Case Report, Res Rep Gastroenterol Vol: 5 Issue: 3
Recurrent Sigmoid Volvulus in Third Trimester Pregnancy: A Case Report
Monika Shenouda*, Monir Mardini, Abiola Mosuro, Syed Saad Uddin, Katerina Yu, Armaity Austin and Gudata Hinika
Department of Family Medicine, Dignity Health California Hospital Medical Center, Los Angeles, CA
*Corresponding Author: Monika Shenouda
Department of Family Medicine, Dignity Health California Hospital Medical Center, Los Angeles, CA
Tel: 949 400 0091
E-Mail: monikamagdy@g.ucla.edu
Received date: April 15, 2021; Accepted date: April 30, 2021; Published date: May 7, 2021
Citation: Shenouda M, Mardini M, Mosuro A, Uddin SS, Yu K, et al (2021) Recurrent Sigmoid Volvulus in Third Trimester Pregnancy: A Case Report and Review of the Literature. Res Rep Gastroenterol 5:3.
Abstract
We present the case of a 34 year old female Gravida 5 Para 4 at 33 weeks and 4 days gestation who presented with lower abdominal pain and constipation. MRI Abdomen and Pelvis demonstrating large bowel obstruction secondary to Sigmoid Volvulus (SV). Patient was initially managed with colonoscopic detorsion but with recurrence of volvulus during the same hospitalization. The second event of volvulus was again treated with colonoscopic detorsion. The patient underwent a C-section due to the recurrence to the volvulus at 34 weeks and 2 days, with the delivery of a pre-term female infant, and exploratory laparotomy concomitantly with bowel resection of the sigmoid and descending colon and colostomy formation. Both procedures were tolerated well by both mother and child without complications. The extremely low incidence of SV along with masking of the clinical presentation by a gravid uterus lead to delay in diagnosis, which is the main reason for devastating outcomes including bowel ischemia, necrosis, perforation and both fetal and maternal death. An effective multidisciplinary approach and prompt diagnosis are critical.
Keywords: Sigmoid Volvulus; Pregnancy: Large Bowel Obstruction
Introduction
Colonic Volvulus remains one of the rare causes of intestinal obstruction in the United States with Sigmoid Volvulus accounting for 2% to 5% of all colonic obstructions [1]. Although the etiology of Sigmoid Volvulus is multifactorial, it has been shown that elongation and dilation of the Sigmoid with its accompanying mesentery results in a redundant loop of bowel that becomes prone to rotation around the mesenteric axis [2]. In the event of rotation, progression to life- threatening complications such as bowel ischemia, perforation, gangrene may occur. The patient population in the Western World commonly centers on the elderly, patients in long term care facilities, and those institutionalized with psychiatric illness. Amongst these populations, chronic constipation is a shared, contributing factor responsible for the increased risk of Sigmoid Volvulus. However, a population in other parts of the world such as Africa and India are more commonly young healthy men whose diet is rich in fiber [3].
Both chronic constipation and a high fiber diet increase the stool load and lead to dilation in the sigmoid colon, making it more susceptible to torsion. Treatment options for uncomplicated events include barium enema and rectal tube and flexible sigmoidoscopy [4,5]. In the setting of complications such as bowel ischemia, gangrene or perforation leading to acute abdomen or recurrence of Volvulus after non operative management, sigmoid resection with primary anastomosis or stoma is the preferred modality of surgical treatment [6]
A patient population that is uncommonly associated with Sigmoid Volvulus are women in the late stages of pregnancy, estimated to occur between 1 in 1500 to 1 in 66431 deliveries [1,2,7]. Volvulus may arise when an intra-pelvic mass or mass effect caused by the gravid uterus causes significant pressure and displacement of the previously elongated and dilated sigmoid colon. Late diagnosis of the volvulus due to the overlapping of clinical signs and symptoms between obstruction and pregnancy may also contribute to the high rate of mortality for both mother and fetus, estimated at 20% and 40%, respectively [7]. Further issues regarding peri-partum radiation exposure and subsequent negative outcomes on the fetus have also made radiographic diagnosis challenging. As such no specific management paradigm has been proposed in literature specifically outlining the risks and benefits of early surgical intervention and c- section in such events. We present a case of a 34 year old Female Gravida 5 Para 4 at 33 weeks and 4 days gestation that after repeated events of Sigmoid Volvulus within the same hospitalization elected to undergo C-section and sigmoid resection with stoma creation at 34 weeks and 2 days gestation.
Case Report
A 34-year-old woman, gravida 5, para 4, presented at 33 weeks and 4 days gestation of an otherwise uneventful pregnancy, with intermittent sharp lower abdominal pain and constipation for 4 days. She endorsed nausea but no history of vomiting or fever. Her previous pregnancies consisted of two normal spontaneous vaginal deliveries and two C-sections, respectively, without complications. On examination, she was afebrile, with bilateral lower abdominal tenderness. Sterile vaginal examination showed a closed cervix with irritable contractions on the tocometer. Laboratory studies revealed elevated white blood cell count of 13,700 with all other labs within normal limits. Urinalysis was negative for urinary tract infection. Obstetrics ultrasound showed no abnormalities. She was given terbutaline, fleet enema and bisacodyl suppository. Abdominal pain initially improved with bowel movement and she was discharged home.
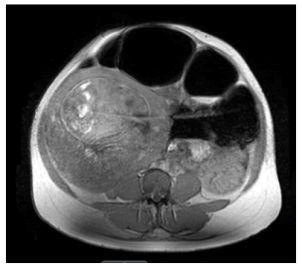
However, the patient returned the next day with a similar presentation of abdominal pain. It was clear that the patient was not in preterm labor as the cervix remained closed and no signs of fetal distress or abnormality on ultrasound. Her pain continued to worsen and it was necessary to explore other etiologies of the abdominal pain. Complete abdominal ultrasound showed fluid collection in the left lower quadrant of the abdomen measuring 2.3 × 3.0 × 7.7 cm. Subsequent MRI of the abdomen showed suspected Sigmoid Volvulus resulting in obstruction of the colon which was prominently dilated with air-fluid levels and a collapsed appearance of the distal sigmoid colon and rectum (Figures 1 and 2).
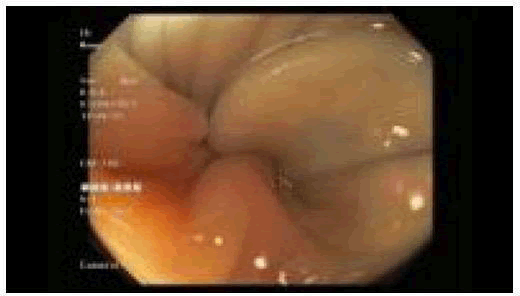
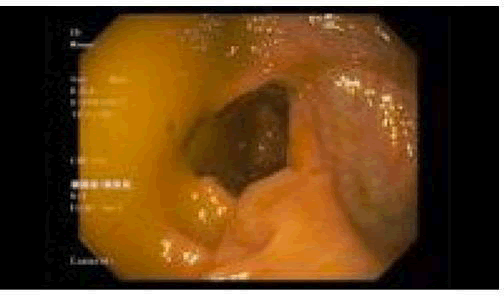
She underwent urgent colonoscopy with successful detorsion and decompression of the Sigmoid Volvulus (Figures 3 and 4). She then reported improvement of abdominal pain with two subsequent bowel movements hours post-detorsion.
The day after the colonoscopy, similar symptoms of the abdominal pain returned. With high suspicion of recurrence, she underwent another colonoscopy with another successful detorsion of the sigmoid volvulus. Fetal heart tones were monitored continuously, before and after the procedures.
Due to the recurrence of the volvulus, she was scheduled the next day at weeks 34 and 2 days for a C-section and exploratory laparotomy concomitantly via vertical midline incision of the skin and fascia with a low transverse incision of the uterus which resulted in the delivery of a preterm female infant with APGARS 8 and 9 and followed by bowel resection of sigmoid and descending colon and colostomy formation. Gross pathology examination revealed a dilated and twisted large bowel measuring 35 × 9 cm with lumen filled with air, wall edema, decreased folds and wall thickness consistent with the clinical diagnosis of volvulus (Figures 5 and 6). No granuloma, dysplasia or malignancy was identified. The patient was discharged on post operative day 3 without complications.
Discussion
Bowel obstruction during pregnancy is quite rare. In 44% of the cases of bowel obstruction in pregnancy, Sigmoid Volvulus [SV] is the cause of the bowel obstruction with an increased incidence in the third trimester of gestation thought to be due to the gravid uterus compressing and displacing the sigmoid colon or causing twisting of a longer than average sigmoid colon [7]. It is also difficult to differentiate the gastrointestinal root cause from gynecologic root cause for pain which is why identification of cases of SV during pregnancy is prolonged. Classic symptoms of SV including vomiting, abdominal distention, pain and constipation also correspond to regular pregnancy related complaints [8,9]. This can be deciphered from the fact that the uterus, cervix, and adnexa share the same visceral innervations as the terminal ileum, sigmoid colon, and rectum [10]. Our patient presented with all these classic symptoms.
Several conditions that demonstrate a higher incidence of SV include, high fiber diet, chronic constipation, neuropsychiatric disorders, and my opathies; however, the most prevalent risk factors that are understood thus far include, Hirschprung’s disease, enlarged colon, intestinal mal rotation, abdominal adhesions, and as in our case, pregnancy [11,12]. Our patient presented with a third trimester pregnancy, as well as, a significant past surgical history of two cesarean sections. Abdominal adhesions are common after C-sections and their incidence is increased with each subsequent procedure leading to a significant morbidity of bowel obstructions [13].
In the general population, the mortality rate for SV ranges from 0- 40% [14,15]. Furthermore, in a recent review, the prospective mortality rates for pregnancy with SV demonstrated 20% maternally and 40% fetal mortality; however, maternal and fetal mortality in these patient sis directly correlated to the degree of bowel is chemia and subsequent sepsis [7]. A grave associated complication of SV is sigmoid gangrene, seen in 6.1%-30.2% of all SV patients. The mortality rate increases from 0%-40% to 3.7%-80%, nearly doubling [15,16]. Notably, in are trospective study of 442 SV patients, there was a negative correlation between pregnancy and the development of sigmoid gangrene [14].
Fluoroscopy, radiography, and Computed Tomography (CT) are the diagnostic imaging studies of choice in SV because non-specific symptom atology makes clinical diagnosis only difficult [16]. Plain film x-ray and clinical findings only are 81.4% diagnostic; however, CT and Magnetic Resonance Imaging (MRI) are 100% diagnostic, with flexible endoscopy being always diagnostic, in the setting of SV [17]. In regards to pregnancy, the modality of imaging changes when considering the fetus; nonetheless, SV is a life-threatening complication for the mother and fetus. A delay in diagnosis and treatment of 48 hrs or more can significantly increase the maternal and fetal morbidity and mortality secondary to intestinal ischemia and colonic necrosis [18]. Prompt diagnosis and treatment are necessary to prevent maternal and fetal death.
Given that SV is a medical emergency, initial management in our case resembled conservative therapy for a non-pregnant case consisting of fluid resuscitation, NPO status, pain management and colonoscopic decompression. With no signs of peritonitis or sepsis, conservative management seemed sensible as opposed to emergent surgery in an attempt to achieve 37 weeks gestation prior to delivery. In our case, the patient underwent two consecutive endoscopic reductions of the colon both confirming no signs of bowel ischemia or perforation. Although endoscopy can be restricted by the enlarged uterus during the third trimester, this was not the case [19]. The first bowel decompression relieved pain and allowed for bowel movements so diet was advanced. However, the patient began having increased pain and became increasingly distended raising the concern for recurrent SV. This yielded another colonoscopic decompression the next day. After the second decompression, the bowel had re-volvulized which hastened the decision for surgery.
Conservative therapy with endoscopic detorsion and decompression is efficacious in 75%-95% of cases [20]. In fact, there have been effective endoscopic interventions during pregnancy to relieve obstruction and there are less than 10 cases of persisting Sigmoid Volvulus in the same pregnancy [20]. On the contrary, with pregnancy as the alluring factor for recurrence there was an increased likelihood of another episode of Volvulus. While colonoscopy during pregnancy is relatively safe in the third trimester, it still has the risks of bleeding, perforation, infection and possibly inducing early labor [20]. The risks of emergent bowel resection versus continual endoscopic decompression were weighed. It was no longer merited to continue attempting to with hold surgery until 37 weeks since survival after 34 weeks is excellent, and the patient was within 7 days of the antenatal steroid course. The multidisciplinary team including Gastroenterology, Surgery, Maternal-Fetal-Medicine, Neonatologist and OB/GY N physicians reviewed the case and agreed that caesarean section followed by sigmoid resection with Colostomy was ideal given the fact that the Volvulus was refractory to non-surgical management. Caesarean section is ideal in order for the entire bowel to be examined for other areas of obstruction [7,19]. The decision on the Hartmann Procedure instead of the sigmoid colostomy was made to avoid the complication of a leak with the anastomosis.
It was important for surgery to be done in a timely manner to avoid volvulus recurrence and complications of bowel ischemia, gangrene, perforation and sepsis that affect maternal and neonatal mortality and morbidity. Sigmoid dilatation can cause increased intra-abdominal pressure or reduce placental blood flow and contribute to fetal death [20]. Fetal complications include preterm delivery, intrauterine death and neonatal sepsis with mortality in SV is as high as 30% [7,19]. Apart from surgery, other preventative therapies are unknown and while favorable, dietary modification and stool softeners have not been proven to show short-term efficacy [8].
While there has not yet been a recurrence of SV postpartum or in following pregnancies, Alrahmani’s case of SV occurred at a similar gestational age in two successive pregnancies [8]. This hints toward uterine compression as the precipitating factor so patients who underwent successful colonoscopic decompression should be counseled and educated on the possibility of having recurrence in future pregnancies [8].
Conclusion
Although difficult to diagnose based on presenting symptoms, pregnant patients with un-resolving symptoms of abdominal distension, pain and constipation should be further evaluated for SV especially during the second and third trimesters. A high index of clinical suspicion is vital in pregnant women with signs and symptoms of intestinal obstruction to avoid any delay in diagnosis and treatment. This needs to be stressed amongst the general practitioners and community obstetricians primarily responsible for taking care of these patients.
References
- Atamanalp S S (2010) Sigmoid Volvulus. Eurasian J Med 42: 142-7.
- Le Carol K, Nahirniak P, Anand S, Cooper W (2010) Volvulus. Stat Pearls, U.S. National Library of Medicine, 7 Dec. 2020.
- Ballantyne GH, Brandner MD, Beart RW Jr, Ilstrup DM (1985) Volvulus of the colon. Incidence and mortality. Ann Surg 202: 83-92.
- Lou Z, Yu E-D, Zhang W, Meng R-G, Hao L-Q (2013) Appropriate treatment of acute sigmoid Volvulus in the emergency setting. World J Gastroenterol 19: 4979-4983.
- Quénéhervé L, Dagouat C, Rhun ML, Robles EP-C, Duchalaisa E, et al. (2018) Outcomes of First-Line Endoscopic Management for Patients with Sigmoid Volvulus. Digest Liv Dis 51: 386-390.
- Larkin JO, Thekiso TB, Waldron R, Barry K, Eustace P (2009) Recurrent sigmoid Volvulus - early resection may obviate later emergency surgery and reduce morbidity and mortality. Ann R Coll Surg Engl 91: 205-209.
- Khan MR, Rehman SU (2012) Sigmoid Volvulus in pregnancy and puerperium: A surgical and obstetric catastrophe. Report of a case and review of the world literature. Wld J Emerg Surg 7:1-5.
- LayanAlrahmani, Jaclyn Rivington, Carl H Rose. (2018) Recurrent Volvulus during pregnancy: Case Report and Review of the Literature, Case Reports in Obstetrics and Gynecology 4510754: 5.
- Serafeimidis C, Waqainabete I, Creaton A, Vakamacawai E, Kumar R (2016) Sigmoid Volvulus in pregnancy: Case report and review of literature. Clin Case Rep 4: 759-761
- Ward KE, Blake E, Gonzalez E, Pieracci F, Alston M (2017) Sigmoid Volvulus complicating postpartum period. Case Reports in Obstet Gynaecol 9034925: 1-3.
- Le Carol K, Nahirniak P, Anand S, Cooper W. Volvulus. Stat Pearls, U.S. National Library of Medicine, 7 Dec. 2020.
- Ballantyne G H, Brandner MD, Beart RW, Ilstrup DM (1985) Volvulus of the colon. Incidence and mortality. Ann Surg 202: 83-92.
- Poole JH (2013) Adhesions following cesarean delivery: A review of their occurrence consequences and preventative management using adhesion barriers. Women’s Health 9:467-477.
- Atamanalp SS, Kisaoglu A, Ozogul B (2013). Factors affecting bowel gangrene development in patients with sigmoid volvulus. Ann Saudi Med 33:144-148.
- Atamanalp SS, Disci E, Atamanalp RS (2019) Sigmoid volvulus: Comorbidity with sigmoid gangrene. Pak J Med Sci 35: 288-290.
- Peterson CM, Anderson JS, Hara AK, Carenza JW, Menias CO (2009) Volvulus of the gastrointestinal tract: Appearances at multimodality imaging. Radiographics 29:1281-93.
- Atamanalp SS (2013) Sigmoid Volvulus: Diagnosis in 938 patients over 45.5 years. Tech Coloproctol 17: 419-424.
- Al Maksoud A, Barsoum A, Moneer M (2021) Sigmoid volvulus during pregnancy: A rare non-obstetric complication. Report of a case and review of the literature. Int J Surg Case Reports 17: 61-64.
- Cortez N, Berzosa M, Muddasani K, Ben-David K (2020) Endoscopic de-compression of recurrent sigmoid volvulus in pregnancy. J Invest Med High Impact Case Reports 8:1-3.
- Steven RF, Navakanth G, Mitchell CS (2007) Safety of colonoscopy during pregnancy. Am J Gastroenterol 102: S270-S271.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi