pressure ≥ 140/90 mmHg after 20 weeks’ gestation on two occasions with 4-hours apart after rest).The definition of hypertension in pregnancy is based only on office (or in-hospital) BP values [systolic BP (SBP) ≥ 140 mmHg and/or DBP ≥ 90 mmHg and distinguishes mildly (140-159/90-109 mmHg) or severely (≥ 160/110 mmHg) elevated BP.
Preeclampsia (a new-onset hypertension associated with new-onset proteinuria of ≥ 0.3 g protein in 24 h urine collection or urinary dipsticks ≥ 1+) or gestational diabetes mellitus (elevated ≥ 2 values after performing a 75 g, two-hour oral glucose tolerance test).Fetal and neonatal outcome: low birth weight, defined as a birth weight<2500 g. Then participants were followed up 6 weeks after delivery at the postnatal care clinic at Menoufia University hospital to confirm the normalization of lipid profile level. The whole study group was classified into four groups according to the complications: (Group 1: patients with gestational DM (GDM), group 2: patients with gestational HTN/pregnancy induced HTN, group 3: patients with preeclampsia (PE) and group 4: patients with (LBW)).
Results
Maternal demographic data including age, weight, height, BMI, baseline systolic, diastolic blood pressure and maternal lipid profile in relation to normal range was showed (Table 1).
| N | Minimum | Maximum | Mean | Std. Deviation | |
|---|---|---|---|---|---|
| Age | 94 | 22 | 43 | 30.14 | 4.760 |
| Wt | 94 | 50 | 115 | 79.46 | 11.053 |
| Ht | 94 | 150 | 179 | 164.19 | 6.306 |
| BMI | 94 | 21.3 | 40.3 | 29.531 | 4.1965 |
| SBP | 94 | 80 | 180 | 117.91 | 23.595 |
| DBP | 94 | 50 | 185 | 75.60 | 18.084 |
| Chol | 94 | 160 | 340 | 249.34 | 46.963 |
| HDL | 94 | 35 | 101 | 67.26 | 12.076 |
| LDL | 94 | 48 | 230 | 137.20 | 45.601 |
| TG | 94 | 94 | 491 | 220.39 | 83.771 |
| Chol% difference | 94 | -20 | 70 | 24.67 | 23.482 |
| HDL% difference | 94 | -30 | 102 | 34.51 | 24.152 |
| LDL% difference | 94 | -63 | 77 | 5.54 | 35.078 |
| TG% difference | 94 | -37 | 227 | 46.93 | 55.847 |
Table 1: Maternal demographic data.
Regarding mean value of lipid profile components in pregnancy: Cholesterol 249 mg/dl (reference normal value 200 mg/dl) HDL 67 md/dl (reference normal value>50 mg/dl), LDL 137 mg/dl (reference normal value 130 mg/dl) and TG 220 mg/dl (reference normal value 150 mg/dl). Meanwhile, mean percent difference from the reference normal values of the lipid profile were: Cholesterol% difference 24.5%, HDL% difference 34.5%, LDL% difference 5.5% and TG% difference 46.9%.
Frequency of adverse obstetric outcome among participants was showed as following: Gestational hypertension (pregnancy induced HTN=PIH) was the most common complication in the study affecting 13 patients (13.8%) followed by preeclampsia in 8 patients (8.5%), gestational DM (GDM) in 7 patients (7.4%) and lastly low birth weight in 4 neonates (4.3%) (Figure 1).
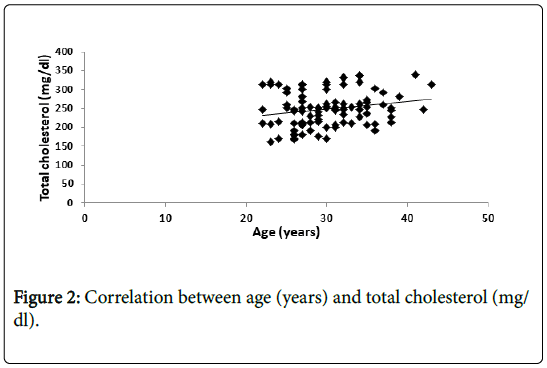
Meanwhile, there is positive significant correlation between total cholesterol (TC) level and age (Figure 2).
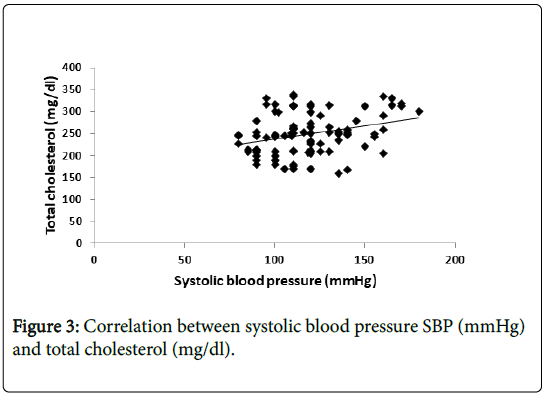
Also, there is positive significant correlation between total cholesterol (TC) level and systolic blood pressure (Figure 3).
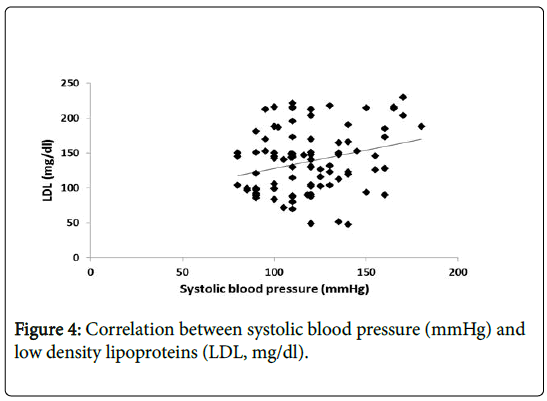
While, there is positive significant correlation between (LDL) level and (SBP) (Figure 4).
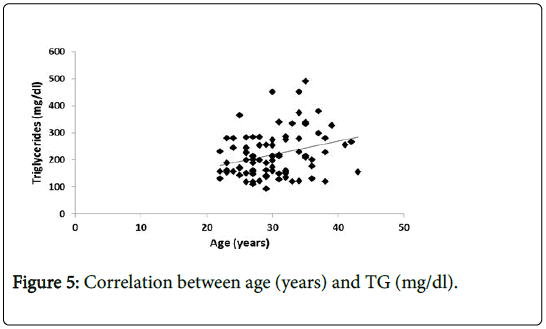
In addition, there is positive significant correlation between (TG) level and age (Figure 5).
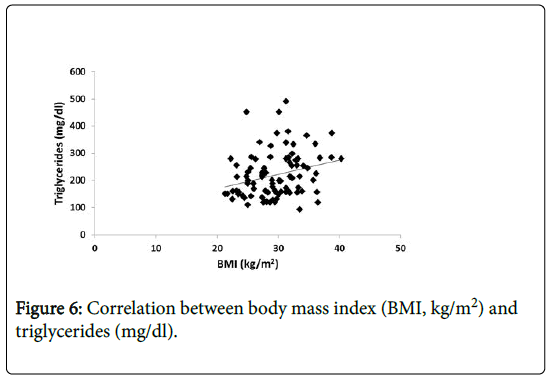
Also, there is positive significant correlation between (TG) and and BMI (Figure 6).
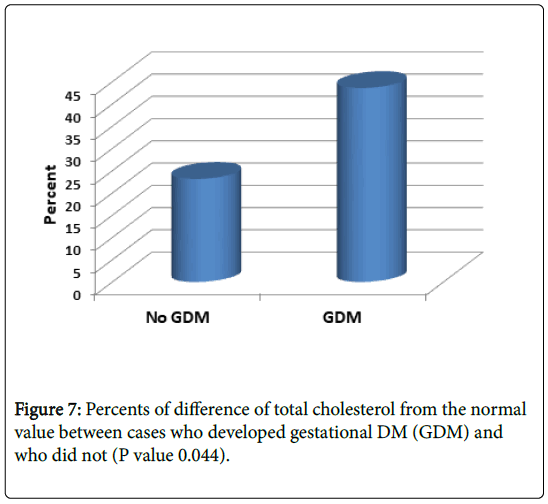
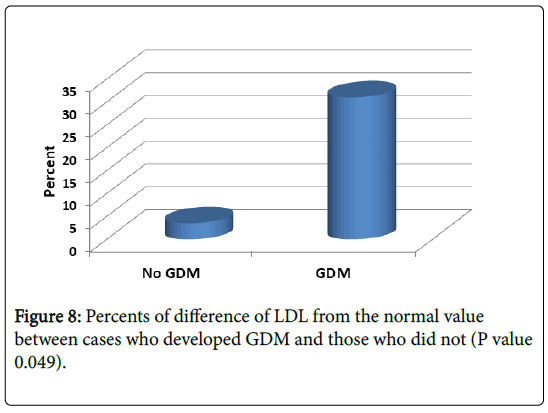
Mean percent difference from the reference normal values in patient developed gestational DM were significantly higher than those without GDM: Cholesterol 44% (vs. 23% in those without GDM) and LDL 31% (vs. 3% in those without GDM) (P value 0.044 and 0.049 respectively) (Figures 7 and 8).
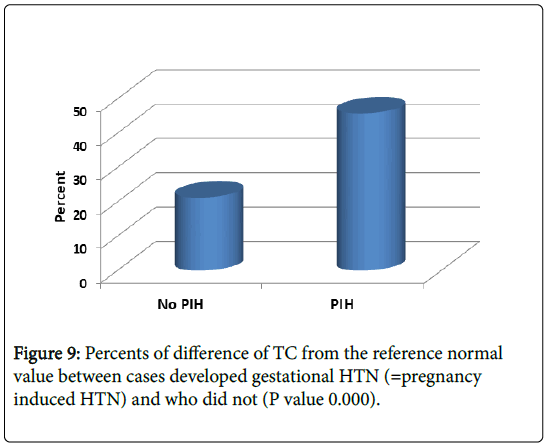
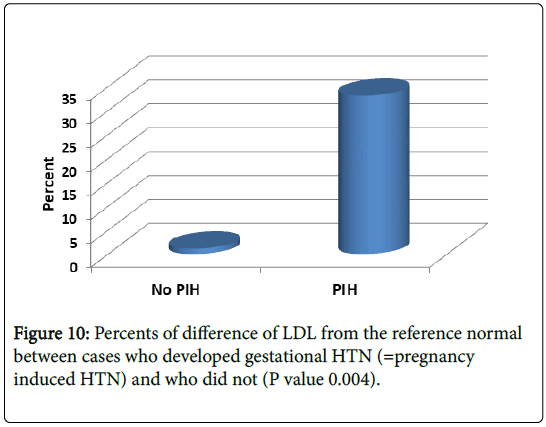
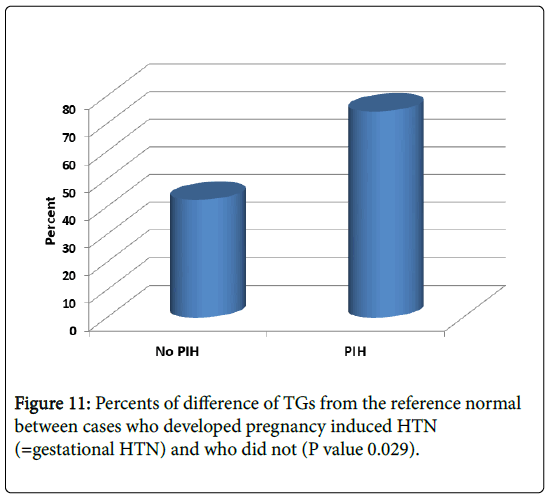
As shown in Figures 9-11, we showed mean percent difference of lipid profile in patient developed gestational HTN were significantly higher than those without gestational HTN: Cholesterol 46% (21% in those without HTN), LDL 33% (vs. 1.1%in those without HTN) and TG 74% (vs. 42% in those without HTN) (P value 0.0001, 0.004 and 0.029 respectively).
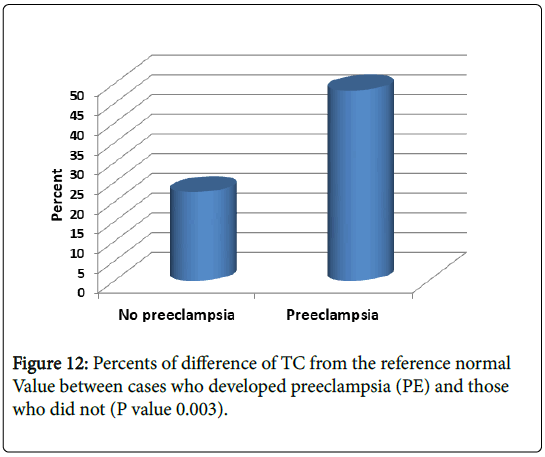
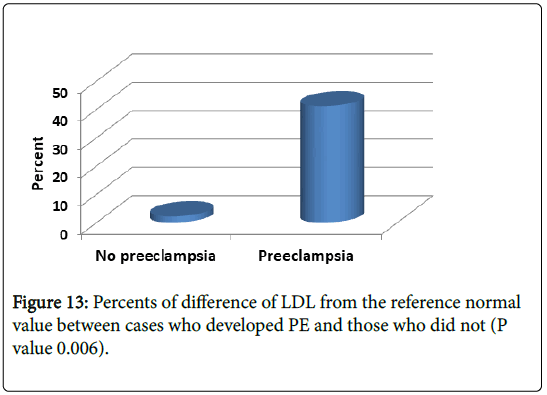
We speculated mean percent difference of lipid profile in patient developed preeclampsia (PE) were significantly higher than those without: Cholesterol 48% (vs. 23% in those without) and LDL 41% (vs. 2.2% in those without) P value 0.003 and 0.006 respectively (Figures 12 and 13).
Discussion
The current study confirmed the previous associations between altered maternal lipid profile components and adverse maternal outcome. Second trimester elevated TC and LDL were found in women developed GDM. TC, TG and LDL were elevated in those developing gestational hypertension while elevated TC, LDL and high BMI were associated with the development of preeclampsia.
Maternal plasma lipids climb substantially above levels seen in normal pregnancies in women who developed preeclampsia or IUGR without maternal systemic manifestations of hypertension and proteinuria [8]. A more recent population-based study from China including 934 pairs of non-diabetic mothers and neonates between 2010 and 2011 with maternal lipid profile measured during the first, second and third trimesters had revealed that maternal high TG in late pregnancy was independently associated with increased risk of GDM [9].
Even though, pre-pregnancy altered maternal lipid profile was associated with subsequent development of GDM as depicted in recent nested case control study [10]. Bharathi et al., tested lipid profile in 100 Indian pregnant showed serum triglyceride, total cholesterol and VLDL level are significantly higher among woman with GDM compared to non GDM pregnant women [11].
A previous larger cohort study included 4008 non-diabetic women with early maternal lipid profile measured during early gestation (12-14 weeks) to detect the association between lipid profile and pregnancy-induced hypertension (PIH), had revealed that every unit increase in TG was linearly associated with an increased risk of PIH [odds ratio (OR)=1.60, P=0.021] while TC was not associated with any of the outcome measures [12]. Our results were concordant to Chandi et al., who recognized an association of maternal hypertriglyceridemia with pregnancy-induced hypertension. Among 59 women, a significant positive correlation was found between serum TG concentration and systolic blood pressure. Also, the mothers with hypertriglyceridemia were found to be at higher risk of developing early-onset gestational HTN [13].
Anaelechi et al. have evaluated the serum lipid profile and Creactive protein (CRP) in 35 Nigerian women with pre-eclampsia and indicated that the women with pre-eclampsia had a significantly higher mean serum CRP (p=0.001), TG (p=0.001) and total cholesterol (p=0.001) level but a lower mean HDL-C (p=0.001) level than the controls [14].
The difference between our results and others can be explained on the basis of race, maternal age, nutrition, stage of pregnancy, socioeconomic, genetic factors and dietary pattern of individuals. From all these data, lifestyle modifications for women during the reproductive years should focus on lowering maternal triglyceride levels through diet, weight reduction and physical activity that may help in decreasing the maternal complications during pregnancy. Inability to measure maternal lipid profile during the three trimesters secondary to their high cost as well as to include larger cohort was unintended limitations of the current study. Future research should explore the implementation of maternal lipid profile and lifestyle modifications for the prevention of hypertensive disorders during pregnancy and other adverse outcome.
Conclusion
Maternal lipid profile components increase significantly in patients with hypertensive disorders and GDM among Egyptian women. Lifestyle modifications are required to prevent complications. Accordingly, we recommend Lipid profile should be done routinely during gestational course follow. Further studies with larger number of patients are required and, if possible, assessment of lipid profile pre pregnancy, during the three trimesters and after delivery (to compare all together).
References
- Lippi G, Albiero A, Montagnana M, Salvagno GL, Scevarolli S (2007) Lipid and lipoprotein profile in physiological pregnancy. Clin Lab 53: 173–177.
- Husain F, Latif S, Uddin M, Nessa A (2008) Lipid profile changes in second trimester of pregnancy. Mymensingh Med J 17: 17–21.
- Charlton F, Tooher J, Rye KA (2014) Hennessy A: Cardiovascular risk, lipids and pregnancy: preeclampsia and the risk of later life cardiovascular disease. Heart Lung Circ 23: 203-212.
- Bartels A, Egan N, Broadhurst DI, Khashan AS, Joyce C (2012) Maternal serum cholesterol levels are elevated from the 1st trimester of pregnancy: A cross-sectional study. J Obstet Gynaecol 32: 747–52.
- Koukkou E, Watts GF, Lowy C (1996) Serum lipid, lipoprotein and Apo lipoprotein changes in gestational diabetes mellitus: a cross-sectional and prospective study. J Clin Pathol 49: 634–637.
- Wiznitzer A, Mayer A, Novack V, Sheiner E, Gilutz H, et al. (2009) Association of lipid levels during gestation with preeclampsia and gestational diabetes mellitus: a population-based study. Am J Obstet Gynecol 201: 482.
- Ferriols E, Rueda C, Gamero R, Vidal M, Payá A (2016) Relationship between lipid alterations during pregnancy and adverse pregnancy outcomes. Clin Investig Arterioscler 28: 232-244.
- Sattar N, Greer IA, Galloway PJ, Packard CJ, Shepherd J (1999) Lipid and lipoprotein concentrations in pregnancies complicated by intrauterine growthrestriction. J Clin Endocrinol Metab 84: 128-130.
- Jin WY, Lin SL, Hou RL, Chen XY, Han T (2016) Associations between maternal lipid profile and pregnancy complications and perinatal outcomes: a population-based study from China. BMC Pregnancy Childbirth 16: 60.
- Vrijkotte TG, Krukziener N, Hutten BA, Vollebregt KC, Van EM (2012) Maternal lipid profile during early pregnancy and pregnancy complications and outcomes: the ABCD study. J Clin Endocrinol Metab 97: 3917-3925.
- Bharathi KR, Vijayalakshmi S, Shrunga RP (2017) A study of lipid parameters among GDM and non GDM pregnant women: a hospital based study. Int J Reprod Contracept Obstet Gynecol 6: 5488-5490.
- Han ES, Krauss RM, Xu F, Sridhar SB, Ferrara A (2016) Prepregnancy Adverse Lipid Profile and Subsequent risk of Gestational Diabetes. J Clin Endocrinol Metab 101: 2721-2727.
- Chandi A, Sirohiwal D, Malik R (2015) Association of early maternal hypertriglyceridemia with pregnancy-induced hypertension. Arch Gynecol Obstet 292: 1135–1143.
- Anaelechi JO, Japhet MO, John UU (2015) Evaluation of high-sensitivity c-reactive protein and serum lipid profile in southeastern nigerian women with Pre-Eclampsia, Departments of a Chemical Pathology and Obstetrics and Gynaecology, College of Health Sciences, Nnamdi Azikiwe University, Nnewi, Nigeria. Med Princ Pract 24: 276–279.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi