Case Report, Int J Cardiovasc Res Vol: 9 Issue: 8
Ruptured Carotid Artery Aneurysm: A Case Study and Nurse led Interventions
Devanshi Chowdhary and Renuka Kadian*
Nursing Officer, All India Institute of Medical Sciences, New Delhi, India
*Corresponding Author: Renuka Kadian
BSc. Nursing (PGIMS, Rohtak), MSc. Nursing – Child Health Nursing (PGIMER, Chandigarh), Nursing Officer, All India Institute of Medical Sciences, New Delhi, India
E-mail: renukadian2930@gmail.com
Received: November 04, 2020 Accepted: December 04, 2020 Published: December 11, 2020
Citation: Chowdhary D, Kadian R (2020) Ruptured Carotid Artery Aneurysm: A Case Study and Nurse led Interventions. Int J Cardiovasc Res 9:8.. doi: 10.37532/icrj.2020.9(8).428
Abstract
Carotid artery aneurysm is defined as a bulge or weakened area of carotid artery which allows part of blood vessel to protrude out posing a risk for rupture. External carotid artery aneurysm is a bulge in the wall of carotid arteries on either side of the neck. The following case presents a case of a middle aged women presenting with carotid artery aneurysm and planned for emergency surgery, awaiting which the patient suffered rupture of carotid artery aneurysm, and underwent debranching of the innominate artery and reconstruction of Right Common carotid artery and supraclavicular artery, the skin defect formed due to the rupture of carotid artery aneurysm was corrected by pectoralis major myocutaneus flap cover. The care of the patient across the time of stay in critical care had various nursing challenges which were handled diligently rendering to the effective management of the patient.
Keywords: Carotid artery aneurysm; Carotid artery rupture; Surgical flap; Nursing interventions
Case report
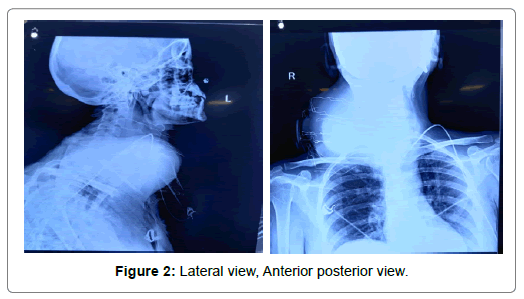
A 45 years old woman, presented in emergency department, All India Institute of Medical Sciences on 26/6/20 with sudden increase in size of a small preexisting lump on the right side of neck, on examination was found to have a large nodular cystic mass over the right supraclavicular area, with facial swelling and hoarseness of voice, and tingling in the right arm and forearm. The patient had tachycardia with all other vital parameters under normal range, patient was triaged in yellow zone, and an emergency computed tomography scan was done which revealed a large pseudoaneurysm (9* 8*7) communicating with Right common carotid artery, with active contrast extravasation and enlarged cervical and superior mediastinal lymph nodes. Mycotic aneurysm was also suspected as the patient had a history of untreated pott’s spine (Figures 1 and 2).
The patient was shifted to an intensive cardiac care unit on the same day and was kept under continuous observation, with hourly vitals, cardiac monitoring, and intake output measurements. Clinical history revealed that patient was a non- smoker with no history of any cardiovascular disease, there was no history of trauma or previous head and neck surgery, patient had untreated pott’s spine with incomplete ATT treatment. Clinical examination of the neck mass revealed a 15* 12 irregular mass on the right side extending 2 cm below the angle of mandible to right supraclavicular fossa. Ultrasonography of the neck showed a large aneurysmal sac (6*12 cm), 2.5 mm involving whole of neck with low turbulent low resistance forward flow was seen within sac, aneurysm was arising from the Right CCA. Baseline blood chemistry tests were done which showed signs of infection with decreasing hemoglobin, RBC count, MCHC, MCH (5.8gm/dl, 2.34*106, 29.3, 23.9), deranged Liver function test (Alkaline Phosphatase 321IU/L, SGPT 401U/L) and renal function test (increased creatinine to 2.3 mg/dl, phosphate 4.7mg/dl globulin 3.7 mg/dl), thyroid profile T3(130 ng/dl), T4(8 μg/dL) and Thyroid stimulating hormone (3 mIU/ml).
The patient received 3 units of PRBC preoperatively due to falling Hb levels. In view of the extensive surgical procedure, which was planned after multidisciplinary workup including Cardiac radiology, cardiac surgery, neurology, nephrology, pulmonology, ENT was done, and surgical clearance was taken from all of these departments. Stenting of the CCA was kept as an option only when it was immediately followed by surgical procedure of evacuation of hematoma. The patient was planned for surgery on subsequent day.
On 29/6/20 while awaiting for consent of the patient for the surgical procedure, the patient suddenly developed severe pain on right side of the neck with tachycardia, distressed breathing, fall in blood pressure, increase in the size of mass, and subsequent rupture of the carotid aneurysm. The patient was immediately rushed to the operation theatre.
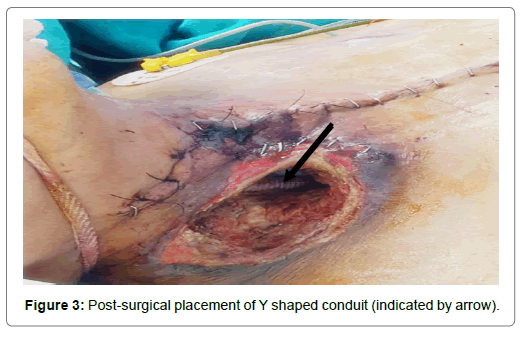
The patient underwent emergency debranching of the innominate artery with Y shaped conduit vascular prosthesis (16*8mm, 45 cm) and reconstruction of Right CCA and supraclavian artery on 29/6/20 under deep hypothermic cardiac arrest at 24° Celsius. Due to the sudden rupture of the carotid aneurysm the patient developed a 5*5 skin defect post operatively. The area was packed with sterile gauze and dressing was done regularly at frequent intervals. The patient was on high ionotropic support with noradrenaline at the rate of 0.6 μg/ kg/min, dopamine at a rate of 5 μg/kg/min and adrenaline at the rate of 0.5 μg/kg/min (Figures 3 and 4).
The skin defect was planned to be covered by a skin graft by the plastic surgery department. NCCT brain was done on the same day to check for any circulation deficits due to the prolonged surgery which showed minimal areas of decreased blood circulation. The patient was kept under strict observation in the cardiac intensive care ICU with high inotropic support, which was being tapered constantly, On 5th post op day, patient was extubated, it was observed that there was bilateral upper limb weakness (Left>>right) power off the limbs was as follows:
• B/L lower limbs: >>4/5.
• Right upper limb: 0/5 at shoulder and above, and 2/5 at the wrist level.
• Left upper Limb: 0/5 at all points.
• Deep tendon reflex – negative in both the upper limbs, +1 in both lower limbs
NCCT head was done again, which revealed diffuse cerebral edema, and sulcal effacement, a posterior watershed ischemia possible due to prolonged hypoperfusion in the brain and sulcal ischemia, postoperative plexopathy was also diagnosed. Continuous regular physiotherapy was prescribed and was followed thereafter.
After the tapering of inotropic support to minimal(noradrenaline at the rate of 0.1 μg/kg/min, and adrenaline at the rate of 0.2 μg/kg/ min) the patient was considered for flap reconstruction of the skin defect at the operative site, decided for PMMC flap (Pectoralis major myocutaneous flap) repair of the operative area on 5/7/20.
The patient thereafter was on wide spectrum antibiotic support:
• Inj. Zosyn 4.5 grams IV TDS
• Inj. Targocid 400 micrograms IV OD
• Inj Pantop micrograms 40 IV OD
• Inj PCM. 1gram I.V TDS
• NS 50ml/hr
• Blood and blood products as required
The patient was shifted from the ICU to ward on 30/7/20, off inotropic support and with vitals stable regular physiotherapy, continuous cardiac monitoring and flap dressing with normal saline were advised.
The patient was discharged from the ward on 15/8/20, on oral antibiotics and regular physiotherapy exercises, and a continuous follow up every month.
Though the patient’s neurological deficit had not resolved completely, the patient had showed significant improvement in the muscle power with continuous physiotherapy. At discharge the muscle power of the patient was as shown in Table 1.
| AFTER THE SURGICAL INTERVENTION FOR ANEURYSM | AT DISCHARGE FROM HOSPITAL |
|---|---|
| B/L lower limbs: >>4/5. | B/L lower limbs: >>4/5. |
| Right upper limb: 0/5 at shoulder and above, and 2/5 at the wrist level. | Right upper limb: 2/5 at shoulder and above, and 4/5 at the wrist level. |
| Left upper Limb: 0/5 at all points. | Left upper Limb: 2/5 at shoulder and above, 3/5 at the wrist level. |
| Deep tendon reflex – negative in both the upper limbs, +1 in both lower limbs | Deep tendon reflex –, +2 in both lower limbs, +1 in both upper limbs |
Table 1: The muscle power of the patient at the time of discharge.
Disease Condition
Introduction
Carotid artery aneurysm is defined as a bulge or weakened area of carotid artery which allows part of blood vessel to protrude out posing a risk for rupture. It is localized blood-filled abnormal dilation of an artery. Aneurysms may lead to stroke and severe bleeding. Intracranial carotid artery aneurysm is when one develops inside the skull involving the vessels supplying the brain. External carotid artery aneurysm is a bulge in the wall of carotid arteries on either side of the neck. The types pf aneurysm is Saccular (A bulbous out-pouching of one side of the artery resulting in localized stretching of artery wall) and Fusiform (A uniformly shaped dilation involving entire circumference of artery). The risk factors are: men are at greater risk than women, Age, Smoking, Connective tissue disorders, Family history of aneurysms, Atherosclerosis and High blood pressure.
Incidence
Carotid artery aneurysms are rare. Most common reported site of extracranial carotid system is the bifurcation of common carotid artery [1]. Aneurysms in total are most commonly reported in abdominal aorta. Thoracic aneurysms account for about 25% of all cases [2]. Reported incidence of Extracranial Carotid Artery (ECCA) aneurysms is about 0.2% to 5% of all carotid artery surgeries [3].
Clinical manifestation
It is not necessary to present symptoms every time with extracranial carotid artery aneurysms. It depends mostly on the site and size of aneurysms. It can cause Difficulty in swallowing, Facial swelling, hoarseness in voice
In cases of ruptured aneurysms, it can even lead to stroke or TIA (transient ischemic attack) resulting in mini stroke that temporarily stops blood from reaching your brain [4,5].
Workup
A physical exam and asking about any symptoms are necessary steps in diagnostic evaluation of extracranial carotid artery aneurysm. Other diagnostic tests are,
1. Angiography
2. CT scan (computed tomography)
3. Echocardiography (ultrasound testing)
4. MRI (magnetic resonance imaging).
Surgical Management
The goals of treatment are to reduce symptoms and reduce the risk of complications. Medications are also used to lower the blood pressure and cholesterol levels or to dissolve clots so that rupture or unnecessary complications can be prevented. The treatment options are surgical repair and Endovascular stent grafting.
1. Surgical Repair: Surgery is the mainstay for treating extracranial carotid artery aneurysms. It is resecting the portion of involved carotid artery. Then bypass is created between two normal artery ends above and below the aneurysm with the help of variety of conduits. It may include vein from the leg, artery from any other part of body or a prosthetic graft usually made up of gortex or polyester.
2. Endovascular Stent Grafting: The procedure depends on size of aneurysm and location involving the other branches of carotid artery. This is a form of catheterization performed inside the artery using femoral access. Catheters are used to guide and deliver a stentgraft through arteries up to the site of aneurysm. Artificial graft is then positioned in the area of aneurysm under X-Ray or ultrasound guidance and expanded inside the target artery. Site is fixed with metallic staples instead of sutures.
Prognosis
More cases have been documented with open aneurysm repair and outcomes are somewhat similar to carotid endarterectomy. Less than 4% of surgeries are associated with most concerning risk of peri-operative stroke. Damage to nerves and adjacent structures is another risk. Stent-graft repair like carotid artery stenting and carotid endarterectomy has emerging success rates.
Nursing Management
A planned nursing care is required to manage a patient with external carotid artery aneurysm. Following nursing diagnosis were formulated by prioritizing the needs of the patient.
Assessment
Increased demands, Request to have family members at bedside all the time, tense, anxious appearance.
Nursing Diagnosis: Anxiety related to sudden onset of illness, impending surgery and multiple tests and procedures evidenced by increased alertness, restlessness and increased questioning.
Nursing Interventions:
a) Assess the level of anxiety (mild to severe) of patient.
b) Note the non-verbal clues associated with acute lifethreatening situation.
c) Acknowledge patient’s feelings and accept the anxiety which confirms validation.
d) Ensuring the environment and surroundings are quiet, noise free.
e) Minimize external stimuli like unnecessary conversations, and medical equipment which aggravates anxiety.
f) All the procedure related information should be conveyed in more simple, clear and brief instructions. Use of appropriate, concrete words helps reducing anxiety.
Evaluation: Patient exhibits positive coping strategies and verbalizes fears.
Assessment
Repeated questioning, Restlessness
Nursing Diagnosis: Deficient knowledge related to diseased condition and unfamiliarity with hospital care and surgical outcome evidenced by repeated questioning and expressed need of information.
Nursing Interventions:
a) Assess the current existing knowledge of the patient regarding the disease and treatment options.
b) Clear and concise instructions should be given about:
• Possible sign and symptoms such as pain in chest, decreased urine output, cool extremities.
• Use of antihypertensive medication, its side effects and monitoring BP levels.
• Importance of follow up and compliance to treatment regime.
c) Activity restrictions like heavy lifting, straining for bowel movements to reduce strain on suture lines and promote wound healing. (at least for 4-6 weeks).
d) Isometric activities which can abruptly elevate the BP levels should be avoided.
e) Follow up is needed to evaluate the wound at 1 and 6 months and yearly check-ups are necessary. Follow up CT scans are needed to assess endograft leak.
Evaluation: Patient verbalizes understanding of disease process, treatment options and set goals.
Assessment
Tachycardia, decreased urinary output, restlessness.
Nursing Diagnosis: Decreased cardiac output related to rupture of aneurysm, surgical intervention and side effects of medications.
Nursing Interventions:
a) Note the signs of MI such as tachycardia, chest pain and ECG changes.
b) Monitor signs of reduced cardiac output and hemodynamic instability as it suggests rupturing aneurysm.
c) Maintain efficient circulation by diagnosing severe aortic inefficiency or ruptured aorta.
d) Administration of IV Fluids, blood products and medication.
e) Provide emotional support to patient by staying with the client.
f) Prepare the patient about the surgical procedure or other diagnostic procedures in simple, concise words.
g) Fluid management: administration of isotonic fluids and plasma expanders in case of reduced cardiac output.
Evaluation: Cardiac output of the patient is adequate evidenced by normal BP levels, urine output more than 30 ml/hr, Hr b/w 60-100 bpm and clear lung sounds.
Nursing Diagnosis
Ineffective tissue perfusion related to increased BP, risk of dissection, defect in vessel wall, trauma or other unknown causes.
Nursing Interventions:
a. Note the characteristics and location of pain. Pain in neck, shoulders and lower back suggests thoracic involvement. Use of non-pharmacological measures for pain relief such as relaxation techniques, position of comfort, cold and hot physical touch.
b. Complete physical history suggests risk for aneurysm rupture. Poorly managed hypertension aggravates the risk.
c. Monitoring progression of aortic dissection by changes in level of consciousness and weakened carotid pulses. It is also determined by decreased urine output, abdominal pain, altered motor and sensory function etc.
d. Assess upper and lower extremities for signs of peripheral ischemia and insufficiency. (paralysis, weakness, weak pulse, cool extremities).
e. Assess the quality of peripheral pulse to ensure distal perfusion.
f. Assess the respiratory compromise because of compression of trachea or adjacent structures. Hemoptysis can also be presented. Patient can also present dysphagia by compression of esophagus.
g. Anticipate further diagnostic tests (chest X-Ray, USG, CT, MRI scan) and plan follow up.
h. Assess for swelling in upper extremities or head due to obstruction of subclavian artery.
i. Administration of anti-hypertensive medications as ordered. (beta blockers, ACE inhibitors).
Evaluation: Patient exhibit strong palpable pulses, warm extremities, normal urine output, alert, normal bowel sounds and absence of chest/abdominal pain which suggests adequate tissue perfusion.
Conclusion
Nurses play an important role in managing conditions that affect the complex cardiovascular system. They work to promote preventive measures like early diagnosis and disease prevention. They also provide comprehensive nursing care to patients including pre, intra and post operative care in tertiary care hospitals
References
- Pinjala RK (2010). Ruptured large carotid artery aneurysm. Indian journal of surgery. 72:321–322.
- Pourier V, van Laarhoven CJ, Vergouwen M, Rinkel G, de Borst G, et al. (2019) Prevalence of extracranial carotid artery aneurysms in patients with an intracranial aneurysm. European Journal of vascular and Endovascular surgery, 58:91.
- Painter TA, Hertzer NR, Beven EG, O’Hara PJ. (1985) Extracranial carotid aneurysms: report of six cases and review of the literature. J Vasc Surg. 2:312-318.
- Liapis CD, Gugulakis A, Misiakos E, Verikokos C, Dousaitou B, et al. (1994) Surgical treatment of extracranial carotid aneurysms. Int Angiol. 13:290-295.
- Pulli R, Gatti M, Credi G, Narcetti S, Capaccioli L, et al. (1997) Extracranial carotid artery aneurysms. J Cardiovasc Surg (Torino). 38:339-346.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi