Research Article, Int J Cardiovasc Res Vol: 9 Issue: 1
Predictors of Complications During Percutaneous Multitrack Balloon Mitral Valvuloplasty
Mohamed Ahmed Sabry1* and Said Shalaby Montaser2
1Department of Cardiology, Mabaret Misr Elkhadim Hospital, Egypt
2Department of Cardiology, Faculty of Medicine, Menoufiya University, Egypt
*Corresponding Author: Mohamed Ahmed Sabry
Department of Cardiology, Mabaret Misr Elkhadim Hospital, Egypt
Tel: +01020379222
E-mail: drsabryegypt@gmail.com
Received: February 05, 2020 Accepted: February 24, 2020 Published: March 02, 2020
Citation: Sabry MA, Montaser SS (2020) Predictors of Complications During Percutaneous Multitrack Balloon Mitral Valvuloplasty. Int J Cardiovasc Res 9:1. doi: 10.37532/icrj.2020.9(1).393
Abstract
Introduction: Mitral Stenosis (MS) is characterized by a decrease in Mitral Valve (MV) orifice area leading to compromised left ventricular filling. The consequence is stagnation of blood proximal to the MV that results in elevated left atrial, pulmonary venous, and pulmonary artery pressure. Aim of the work: Trace the complication of mitral regurgitation during the procedure percutaneous Balloon Mitral Valvuloplasty (PMV) by using multitrack balloon. Subjects and methods: This interventional non-randomized cohort study was conducted on 121 patients who presented with moderate to severe MS and subjected to PMV using multitrack balloon technique and were divided into 2 groups, according to resultant mitral regurgitation: Group A: included patients with no or mild mitral regurgitation and Group B: included patients with severe mitral regurgitation. Results: Multivariate regression identified MV balloon sizing (OR 3.877, CI 95% 1.131-13.289, P value 0.031), MV commissural asymmetry (OR 67.48, CI 95% 5.759-790.72, P value 0.001). Conclusion: Mitral valve calcification, balloon sizing and MV asymmetry are significant factors that can predict the development of severe MR after balloon valvuloplasty.
Keywords: Mitral valvuloplasty; Percutaneous multitrack Balloon; Mitral stenosis
Introduction
Mitral stenosis (MS) is characterized by a decrease in Mitral Valve (MV) orifice area leading to compromised left ventricular filling. The consequence is stagnation of blood proximal to the MV that results in elevated left atrial, pulmonary venous, and pulmonary artery pressure [1].
MS most often occurs decades after the occurrence of rheumatic fever. However, in developed countries, calcific changes of the mitral annulus cause Degenerative MS (DMS) in a sizeable proportion of patients, especially in the elderly [2].
Before the appearance of percutaneous therapy, the treatment of MS was dependable on and the range of techniques included open or closed commissurotomy and replacement with biological or mechanical prostheses. Later, the development of percutaneous devices allowed percutaneous balloon mitral valvuloplasty (PMV) to become, beginning in the 1980s, not only a valid alternative to surgery but also the procedure of choice for all MS patients with a favorable valve anatomy. Percutaneous balloon mitral valvuloplasty is a safe and cheap procedure, which does not require general anesthesia. It is not a contraindication for subsequent surgical valvuloplasty or valve replacement, and does not require permanent anticoagulant therapy, except for a few cases, such as atrial fibrillation, major dilation of the left atrium, or prior episodes of embolism [3].
Acute severe mitral regurgitation (MR) is the commonest complication which needs emergency surgery following a balloon mitral valvuloplasty (BMV). The structure of the mitral valve apparatus is a complex one and BMV can sustain injury to different components of the valve apparatus [4].
We aim in this study to trace the complication of mitral regurgitation during the procedure percutaneous balloon mitral valvuloplasty by using multitrack balloon.
Subjects and Methods
This interventional non-randomized cohort study was conducted on 121 patients who presented with moderate to severe MS and subjected to PMV using multitrack balloon technique in the period from October 2017 until October 2019. This study was conducted in cardiac catheterization laboratory in cardiology department in Menoufiya University hospitals. Local ethical committee approval was taken. Participating subjects were counseled, and written consents were taken as well.
The recruited patients were divided into 2 groups, according to resultant mitral regurgitation: Group A: included patients with no or mild mitral regurgitation and Group B: included patients with severe mitral regurgitation.
All cases presented with moderate to severe mitral stenosis, suitable mitral valve morphology, symmetric commissural morphology and both sexes were included. Exclusion criteria were presence of left atrial (LA) thrombi in transesophageal echocardiography, high echocardiography score, moderate to severe mitral regurgitation, and sever calcification of both commissures.
All patients were subjected to full history taking, general examination, Body Mass Index (BMI), Body Surface Area (BSA), systemic examination and Intraoperative and post-operative transthoracic echocardiography including ejection fraction (EF), right Ventricular Systolic Pressure (RVSP), mitral valve measurements and LA measurements.
PMV was performed by The Multi-Track System technique. Left Atrial (LA), right ventricle and pulmonary artery pressures were measured before and immediately after PMV. Pre and post procedure, Mitral Valve (MV) area and MR were graded by Echocardiography.
The Multitrack balloon sizing was done by effective balloon dilatation area EBDA by using standard geometric formula [5].
Statistical analysis
The data were coded, entered and processed on computer using SPSS (version 24). The results were represented in tabular and diagrammatic forms then interpreted. Mean, standard deviation, range, frequency, and percentage were use as descriptive statistics.
Results
Table 1 shows that Pre-commissurotomy, mild AR was present in 51 patients (42.1%), MV commissural calcification in 22 patients (18.2%), MV commissural asymmetry in 17 patients (14.0%), mild MR in 51 patients (42.1%) and AF rhythm in 45 patients (37.2%). No reported cardiac tamponade, cardiac perforation, new onset mitral regurgitation or death.
| Frequency | |
|---|---|
| Pre-commissurotomy Mild AR | 51 (42.1%) |
| Pre-commissurotomy MV commissures calcification | 22 (18.2%) |
| Pre-commissurotomy MV commissures Asymmetricity | 17 (14.0%) |
| Pre-commissurotomy Mild MR | 51 (42.1%) |
| Pre-commissurotomy AF | 45 (37.2%) |
| Severe MR post-MV commissurotomy | 12 (9.9%) |
| AF post-MV commissurotomy | 45 (37.2%) |
| Cardiac tamponade | - |
| Cardiac perforation | - |
| New onset mitral regurgitation | - |
| Death | - |
Table 1: Aortic and mitral valves morphology and ECG rhythm pre-MV commissurotom.
Table 2 shows that patients who developed severe MR postcommissurotomy of higher physical dimensions. They had higher weight (79.7 ± 0.9 versus 73.6 ± 7.5, P value<0.001). They were also taller (height: 173.7 ± 4.9 versus 166.9 ± 5.4, P value<0.001). They had higher BMI (36.6 ± 0.7 versus 32.7 ± 6.4, P value<0.001). They showed higher BSA (2.0 ± 0.0 versus 1.8 ± 0.1, P value<0.001).
| No or mild MR | Severe MR | P value | |
|---|---|---|---|
| Age | 35.3±10.1 | 34.1±3.6 | 0.383 |
| Gender (male) | 46 (42.2%) | 4 (33.3%) | 0.394 |
| Weight | 73.6±7.5 | 79.7±0.9 | <0.001 |
| Height | 166.9±5.4 | 173.7±4.9 | <0.001 |
| BMI | 32.7±6.4 | 36.6±0.7 | <0.001 |
| BSA | 1.8±0.1 | 2.0±0.0 | <0.001 |
Table 2: Comparison of physical measurements of recruited patients.
In Table 3, univariate regression identified BMI (OR 1.108, CI 95% 1.002-1.224, P value 0.045), EF (OR 1.16, CI 95% 1.015-1.326, P value 0.029), MV commissural calcification (OR 5.812, CI 95% 1.666- 20.283, P value 0.006), MV commissural asymmetry (OR 37.875, CI 95% 8.520- 168.361, P value<0.001) and MV balloon size (OR 2.592, CI 95% 1.366-4.918, P value 0.004).
| Exp(B) | P value | 95% C.I. for EXP(B) | ||
|---|---|---|---|---|
| BMI | 1.108 | 0.045 | 1.002 | 1.224 |
| EF | 1.16 | 0.029 | 1.015 | 1.326 |
| Wilkins score | 1.785 | 0.052 | 0.996 | 3.2 |
| MV commissures Calcifications | 5.812 | 0.006 | 1.666 | 20.283 |
| MV commissures Asymmetricity | 37.875 | <0.001 | 8.52 | 168.361 |
| MR | 4.97E+08 | 0.997 | 0 | |
| Balloon sizing | 2.592 | 0.004 | 1.366 | 4.918 |
Table 3: Univariate regression for predicting severe MR post commissurotomy.
In Table 4, multivariate regression identified MV balloon sizing (OR 3.877, CI 95% 1.131-13.289, P value 0.031), MV commissural asymmetry (OR 67.48, CI 95% 5.759-790.72, P value 0.001).
| Exp(B) | P value | 95% C.I. for EXP(B) | ||
|---|---|---|---|---|
| Balloon sizing | 3.877 | 0.031 | 1.131 | 13.289 |
| BMI | 1.159 | 0.208 | 0.921 | 1.459 |
| EF | 1.135 | 0.173 | 0.946 | 1.363 |
| MV commissures Calcifications | 1.574 | 0.715 | 0.138 | 17.889 |
| MV commissures Asymmetricity | 67.48 | 0.001 | 5.759 | 790.72 |
Table 4: Multivariate regression for predicting severe MR post commissurotomy.
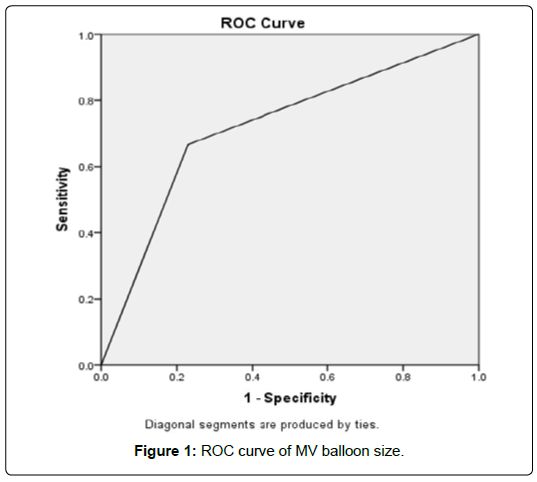
Figure 1 shows ROC analysis was done to determine possible MV balloon size that is associated with possibility of severe MR post-commissurotomy. ROC showed that size of ≥ 17 showed sensitivity of 66.7% and specificity of 7.1% with area under curve (AUC) of 0.719.
Discussion
Mitral Stenosis (MS) is almost invariably the result of chronic rheumatic heart disease secondary to one or more prior episodes of acute rheumatic fever. Since In otto et al. [6] introduced balloon valvuloplasty in 1984, this procedure has become the treatment of choice replacing surgical commissurotomy in many cases. Despite the high technical expertise in percutaneous mitral commissurotomy, mitral regurgitation remains a major procedure-related complication [7].
Actually PMC is an effective procedure for MS with any of its technique either by Inoue balloon (IB), metallic commissurotomy (PMMC), or Multi-Track Double Balloon (MTDB) as in the study of Sharieff et al. [8] where a total of 486 patients were subjected to PMV using any of the 3 techniques and the overall success rate was 97.3% for IB, 97.6% for PMMC, and 98.3% for MTDB. Overall, the transmitral gradient decreased from 20.7 ± 7.2 mmHg to 6.5 ± 3.7 mmHg (p<0.001) and Left atrial pressure decreased from 29.3 ± 8.4 mmHg to 16.1 ± 11.5 mmHg (p< 0.001) [8].
Also, in Egyptian study of Sherif et al. [9] mean pressure gradient dropped from 15.94 ± 5.46 mmHg to 5.85 ± 2.6 mmHg by different techniques of PMV and the Multi- Track system was able to induce largest increase in MV area [9].
Regarding Post-commissurotomy MR, 12 patients developed severe MR (9.9%) in the current study who were compared with other patients to identify important distinction points. Sever MR group showed significant higher weight, height, BMI and BSA (P value>0.001).
Higher incidence (13.3%) of severe MR was observed by Elsawy et al. [10] in his study since four of 30 patients who underwent multitrack PMV developed severe MR. However, in the study of Sadaka et al. [11] on 30 patients who underwent PBMV no one developed severe MR even after follow up of 3 months [11]. In addition, Hou et al [12] observed severe MR in 12 out of 1768 patients (0.68%) underwent PBMV.
In the current study there was no significant difference between the two studied groups regarding age or sex (P value=0.383, 0.394 respectively). In the same point of view, Elasfar and Elsokkary did not find significant difference between patients with post-Inoue PMV severe MR and other patients without severe MR regarding their age or sex [7].
Pre-operative RVSP in the current study was significantly higher among patients with severe MR (37.3 ± 2.0 for severe MR versus 35.0 ± 3.2, P value 0.002).
This is in agreement with Farman et al, who showed that high RV pressure was correlated with unsuccessful procedures. They confirmed their results by multivariate logistic regression which showed that RV pressure is a significant predictive factor for a successful PTMC [13].
Regarding balloon sizing, it was significantly higher among patients who developed severe MR compared with patients with mild or no MR (P value 0.001).
Tastan et al. [14] studied 2 groups of patients undergoing PBMV. One group was allocated to conventional height-based balloon reference sizing (the HBRS group) and the other was allocated to balloons sized by the echocardiographic measurement of the diastolic inter-commissural diameter (the EBRS group). They noticed that the mean of the calculated balloon reference sizes was significantly higher in the HBRS than in the EBRS group and MR > 2+ was less in the EBRS group [14].
Finally, it is obvious that several factors can predict the development of severe MR after multi-track PMV as MV calcification, balloon sizing and MV asymmetry. It also must be noted that this study is the first one to concentrate on predictors of severe MR after multi-track PMV. However, the current study has some limitations that must be mentioned including absence the correlation with MV area and absence the comparison with outcomes of other techniques to detect the general role of procedure in developing MR.
Conclusion
Mitral valve calcification, balloon sizing and MV asymmetry are significant factors that can predict the development of severe mitral regurgitation after balloon valvuloplasty.
Recommendations
a) Special attention should be paid to patients with higher BMI, MV calcification and MV asymmetry.
b) Patients should be counseled about the risk of developing MR after the procedure and patients with higher BMI, MV calcification and MV asymmetry should know about their higher risk.
c) Great attention should be conducted to choose a small balloon whenever possible.
References
- Pressman GS, Ranjan (2018) Aetiology and epidemiology of mitral stenosis. E-Journal of Cardiology Practice 16: 14.
- Iung B, Vahanian A (2011) Epidemiology of valvular heart disease in the adult. Nat Rev Cardiol 8: 162-172.
- Capodanno D, Barbanti M, Tamburino C (2018) Mitral stenosis: percutaneous treatment of left side cardiac valves. (2nd Edition), Springer international publishing.
- Pillai AA, Balasubramonian VR, Munuswamy H, Seenuvaslu S (2019) Acute severe mitral regurgitation with cardiogenic shock following balloon mitral valvuloplasty: echocardiographic findings and outcomes following surgery. Cardiovasc Interv Ther 34: 260-268.
- Roth RB, Block PC, Palacios IF (1990) Predictors of increased mitral regurgitation after percutaneous mitral balloon valvotomy. Cathet Cardiovasc Diagn 20: 17-21.
- Otto C, Bonow R (2014) Valvular heart disease: A companion to braunwald's heart disease(3rd Edition), Elsevier saunders,Philadelphia 2014: 255-277.
- Elasfar AA, Elsokkary HF, (2011) Predictors of developing significant mitral regurgitation following percutaneous mitral commissurotomy with inoue balloon technique. Cardiol Res Pract 1: 312-319.
- Sharieff S, Aamir K, Sharieff W, Tasneem H, Masood T, et al. (2008) Comparison of Inoue balloon, metallic commissurotome and multi- track double-balloon valvuloplasty in the treatment of rheumatic mitral stenosis. J Invasive Cardiol 20: 521-525.
- Sherif MA, Khashaba AA, Gomaa Y, Khaled S, Refaie O, et al. (2009): Pooled analysis of percutaneous mitral valvuloplasty in Egypt. Catheter Cardiovasc Interv 73: 419-425.
- Elsawy E, Allam S, Elabbady M (2009) Evaluation of the immediate and short-term results of mitral valvuloplasty using the multitrack balloon versus metallic. AAMJ 7: 246–257.
- Sadaka MA, Elsharkawy EM, Ali RA, Rashwan MA (2012) The impact of commissural morphology on clinical outcome in patients undergoing percutaneous balloon mitral valvuloplasty. Egypt Hear J 64: 233-240.
- Hou ZS, Ou ZH, Wei YJ, Hou YM, Shao MF, et al. (2009) Long-term outcome of percutaneous balloon mitral valvuloplasty in patients with rheumatic mitral valve stenosis. Zhonghua xin xue guan bing za zhi 37: 994–997.
- Farman MT, Khan N, Sial JA, Saghir T, Ashraf T, et al. (2015) Predictors of successful percutaneous transvenous mitral commissurotomy using the bonhoeffer multi-track system in patients with moderate to severe mitral stenosis: Can we see beyond the Wilkins score?. Anatol J Cardiol 15: 373–379.
- Tastan A, Ozturk A, Senarslan O, Ozel E, Uyar S, et al. (2016) Comparison of two different techniques for balloon sizing in percutaneous mitral balloon valvuloplasty: Which is preferable?. Cardiovasc J Afr 27: 147-151.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi