Case Report, Res Rep Gastroenterol Vol: 2 Issue: 1
Primary Acquired Gastric Outlet Obstruction in Pediatrics (Jodhpur Disease) How to Manage? A Report of Two Cases
Takrouney MH*, Sabra TA, Ibrahim H and Ahmed MEL
Pediatric Surgery Unit, Faculty of Medicine, Assiut University, Assiut Government, Egypt
*Corresponding Author : Mohammed Hamada Takrouney
Pediatric Surgery Unit, Faculty of medicine, Assiut University, Assiut Government, Egypt
E-mail: m.takrouney1988@aun.edu.eg or m.takrouney1988@gamil.com
Received: November 21, 2017 Accepted: December 29, 2017 Published: January 03, 2018
Citation: Takrouney MH, Sabra TA, Ibrahim H, Ahmed MEL (2018) Primary acquired Gastric Outlet Obstruction in Pediatrics (Jodhpur Disease) How to Manage? A Report of Two Cases. Res Rep Gastroenterol 2:1
Abstract
Pediatric gastric outlet obstruction is a relatively common condition, sonographic evaluation of gastric muscular wall thickness and pyloric canal length can exclude congenital hypertrophic pyloric stenosis from primary gastric outlet obstruction (GOO) which is a rare disease. Herein, we reported two cases of GOO which, were treated surgically by Pyloroplasty and Gastrojejunostomy.
Keywords: Gastric outlet obstruction; Pyloroplasty; Gastrojejunostomy
Introduction
Gastric outlet obstruction (GOO) is a rare structural abnormality of unknown etiology in which clinical and pathophysiological consequences produce mechanical impediment emptying of gastric content into duodenum [1]. Nausea and non-bilious vomiting are the characteristic symptoms [2].
Primary acquired GOO in children is a separate entity from Congenital Hypertrophic Pyloric Stenosis (CHPS), congenital intrinsic obstruction and other extrinsic causes of obstruction [3]. We present two cases of recurrent non-bilious vomiting, which resulted in severe malnutrition.
This condition was intractable by medical treatment and so exploration of both cases was done and revealed in dilated stomach and no muscular hypertrophy of pylorus, Pyloroplasty was done in one case and Gastrojejunostomy was done in the second case and patients improved.
Case Reports
Case 1
A 3-month-old male child was complaining of repeated nonbilious, projectile vomiting, 3-4 times daily after breast feeding by about 1 hour for 1month. Normal bowel habits, with significant weight loss (2 kg in one month). No history of caustic ingestion, no jaundice, no fever or history of contact with Tuberculosis patient.
On examination: Generally, the patient was malnourished, dehydrated, his weight was 2 kg and his height was 50 cm. Abdominal examination showed epigastric distention; reversed peristalsis (from the right to the left of the abdomen) noticed after breast feeding, no palpable olive tumor (pathognomonic sign of CHPS), no organomegaly, with a tympanic note on percussion, other systems were with no abnormality.
Laboratory investigations: Revealed normal hemoglobin, hypoalbumenia, hypernatremia and hypokalemia.
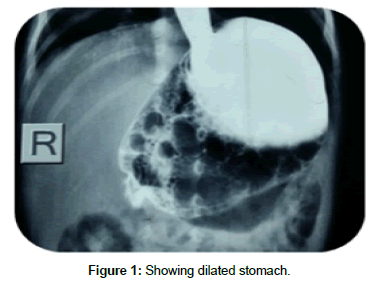
Abdominal ultrasonography: Revealed dilated stomach (Figure 1), normal wall thickness and normal pyloric canal length.
Gastrograffin meal showed dilated stomach, delayed gastric emptying, no duodenal dilatation or Gastro esophageal reflux.
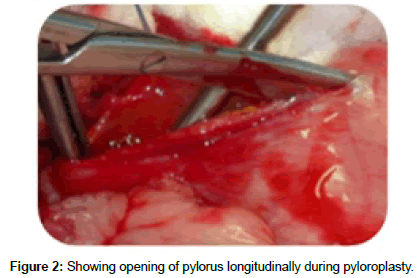
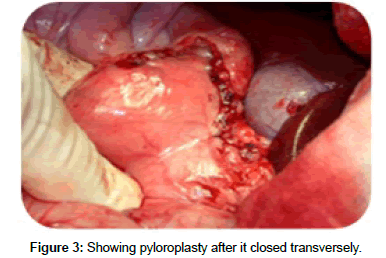
After improvement of general condition, under general anesthesia the abdomen was examined, and no palpable masses were found. Exploration the of abdomen revealed dilated stomach and smooth stenosed pylorus Heinke-Mickulicz Pyloroplasty was done (opening of the pylorus longitudinally (Figure 2) and closed transversaly (Figure 3)). Sub-hepatic drain was left, 48 hours later, the patient started oral feeding with sporadic attacks of vomiting responded to antiemetic medications, patient was discharged and was followed up after one month. The patient was well and gaining weight (5 kg).
Case 2
2-years-old male child, presented by frequent non-bilious vomiting (5-6 times) after oral feeding since age of 2 months, with abdominal pain increased by eating and relieved by vomiting, normal bowel habits, no history of caustic ingestion and no history of hematemesis.
Examination: Patient was pale, malnourished and with delayed growth, his weight was 5 kg and his height was 53 cm. cm.
Abdominal examination: moderate abdominal distention mainly epigastric, no organomegaly, tympanic note in percussion increased in epigastrium and normal audible intestinal sounds..
Laboratory investigations: Low hemoglobin level, thrombocytopenia, hypoalbumenia and hypokalemia.
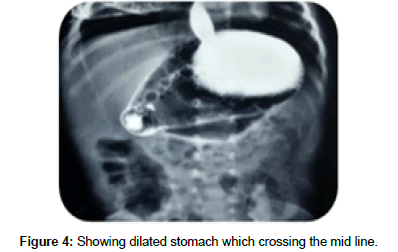
Abdominal ultrasound: Showed dilated stomach, its wall thickness was 4mm, normal pyloric canal length (Figure 4).
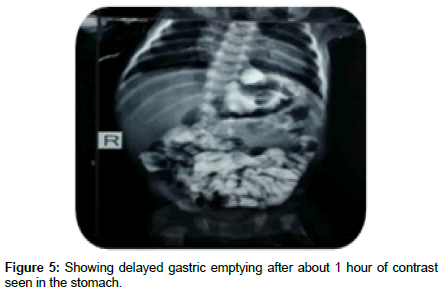
Gastrograffin meal: Showed dilated stomach, delayed gastric emptying (Figure 5), no gastro esophageal reflux.
Upper endoscopy: revealed stenosis of pyloric canal, trials of balloon dilation were done, but failed a biopsy was taken, and surgical correction was advised. Histopathological examination revealed no abnormalities, a part of congestion and wall edema. Abdominal exploration revealed dilated thick-walled stomach, with mild fibrosis of the pylorus and normal other organs. Iso peristaltic, retro colic, gastrojejunostomy was made, sub hepatic drain was left, and the abdomen was closed anatomically. The postoperative course was uneventful, and the patient was discharged from the hospital on the postoperative day 3.
Discussion
Late onset GOO in children ranging from 3 months to 6 years without intrinsic or extrinsic cause is very rare [4]. Several names have been used for describing this disease including GOO during infancy and childhood [4], primary acquired GOO [4,5] late onset primary GOO [6] non- obstructive delayed gastric emptying in children [7], pyloric achalasia [8], non- hypertrophic pyloric stenosis [9] and Jodhpur disease it was named after the city in which the first case has been discovered [10].
The etiology of the disease has remained poorly understood, it has been suggested that localized pyloric neurotransmitter incoordination caused by lack of nitric oxide synthase enzyme, that has been the main inhibitory neurotransmitter of lower esophageal sphincter and pylorus [11,12]. Other hypothesis claims that abnormality of interstitial cells of Cajal which is peacemaker of gastrointestinal tract [13].
The disease occurs mainly in males with incidence of 1:100,000 live births [14], it characterized by intractable vomiting, weight loss and growth retardation. Using abdominal US and Gastrograffin meal can help in diagnosis of the disease.
Many therapeutic options for treatment of GOO in children, non-operative lines of treatment including pneumatic balloon dilatation and botulinum toxin and operative treatment including Heinke-Mickulicz Pyloroplasty and Gastrojejunostomy, but surgical management remains the standard curative therapeutic option for management of Jodhpur disease.
Conclusion
Primary acquired GOO is very rare disease and child cannot digest food over period of time and this result in marked weight loss and growth retardation, its clinical presentation which similar to CHPS but in older infants, and children should be strongly suspect of primary acquired GOO.
Because of rarity of primary acquired GOO, it is difficult to detect best therapeutic option (operative and non-operative) which need large studies.
References
- Sharma KK, Agrawal P, Toshniwal H (1997) Acquired gastric outlet obstruction during infancy and childhood: a report of five unusual cases. J Pediatr Surg 32: 928-930.
- Abuhandan M, Caksen H, Eskicubuk S (2004) A case of acquired gastric outlet obstruction diagnosed at 16 years of age. Pediatr Surg Int 20: 148-150.
- Nazir Z, Arshad M (2005) Late-onset primary gastric outlet obstruction an unusual 3-cause of growth retardation. J Pediatr Surg 40: E13.
- Jawaid W, Abdalwahab A, Blair G, Skarsgard E, Webber E (2016) Outcomes of pyloroplasty and pyloric dilatation in children diagnosed with nonobstructive delayed gastric emptying. J Pediatr Surg 41:2059-2061.
- Lin JY, Lee ZF, Yen YC, Chang YT (2007) Pneumatic dilation in treatment of lateonset primary gastric outlet obstruction in childhood. J Pediatr Surg 42: e1-4.
- Hameury F, Mcheik J, Lardy H, Gaudina J, Petit T, et al. (2007) Acquired non hypertrophic pyloric stenosis in children. Arch Pediatr 14: 330-333.
- Castro A, Mearin F, Gil-Vernet JM, Malagelada JR (1997). Infantile hypertrophic pyloricstenosis and achalasia: NO-related or non-related conditions. Digestion 58: 596-598.
- Vanderwinden JM, Mailleux P, Schiffmann S, Vanderhaeghen JJ, De Laet (1992) MH Nitric oxide synthase activity in infantile hypertrophic pyloric stenosis. N Eng J Med 327: 511-515.
- Takahashi T (2003) Pathophysiological significance of neuronal nitric oxide synthase in the gastrointestinal tract. J Gastroenterol 38: 421-430.
- Ceccanti S, Mele E, Frediani S, Di Nardo G, Roggini M, et al. (2012) Laparoscopic pyloroplasty for idiopathic non-hypertrophic pyloric stenosis in a child. J Pediatr Surg 47: 1955-1958.
- Sharma KK, Ranka P, Goyal P, Dabi DR (2008) Gastric outlet obstruction in children an overview with report of “Jodhpur disease” and Sharma's classification. J Pediatr Surg 43: 1891-1897.
- Karnsakul W, Cannon ML, Gillespie S, Vaughan R (2010) Idiopathic non-hypertrophic pyloric stenosis in an infant successfully treated via endoscopic approach. World J Gastrointest Endosc 2: 413-416.
- Islam S1, Vick LR, Runnels MJ, Gosche JR, Abell T (2008) Gastric electrical stimulation for children with intractable nausea and gastroparesis. J Pediatr Surg 43: 437-442.
- Teich S, Mousa HM, Punati J, Di Lorenzo C (2013) Efficacy of permanent gastric electrical stimulation for the treatment of gastroparesis and functional dyspepsia in children and adolescents. J Pediatr Surg 48: 178-183.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi