Research Article, Int J Cardiovasc Res Vol: 7 Issue: 5
Relation of Diastolic Dysfunction to the LV Twist and Untwist Dynamic: Speckle Tracking Imaging Study
Mahmoud Kamel Ahmed*, Mahmoud Ali Soliman, Morad Beshay Mena, Mohamed Said and Shalaby Montaser
Department of Cardiology, Faculty of Medicine, Menoufia University, Menofia Governorate, Egypt
*Corresponding Author : Mahmoud Kamel Ahmed
Department of Cardiology, Faculty of Medicine, Menoufia University, Menofia Governorate, Egypt
Tel: +01006945404
Fax: 0482333361
E-mail: mahmoudkamel35@gmail.com
Received: August 04, 2018 Accepted: September 20, 2018 Published: September 26, 2018
Citation: Ahmed MK, Soliman MA, Mena MB, Said M, Montaser S (2019) Relation of Diastolic Dysfunction to the LV Twist and Untwist Dynamic: Speckle Tracking Imaging Study. Int J Cardiovasc Res 7:5. doi: 10.4172/2324-8602.1000362
Abstract
Background: There is no single noninvasive index that can directly assess diastolic function. Untwist, contributes to diastolic suction, early filling. Speckle tracking imaging (STI), can be used to study the relation between diastolic indices and untwist in patients with diastolic dysfunction.
Patients and methods: 75 patients with diastolic dysfunction and 25 normal volunteers were selected for this study. According to mitral flow pattern they were classified into Group I (abnormal relaxation), Group II (pseudo-normalized) and group III (stiffness pattern) Using STI, the basal and apical short axis views were imaged. Stored data were processed to get apical and basal rotation, systolic twist, peak systolic twist ratio, diastolic untwist ratio and time to peak twist and untwist ratio.
Results: peak untwisting ratio was significantly higher in Group I Patients that decreased to be normalized and even decreased with progression of diastolic dysfunction from grade II to Group III. There was a highly significant positive and negative correlation with EDV and ESV, respectively. Time to peak untwist ratio non-significantly increased from Group I to III with non significant correlation between untwist ratio and peak E, A, and E/A ratio.
Conclusion: patients with relaxation abnormality have a higher untwist ratio that decrease gradually with progression from relaxation to stiffness pattern. It may appear as a compensatory mechanism to assure early filling with relaxation abnormality.
Keywords: Diastolic dysfunction; Left ventricular twist and untwist; Untwist ratio; Speckle tracking imaging
Introduction
The physiological hallmarks of LV diastolic dysfunction are impaired relaxation, loss of restoring forces, reduced diastolic compliance, and elevated LV filling pressure. Left ventricular diastolic dysfunction in clinical practice is generally diagnosed by imaging and there is no single noninvasive index that provides a direct measure of relaxation, restoring forces, compliance, or LV filling pressure [1]. However, by using a combination of different [2].
In clinical practice to identify and stratify patients with LV diastolic dysfunction, echocardiographic assessment of LV filling using pulsed- Doppler flow velocity of the LV inflow in conjunction with pulmonary venous flow and mitral annulus velocity measurements using Doppler tissue imaging (DTI) have been used [3,4]. However, all these indices are load-dependent, measuring events that occur after mitral valve opening (MVO), thus provide little information on the relaxation process that predominantly occurs prior to MVO, and evaluating only the later stages of LV relaxation [5]. That is why a novel non-invasive method for assessing the earlier stages of LV diastole, (relaxation and restoring forces) need to be developed [6].
Systolic LV twisting and early diastolic LV untwisting are key components of normal ventricular function and appear to play important roles in physiological ventricular adaptation and development of clinically relevant cardio-vascular disease. Untwist, is associated with the release of restoring force and contributes to diastolic suction, which facilitates early LV filling [7].
Considerable additional work is needed to fully define all aspects of LV twist and untwist mechanics and to determine its role in the assessment of normal and diseased heart [7] speckle tracking imaging, a relatively recent modality, enabled rapid assessment of LV twist and untwist mechanics, which have expanded our understanding of both normal ventricular physiology, adaptation, and decompensated function in key disease states
Aim of the Work
Assessment of the relation-ship between indices of early diastolic function and untwist in patients with diastolic dysfunction.
Patients and Methods
We prospectively examined 100 individuals, (75 patients with different grades of diastolic dysfunction with normal ejection fraction (EF) and 25 normal volunteers), selected from Menoufia University Hospital Outpatients Clinics. They were examined by transthoracic echocardiography for evaluation of dyspnea from January of 2016 to January of 2018. We included all patients with diastolic dysfunction with normal EF, in sinus rhythm and normal electrocardiography. We excluded any Patient suffering from, arrhythmia, valvular lesions, history of ischemic heart disease (Electrocardiographic changes and/ or wall motion abnormality) bundle branch block, congenital heart disease, and cardio-myopathy, renal or hepatic disease. Each included patients was subjected to full history taking, thorough clinical examination, 12 lead Electrocardiogram and laboratory investigations (kidney function, liver function, complete blood count, blood sugar, serum uric acid and lipid profile.
Standard echo-cardio-graphic examination
Transthoracic echocardio-graphy was done using a commercially available echo-cardio-graphic machine (E9, GE Medical Systems, Milwaukee, WI) according to the recommendations of the American Society of echocardiography [8]. Conventional Echocardiography measuring: end diastolic dimension and volume (LVIDd, and EDV), end systolic dimension and volume (LVIDs and ESV), fractional shortening (FS), EF, Septal and Posterior wall thickness (L vs. WT and LVPWT) and left ventricular mass index (LVMI). Using pulsed wave Doppler mitral inflow pattern, included patients were classified into 3 groups:
Group I: Including patients with Grade 1, abnormal relaxation pattern, (E/A ratio<0.8, Deceleration Time>240 ms and Iso-volumic relaxation time>90 ms).
Group II: Including patients with Grade II or pseudo-normalized filling pattern (0.8<E/A<1.5, Deceleration Time 140-200 ms, and Isovolumic relaxation time<90 ms)
Group III: Including patients with Grade III or restrictive filling pattern (E/A>1.5, Deceleration time<140 ms and Iso-volumic relaxation time<70 ms). With pulsed wave Doppler tissue imaging the septal mitral annular velocity curve was recorded for all patients and control to measure peak e, a, e/a ratio and E/e.
From the apical 4 chamber view with the electrocardiogram connected to the patient, the time interval between the onset of the QRS on the electrocardiogram to the aortic and mitral valve opening and closure, were measured using pulsed wave Doppler from the LV outflow and inflow, respectively.
Two-D STI echocardiography
Speckle tracking imaging (STI), module was used for assessment of left ventricular rotational mechanics through scanning and recording from left para-sternal short axis view of both basal and apical shortaxis planes to quantify basal and apical LV rotations using the same machine and probe with a probe frequency range 1.7-2.0 MHz at a high frame rate (range 80-115 frame/s). The basal level was marked as the plane showing the tips of mitral valve leaflets at its center with full-thickness myocardium surrounding the mitral valve. Then the transducer was positioned one or two inter-costal spaces more caudal and slightly lateral from the basal site to be perpendicular to the apical imaging plane [9]. The apical level was defined just proximal to the level of LV apical luminal obliteration at the end-systole. The cross-section must be as circular as possible. We have to pay a careful attention to ensure that full thickness of myocardium is imaged throughout the cardiac cycle. Three consecutive cardiac cycles were digitally saved in a cine-loop format for later offline analysis [10]. Offline analyses was done by an independent echo-cardiographer who was not involved in the image acquisition.
Data processing
To analyze twist and untwist parameters, from the basal and apical short axis, data set with a well defined endo-cardial border and the regions of interest were adjusted to include all myocardial thickness without including the pericardium. The endocardial borders of both basal and short axis planes were manually traced and subsequently tracked by the software. If poor tracking quality was observed the region of interest was readjusted until acceptable tracking was obtained otherwise the segment with poor tracking was discarded and replaced by another one. After processing, curves of basal and apical LV rotation, twist, twist rate and untwist rate were automatically generated by the software. (Excel; Microsoft Corporation, Redmond, WA) twist was calculated as apical rotation relative to the basal rotation with counterclockwise rotation as viewed from LV apex expressed as positive value and clockwise rotation as a negative value. Peak LV twist, peak LV twist rate (as first positive peak after R wave on ECG), and peak LV untwist rate (as the first negative peak after aortic valve closure) were recorded. Cardiac cycle length was measured as R-R interval. Time to peak twist rate was measured as time from R wave to peak twist rate and time to peak untwist rate was measured as time from R wave to peak untwist rate.
Statistical analysis
Data were analyzed using SPSS software. Quantitative data expressed as mean and standard deviation Chisquare test student t test, Mann whiney U test, Kruskal Walls test and correlation coefficient test.
Results
This study included 75 patients proved to have diastolic dysfunction by Doppler mitral flow pattern and 25 normal volunteers. 33.3% of patients were males and 66.7% were females with mean age of 50.83 ± 9.27 years compared to 24% were males and 76% were females with a mean age of 49.29 ± 11.77 years of normal controls. With no significant difference between patients and controls as regard to Sex and age (P ≥ 0.05). The prevalence of risk factors (especially hypertension and diabetes) was higher among included patients (P ≤ 0.001). There was non-significant difference as regard to conventional echo-cardio-graphic parameters (LVIDd, LVIDs, EDV, ESV. and EF) except for a highly significantly higher the left atrial diameter between patients and control (Table 1).
| Parameters | The studied groups | Test | P value | |
|---|---|---|---|---|
| Patients N = 75 |
Control N = 25 |
|||
| Age | 50.83 ± 9.27 | 49.92 ± 11.77 | 2.80 | <0.31 |
| Sex Male Female |
25 (33.3) 50 (66.7) |
6 (24.0) 19 (76.0) |
X2 0.76 |
0.38 |
| Risk factors Negative HTN DM HTN&DM |
36 (48.0) 25 (33.3) 6 (8.0) 8 (10.7) |
25 (100) 0 (0.0) 0 (0.0) 0 (0.0 |
X2 21.3 |
<0.001 |
| LVIDd,cm | 4.74 ± 0.49 | 4.84 ± 0.39 | t-test=0.96 | 0.34 |
| LVIDs,cm | 2.99 ± 0.39 | 3.11 ± 0.29 | t-test=1.43 | 0.15 |
| EDV (cm)3 | 104.49 ± 26.02 | 113.52 ± 25.52 | t-test=1.51 | 0.13 |
| ESV (cm)3 | 35.37 ± 11.48 | 39.64 ± 11.62 | t-test=1.61 | 0.11 |
| EF | 0.59 ± 8.31 | 0.60 ± 9.42 | U = 0.58 | 0.56 |
| LA, mm | 38.94 ± 1.52 | 34.36 ± 1.48 | t-test=2.92 | 0.004 |
Table 1: Demographic and conventional Echo-cardio-graphic characters of studied population.
There was a significantly higher apical rotation (11.96 ± 8.5 vs. 8.5 ± 4.62 at P ≤ 0.01), systolic twist (16.02 ± 8.34 vs. 11.07 ± 4.83 At P ≤ 0.01), peak twist ratio (98.74 ± 37.23 vs. 80.87 ± 36.68 at P ≤ 0.03), and peak untwist ratio (-128.05 ± 12.88 vs. -119.94 ± 20.98 at P ≤ 0.01) with non-significantly longer time to peak twist (486.44 ± 166.49 vs. 490.36 ± 71.77 at P ≥ 0.05) time to peak twist ratio (98.74 ± 37.23 vs. 80.87 ± 36.68 at P ≥ 0.05) and time to peak untwist ratio (587.5 ± 162.78 vs. 578.16 ± 93.65 at P ≥ 0.05). There was no difference in basal rotations among patients and controls (-4.59 ± 3.45 vs. -4.56 ± 3.75. at P ≥ 0.05) (Table 2).
| Parameters | The studied groups | U test | P value | |
|---|---|---|---|---|
| patients N = 75 X ± SD |
Control N = 25 X ± SD |
|||
| Apical rotation ,degrees | 11.96 ± 8.5 | 8.51 ± 4.62 | 2.46 | 0.01 |
| Basal rotation ,degrees | -4.59 ± 3.45 | -4.56 ± 3.75 | 0.21 | 0.83 |
| systolic twist ,degrees | 16.02 ± 8.34 | 11.07 ± 4.83 | 2.56 | 0.01 |
| Time to peck twist ,degrees | 486.44 ± 166.49 | 490.36 ± 71.77 | 1.07 | 0.28 |
| Peak twist ratio ,degrees/sec | 98.74 ± 37.23 | 80.87 ± 36.68 | 2.14 | 0.03 |
| Time to peak twist ratio ,ms | 347.88 ± 56.05 | 332.03 ± 155.58 | 1.91 | 0.06 |
| Peak untwist ratio ,degrees/sec | -128.05 ± 12.88 | -119.9 4 ± 20.96 | 3.30 | 0.001 |
| Time to peak untwist ratio ,degrees/sec |
587.5 ± 162.78 | 578.16 ± 93.65 | 0.49 | 0.63 |
Table 2: Left ventricular torsion parameters among Patients and control.
DTI derived curve of the septal aspect of the mitral annulus showed that there was a significant progressive decrease of peak septal e wave from Group I to Group II and III (7.7 ± 0.03, 7.5 ± 0.03 and 4.9 ± 0.005 respectively at P ≤ 0.05), with a significant decrease of peak a wave (12 ± 0.3, 10 ± 0.02 and 11 ± 0.02 respectively at P ≤ 0.02) together with e/a ratio (0.64 ± 0.29 0.76 ± 0.21 and 0.68 ± 4.9 respectively at P ≤ o.01). The E/e as a measure of LV end diastolic pressure showed a highly significant difference between the three groups with progressive increase from Group I to Group II and III (8.17 ± 3.2, 9.28 ± 2.49 and 11.78 ± 1.94 respectively at P ≤ 0.01). As regard to isometric relaxation time there was a non-significant progressive increase from Group I to Group II and III (71.21 ± 12.88, 77.78 ± 19.08 and 81.4 ± 17.43 respectively at P ≥ 0.05) (Table 3).
| Parameters | The studied cases | TEST | P value | ||
|---|---|---|---|---|---|
| Group I X ± SD |
Group II X ± SD |
Group III X ± SD |
K | ||
| e' ,cm/sec | 7.7 ± 0.03 | 7.5 ± 0.03 | .4.9 ± 0.05 | 9.6 | 0.05 |
| a' ,cm/sec | 12 ± 0.03 | 10 ± 0.02 | 11 ± 0.02 | 7.9 | 0.02 |
| e'/a' | 0.64 ± 0.29 | 0.76 ± 0.21 | 0.68 ± 4.90 | 16.9 | <0.01 |
| E/e' | 8.17 ± 3.12 | 9.28 ± 2.49 | 11.78 ± 1.94 | 4.1 | 0.01 |
| IR Time ,ms | 71.21 ± 12.88 | 77.78v19.08 | 81.4 ± 17.43 | 4.54 | 0.10 |
Table 3: Mitral Flow Doppler and Tissue Doppler imaging parameters among patient’s subgroups.
At Group level, Group I and II patients have a significantly higher apical rotation compared to normal control (14.4 ± 6.6 and 11.4 ± 67 at P ≤ 0.001 and P ≤ 0.07 respectively), peak twist (19.1 ± 6.6 and 15.0 ± 78 vs. 11.07 ± 4.83 at P ≤ 0.001 and P ≤ 0.04 respectively), peak twist ratio (106.4 ± 45.2 and 102.4 ± 31.3 vs. 80.87 ± 36.68 at P ≤ 0.04 and P ≤ 0.01 respectively), and peak untwist ratio (-139. ± 16.6 and -123.60 ± 50.8 vs. -119.94 ± 20.96 at P ≤ 0.001 and P ≤ 0.002 respectively). However, there was non-significant difference between patients of Group III and controls regarding apical rotation (8.7 ± 3.4 vs. 8.51 ± 4.62 at P ≥ 0.05) peak twist (13.3 ± 10.1 vs. 11.07 ± 4.83 at P ≥ 0.05), peak twist ratio (65.6 ± 22.6 vs. 80.87 ± 36.63 at P ≥ 0.050), and peak untwist ratio (-92.1 ± 38.2 vs. -119.94 ± 20.96 at P ≥ 0.05). Basal rotation in Group III was significantly lower (-1.8 ± 2.4 vs. -4.56 ± 3.75 at P ≤ 0.02). For time to peak twist (542.4 ± 24.03, 529.7 ± 23.11, 450 ± 8.3 vs. 490.236 ± 71.77 at P ≥ 0.05) peak twist ratio (316.6 ± 114.8, 318 ± 121.8, 364.3 ± 117.1 vs. 347.88 ± 56.05 At P ≥ 0.05) and time to peak untwist ratio (556.8 ± 120.7, 554.6 ± 133.3, 628.6 ± 125.7 vs. 587.16 ± 93.65 At P ≥ 0.05). There was a non-significant increase in time with increasing severity of diastolic dysfunction (Table 4).
| Parameters | The studied cases | Control N = 25 | K | P value | Post hoc test | ||
|---|---|---|---|---|---|---|---|
| Group 1 N = 42 |
Group 2 N = 23 |
Group 3 N = 10 |
|||||
| X ± SD | X ± SD | X ± SD | X ± SD | ||||
| Twist ,degrees | 19.1 ± 7.9 | 15.0 ± 7.8 | 13.3 ± 10.1 | 11.07 ± 4.83 | 13.04 | 0.005 | 0.0011 0.042 0.983 |
| Apical rotation ,degrees | 14.4 ± 6.6 | 11.4 ± 6.7 | 8.7 ± 3.4 | 8.51 ± 4.62 | 12.28 | 0.006 | 0.0011 0.072 0.663 |
| Basal rotation ,degrees | -5.8 ± 4.3 | -4.6 ± 2.8 | -1.8 ± 2.4 | -4.56 ± 3.75 | 8.79 | 0.03 | 0.331 0.572 0.023 |
| Time to peak twist , ms | 542.4 ± 240.3 | 529.7 ± 231.1 | 450.0 ± 82.3 | 490.36 ± 71.77 | 5.24 | 0.16 | 0.611 0.872 0.073 |
| Peak twist ratio ,degrees/sec | 106.4 ± 45.2 | 102.4 ± 31.3 | 65.6 ± 22.6 | 80.87 ± 36.68 | 14.39 | 0.002 | 0.041 0.012 0.363 |
| Time to peak twist ratio ,ms | 316.6 ± 114.8 | 318.0 ± 121.1 | 364.3 ± 117.1 | 347.88 ± 56.05 | 0.82 | 0.66 | 0.161 0.042 0.873 |
| Peak untwist ratio ,degrees/sec | -139.0 ± 166.8 | -123.6 ± 50.8 | -92.1 ± 38.2 | -119.94 ± 109.6 | 2.90 | 0.23 | 0.0011 0.0022 0.413 |
| Time to peak untwist ratio ms | 556.8 ± 120.7 | 554.6 ± 133.3 | 628.6 ± 125.7 | 587.16 ± 93.65 | 0.90 | 0.64 | 0.451 0.822 0.813 |
Table 4: Speckle tracking imaging mode among cases subgroups and control.
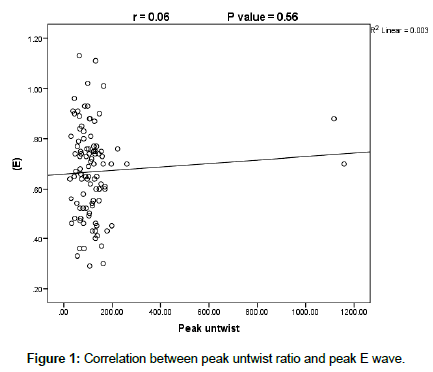
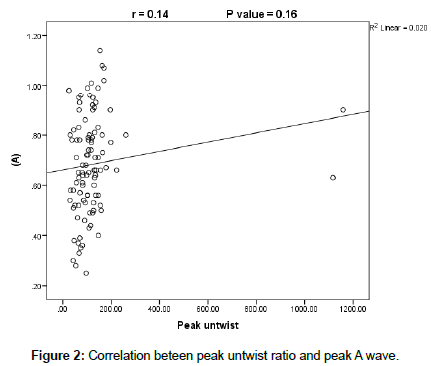
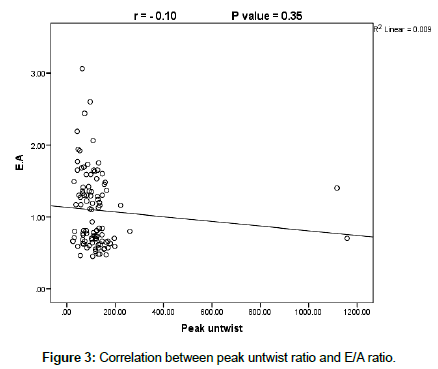
On doing correlation between peak untwist ratio and conventional echocardiographic parameters there was a significant positive correlation between both end diastolic diameter and volume (r=023 at P ≤ 0.02 and r=0.22 at P ≤ 0.03 respectively), with statistically significant negative correlation with both end-systolic diameter and volume (r=0.22 at P ≤ 0.03) with non-significant correlation with the other parameters ((EF, SV, FS, and LA diameter (r=0.18, 0.06, 0.02, and 0.002 at P ≥ 0.05). However, there was a weak and non significant correlation between untwist ratio and Doppler mitral flow indices (E, A and E/A) (r=0.06, 0.14 and 0.10 respectively at P ≥ 0.05) (Figures 1-3). The same finding were recorded as regard to correlation between mitral annulus DTI derived diastolic indices (e, a, e/a, E/e and isometric relaxation time (IRT), (r=0.002, 0.050. 004, 0.01 and 0.16 respectively at P ≥ 0.05) (Table 5).
| Peak untwist | Time to peak untwist | Peak untwist | Time to peak untwist | ||||||
|---|---|---|---|---|---|---|---|---|---|
| R | P value | R | P value | R | P value | R | P value | ||
| LVIDd | -0.23 | 0.02 | 0.22 | 0.03 | E | 0.06 | 0.56 | 0.15 | 0.15 |
| LVIDs | -0.22 | 0.03 | -0.02 | 0.84 | A | 0.14 | 0.16 | -0.08 | 0.42 |
| EDV | -0.22 | 0.03 | 0.20 | 0.05 | E/A | -0.10 | 0.35 | 0.15 | 0.14 |
| ESV | -0.22 | 0.03 | -0.03 | 0.76 | e' | 0.002 | 0.99 | 0.05 | 0.65 |
| EF | 0.18 | 0.14 | -0.15 | 0.13 | a' | -0.05 | 0.62 | -0.04 | 0.69 |
| SV | -0.06 | 0.58 | 0.14 | 0.17 | e'/a' | -0.004 | 0.97 | -0.13 | 0.21 |
| FS | -0.02 | 0.82 | -0.02 | 0.84 | E/e' | -0.01 | 0.92 | 0.02 | 0.77 |
| LA | -0.002 | 0.98 | 0.16 | 0.12 | IRT | -0.16 | 0.12 | -0.07 | 0.49 |
Table 5: Correlation between untwist parameters with conventional echo, mitral inflow and mitral annulus TDI parameters.
Discussion
This study based on STE assessment of left ventricular untwist in patients proved to have diastolic dysfunction by trans-mitral Doppler flow indices to assess the relation between left ventricular untwist and indices of diastolic dysfunction. The major findings of this study were first: Significantly higher apical rotation, peak twist, peak twist ratio and peak untwist ratio when all patients compared to control. Second: A significantly higher apical rotation, peak twist, peak twist ratio and untwist ratio among Group I (impaired relaxation), then these values decreased gradually from group I to group II and III to be normalized or even decreased in Group III. Third: Time to peak twist, twist ratio and untwist ratio showed a progressive non significant increase. Fourth: There was a significantly positive correlation between peak untwist ratio with LVIDd and EDV with a significantly negative correlation with LVIDs and ESV, Fifth: There was no association or correlation between untwist ratio and peak E, A, and E/A ratio.
Several studies of patients with diastolic dysfunction or heart failure with preserved ejection fraction demonstrated that patients earlier stages of diastolic dysfunction has a higher untwist and untwist ratio that becomes normalized or decreased with higher grades of diastolic dysfunction and this findings was not applicable to patients with systolic heart failure [11-13].
These findings can be explained as follow. Twisting and untwisting of the left ventricle are important aspects of the cardiac mechanics and function. In a normal heart, the onset of myofiber shortening occurs earlier in the endocardium than the epicardium [14]. During pre-election, subendocardial shortening and subepicardial stretch contribute to a brief clockwise rotation of the LV apex and counterclockwise rotation of the base [14,15]. During ejection, the activation and contraction of the sub-epicardial layer with larger radius of arm of momentum produces higher torque to dominate the direction of rotation, resulting in counterclockwise of the apex and clockwise rotation the base leading to ventricular twisting. Twisting and shearing of the sub-endocardial fibers deform the matrix and result in storage of potential energy in the deformed intracellular giant protein titin filaments and in the extracellular collagen fibers to be converted into kinetic energy (restoring force) with the start of relaxation leading to recoil and untwist in early diastole [16]. In the majority of patients with diastolic dysfunction the subendocardial layer suffers first and becomes affected earlier leading to a decrease in its counterbalancing effect and the subepicardial domination of rotation becomes more prominent with increased both twist and untwist. With disease progression the sub-epicardial layer becomes affected leading to decrease of its domination with progressive decrease of both twist and untwist [17].
Wang et al. [13] reported that the left ventricular end systolic volume is an important determinant of untwisting rate in patients with diastolic dysfunction irrespective of left ventricular ejection fraction which is in agreement with the finding of this study. Dong et al. [18] reported that higher left ventricular end-diastolic volumes produced higher twist and untwists when end systolic volumes were held constant and higher left ventricular end-systolic volume produced lower twist and untwists when end diastolic volumes were held constant. These findings explain the positive correlation between end-diastolic volume and negative correlation between end-systolic volume with ventricular untwist reported in this study.
The absence of correlation between untwist ratio and both mitral inflow and Doppler tissue derived diastolic parameters can be explained as follow, first: all these indices are load-dependent, measuring events that occur after mitral valve opening (MVO), thus provide little information on the relaxation process that predominantly occurs prior to MVO and evaluating only the later stages of LV relaxation [5] However, untwisting starts in late systole before aortic valve closure and nearly 50% to 70% of LV untwisting occurs within the period of isovolumic relaxation before mitral valve opening, while the rest is completed during early diastolic filling phase [7] leading to time disassociation between the two events. Second: relaxation and stiffness are the major determinant of mitral flow pattern but relaxation is not the sole determinant of untwist where untwist is controlled mainly by the interaction between relaxation and restoring forces and finally, untwist ends in early diastole and before the effect of stiffness. Left ventricular untwisting rate has been associated with early diastolic load and restoring forces but not LV stiffness [19,20]. It becomes clear that the factors controlling mitral flow pattern are not the same that control untwist ratio in addition to different timing of both events. These facts can explain the lack of correlation between both parameters.
As regard to time to peak twist and twist ratios, contractility is a major determinant of twist and it was proved that patients with diastolic dysfunction have subclinical affection of myocardial contractility despite normal EF [21]. This impaired contractility may be the underlying cause of prolongation of time to peak twist and twist ratio. As regard to time to peak untwist ratio the prolongation can be explained as follow First: impaired relaxation tend to prolong time to peak untwist ratio second: increased restoring force in patient with impaired relaxation secondary to dominant subepicardial and weakend counter balancing effect of suendocardial layer in those patients tends to accelerate untwist and shorten the time to peak untwist ratio. The increased restoring force will ameliorate the effect of impaired relaxation and lead to a non significant prolongation of the time to peak untwist ratio [17,21]. With disease progression contractility decreases leading to decrease of restoring force and relaxation becomes more impaired and tend to decrease rate of untwist and prolongation of time to peak untwist ratio that is why time prolongation increases with increasing severity of diastolic dysfunction. However, the smaller number in Group III (10 patients) was a limiting factor to explore its effect on time to peak untwist ratio.
Conclusion
Untwist may add a new dimension to the noninvasive assessment of diastolic dysfunction. It actually reflects the mechanical aspect of global diastolic function especially the early phase of diastole responsible for creation of suction to assure efficient early filling. Twist and untwist are a strong bridge between systole and diastole.
Study Limitations
The sample size especially Group III was smaller (10 patients). Heterogeneity of the underlying cause of diastolic dysfunction. Inspite of paying greater attention to locate the exact apical and basal planes variability may occur between patients and this may affect values of rotations from patient to patient. Apical; and basal plane imaging does not occur in the same cardiac cycle. Lastly out of plane motions especially at basal plane may be a problem. Thus 3D STE may solve some of these limitations.
Acknowledgement
I would like to thank professor said shalaby professor of cardiology, cardiology department faculty of medicine Menoufia University, for his great help and continuous education and unlimited effort.
References
- Flachskampf FA, Biering-Sørensen T, Solomon SD, Duvernoy O, Bjerner T, et al. (2015) Cardiac Imaging to Evaluate left Ventricular Diastolic Function. JACC: Cardiovascular Imaging. 8: 1071-1093.
- Smiseth OA (2018) Evaluation of left ventricular diastolic function: state of the art after 35 years with Doppler assessment. J Echocardiography 16: 55-64.
- Maurer MS, Spevack D, Burkhoff D, Ronzon KI (2004) Diastolic dysfunction: can it be diagnosed by Doppler echocardiography?J Am Coll Cardiol 44: 1543-1549.
- Oh JK, Hatle L, Tajik AJ, Little WC (2006) Diastolic heart failure can be diagnosed by comprehensive two-dimensional and Doppler echocardiography. J Am Coll Cardiol 47: 500-506.
- Dong S, Hees P, Siu C, Weiss J, Shapiro E (2001) MRI assessment of LV relaxation by untwisting rate: a new isovolumic phase measure of tau. Am J Physiol Heart Circ Physiol 281 : H2002-H2009.
- Takeuchi M, Borden WB, Nakai H, Nishikage T, Kokumai M, et al. (2007) Reduced and delayed untwisting of the left ventricle in patients with hypertension and left ventricular hypertrophy: a study using two-dimensional speckle tracking imaging. Eur Heart J 28: 2756-2762.
- Stöhr EJ, Shave RE, Baggish AL, Weiner RB (2016) Left ventricular twist mechanics in the context of normal physiology and cardiovascular disease: a review of studies using speckletracking echocardiography. am J Physiol Heart Circ Physiol 311: H633-H644.
- Mor-Avi V, Lang RM, Badano LP, Belohlavek M, Cardim NM, et al. (2011) Current and evolving echocardiographic techniques for the quantitative evaluation of cardiac mechanics: ASE/EAE consensus statement on methodology and indications endorsed by the Japanese Society of Echocardiography. J Am Soc Echocardiogr 24: 277-313
- Hollekim-Strand SM, Hoydahl SF, Follestad T, Dalen H, Bjørgaas MR, et al. (2016) Exercise training normalizes timing of left ventricular untwist rate , but not peak untwist rate, in individuals with type 2 diabetes and diastolic dysfunction: a pilot study JASE 29: 421-430
- Maufaris C, Schuster I, Doucende G, Vitiello D, Rupp T, et al. (2014) Endurance training minimizes Age-related changes of left ventricular twist-untwist mechanics. JASE 27: 128-1215.
- Park SJ, Miyazaki C, Bruce CJ, Ommen S, Miller FA, et al. (2008) Left ventricular torsion by two-dimensional speckle tracking echocardiography in patients with diastolic dysfunction and normal ejection fraction. J Am Soc Echocardiogr 21: 1129-1137.
- Wang J, Khoury DS, Yue Y, Torre-Amione G, Nagueh SF (2007) Left ventricular untwisting rate by speckle tracking echocardiography. Circulation 116: 2580-2586.
- Wang J, Khoury DS, Yue Y, Torre-Amione G, Nagueh SF (2008) Preserved left ventricular twist and circumferential deformation, but depressed longitudinal and radial deformation in patients with diastolic heart failure. Eur Heart J 29: 1283-1289.
- Ashikaga H, van der Spoel TI, Coppola BA, Omens JH (2009) Transmural myocardial mechanics during isovolumic contraction. JACC Cardiovasc Imaging 2: 202-211.
- Sengupta PP, Tajik AJ, Chandrasekaran K, Khandheria BK (2008) Twist mechanics of the left ventricle: principles and application. JACC Cardiovasc Imaging 1: 366-376.
- Fukuda N, Terui T, Ishiwata S, Kurihara S (2010) Titin-based regulation of diastolic and systolic functions of mammalian cardiac muscle .J Mol Cell Cardiol 48: 876-881.
- Nakatani S (2011) left ventricular rotation and twist : why should we learn? J Cardiovasc Ultrasound 9: 1-6.
- Dong SJ, Hees PS, Siu CO, Weiss JL, Shapiro EP (2001) MRI assessment of LV relaxation by untwisting rate: anew isovolumic phase measure of Ԏ. Am J Physiol Heat Circ Physiol 281: H2002-2009.
- Burns AT, La Gerche A, MacIsaac AI, Prior DL (2008) Augmentation of left ventricular torsion with exercise is attenuated with age. J Am Soc Echocardiogr 21: 315-320.
- Opdahl A, Remme EW, Helle-Valle T, Edvardsen T, Smiseth OA (2012) Myocardial relaxation, restoring forces, and early-diastolic load are independent determinants of left ventricular untwisting rate. Circulation 126: 1441-1451.
- Humg CL, Hou CL, Hu GC (2013) Myths and facts about heart failure with preserved Ejection Fraction : Risk factors, longevity, potential pharmacological and exercise interventions. Int J Gerontol 7: 1-7.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi