Research Article, Int J Cardiovasc Res Vol: 7 Issue: 3
The Impact of Height on Clinical Management of Hypertension in Primary Care
Hatouf H Sukkarieh1*, Rami T Bustami2, Nadia El Amin1 and Hadeel Al-khaneen1
1College of Medicine, King Saud bin Abdulaziz University for health Sciences, Riyadh, Saudi Arabia
2College of Pharmacy, King Saud bin Abdulaziz University for health Sciences, Riyadh, Saudi Arabia
*Corresponding Author : Hatouf H Sukkarieh
College of Medicine, Female Branch, King Saud Bin Abdul-Aziz University for Health Sciences (KSAU-HS), Mail code 3155, Riyadh, PO BOX 11481, Saudi Arabia
Tel: +966 11-42-99772
E-mail: sukkariehh@ksau-hs.edu.sa
Received: March 23, 2018 Accepted: May 10, 2018 Published: May 16, 2018
Citation: Sukkarieh HH, Bustami RT, Amin NE, Al-khaneen H (2018) The Impact of Height on Clinical Management of Hypertension in Primary Care. Int J Cardiovasc Res 7:3. doi: 10.4172/2324-8602.1000349
Abstract
Study demonstrated that hypertension was significantly more controlled with increased height. Also, beta-blockers appeared to be effective for controlling BP in hypertensive patients. High blood pressure is one of the major well-being issues in most developed and developing countries. It is considered a major risk factor for cardiovascular and kidney diseases globally. Worldwide, about one billion individuals were found to have high blood pressure and 13% of all fatalities were carefully related to hypertension.
Keywords: Hypertension; Clinical management; Primary care; Elevated blood pressure
Introduction
Having high blood pressure is one of the major well-being issues in most developed and developing countries. It is considered a major risk factor for cardiovascular and kidney diseases globally. Worldwide, about one billion individuals were found to have high blood pressure and 13% of all fatalities were carefully related to hypertension. Epidemiological studies have established risk factors for hypertension, including obesity, high salt intake; alcohol drinking, cigarette smoking, and sedentary lifestyles, but other factors remain unexplored [1]. It has been found that hypertension is carefully associated with body weight and size in US children. There is a high chance that having hypertension at an early age can develop into hypertension in adulthood [2].
Some evidence reveals an inverse relationship between height and risk of diabetes, cardiac arrest, and death rate [3]. Despite having a large number of publications regarding adult height, there seems to be little integration of the epidemiological and the population health perspectives on modern adult height. The Epidemiological research revealed that height was inversely associated with heart diseases. Contradictory results were reported in regards to an association between height and having high blood pressure. while other studies reported a significant positive relationship between height and elevated BP levels [4]. These studies demonstrated that stature was associated with lower systolic blood pressure (SBP) and pulse pressure (PP) but not with diastolic blood pressure (DBP). It has been additionally observed that stature was related to a reduced occurrence of hypertension in the elderly, independent of antihypertensive medicines. Also, gender had a contributing effect; a study from Brazil reported that hypertension was significantly more prevalent of hypertension after adjustment for age, pay, smoking, sodium and alcohol intake and race. Systolic blood pressure showed a U-shaped association with stature, mainly among women [2,4-7].
The mechanism underlying the association between height and hypertension is unclear. A connection to the dynamic properties of the arterial tree has been reported. That is, individuals of short stature may have shorter arterial tree, which will likely make the reflected waves arrive earlier in the central aorta and augment central pressure and pulse pressure in late systole. Shorter stature in the elderly, low BMD and fractures are associated with increased arterial stiffness and hypertension [2,5,6]. Another possible explanation could be nutrition in childhood, where evidence across studies indicates that short adult height in low and middle-income countries is driven by environmental conditions, particularly net nutrition during early years. Height is not only an important marker of malnutrition in childhood, but also a marker of mother’s nutrition during pregnancy [2,5-7].
Most of the above listed studies were conducted in western countries, and were based on exploring the association between height and hypertension. However, evidence on the relatioship hypertension and height in adult patients is lacking. The aim of this study was to explore the association between height and control of blood pressure in middle-aged and elderly hypertensive adult patients.
Data and Methods
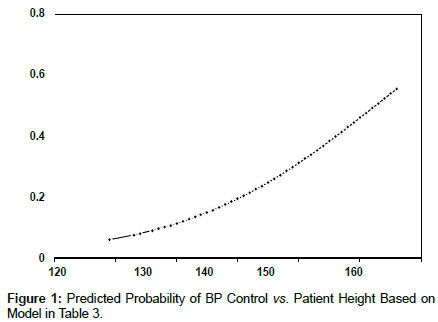
This retrospective study was conducted for a random sample of patients in the outpatient primary care clinic in King Abdulaziz Medical City (KAMC) in Riyadh during 2016-2017. Patients were included if they had records of 3 consecutive blood pressure (BP) readings at least 1 month apart. In addition to BP, data on several patient demographic and medication-related data were also collected including age, gender, weight, height, body mass index (BMI), comorbidities and antihypertensive medications including thiazide-type diuretics, calcium channel blocker (CCB), angiotensin-converting enzyme inhibitors (ACEI), or angiotensin receptor blocker (ARB). Lack of BP control was defined as having a BP measure of ≥ 140/90 on at least two consecutive readings (Figure 1).
Statistical analysis
Descriptive statistical analyses were performed for the study sample. Continuous variables were summarized using mean (SD), median and interquartile range (IQR). Proportions were used for categorical variables. Management of hypertension (hypertension control status) was assessed and compared by demographic and clinical factors. Categorical data were analyzed using the chi-square test. The distribution of all continuous data will be examined. For continuous variables with normal distribution, a t-test was used for comparisons. If there was evidence against normality, the nonparametric Mann-Whitney U test is utilized. A logistic regression analysis was used to determine the effect of height on BP control. Adjustments were made for several demographic and clinical factors including age, gender, weight, height, BMI, co-morbidities and antihypertensive medications. Statistical significance was considered at p<0.05. All statistical analyses were performed using SPSS 21.0 (Release 21.0.0.0, IBM, USA).
Results
A total of 105 subjects were included. Descriptive statistics of the study sample are displayed in Tables 1-3. Average patient age was 66.4 (SD = 11.6) years, with 51% males. Average weight was 78.0 (SD = 19.8) KG, average BMI was 31.0 (SD = 10.4) Kg/m2. Fifty six percent of patients had 3 or more comorbidities and about half of patients had 3 or more antihypertensive medications. BP control was evaluated and achieved in 71 patients (66%). Results from comparing BP control by several patient demographic and clinical characteristics are provided in Table 2. Average ± SD weight among patients with uncontrolled hypertension was 155.5±14.6 vs. 161.0±9.2 for those with controlled BP levels (p = 0.048).
| Factor | Value |
|---|---|
| Gender n (%) | |
| Female | 52 (49.5%) |
| Male | 53 (50.5%) |
| Age (years) mean ± SD | 66.4 ± 11.6 |
| median (IQR) | 68 (60-75) |
| Weight (KG) mean ± SD | 78.0 ± 19.8 |
| median (IQR) | 78 (63-91) |
| Height (CM) mean ± SD | 159.2 ± 11.4 |
| median (IQR) | 160 (152-167) |
| BMI (KG/M2) mean ± SD | 31.0 ± 10.4 |
| median (IQR) | 30.4 (24.6–36.1) |
| Number of comorbidities | |
| One | 12 (11.4%) |
| Two | 34 (32.4%) |
| Three | 28 (26.7%) |
| Four or more | 31 (29.5%) |
| Number of BP medications | |
| One | 21 (20.0%) |
| Two | 32 (30.5%) |
| Three | 27 (25.7%) |
| Four or more | 25 (23.8%) |
Table 1: Descriptive Statistics of the Study Sample. N=105.
| Factor | Uncontrolled HTN |
Controlled HTN |
p-value* |
|---|---|---|---|
| All patients | 34 (32.4%) | 71 (67.6%) | |
| Gender n (%) | 0.37 | ||
| Male | 15 (28.3%) | 38 (71.7%) | |
| Female | 19 (36.5%) | 33 (63.5%) | |
| Age (years) mean ± SD | 64.1 ± 14.1 | 67.6 ± 10.1 | 0.15 |
| median (IQR) | 67 (56.8-75) | 69 (61-75) | |
| Weight (KG) mean ± SD | 77.6 ± 18.9 | 78.2 ± 20.4 | 0.88 |
| median (IQR) | 76 (64.5-92) | 79 (62.5-90.5) | |
| Height (CM) mean ± SD | 155.5 ± 14.6 | 161.0 ± 9.2 | 0.048 |
| median (IQR) | 156.5 (146-164) | 160 (155-168) | |
| BMI (KG/M2) mean ± SD | 33.3 ± 12.8 | 29.9 ± 8.9 | 0.12 |
| median (IQR) | 31.7 (26.9-37.7) | 29.4 (24.4-35.6) | |
| # Comorbidities | 0.65 | ||
| One | 3 (25.0%) | 9 (75.0%) | |
| Two | 13 (38.2%) | 21 (61.8%) | |
| Three | 7 (25.0%) | 21 (75.0%) | |
| Four or more | 11 (35.5%) | 20 (64.5%) | |
| 0.15 | |||
| # BP medications | |||
| One | 6 (28.6%) | 15 (71.4%) | |
| Two | 11 (34.4%) | 21 (65.6%) | |
| Three | 5 (18.5%) | 22 (81.5%) | |
| Four or more | 12 (48.0%) | 13 (52.0%) |
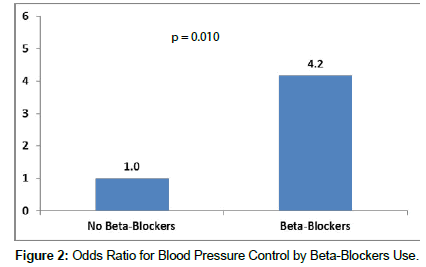
Results from logistic regression analysis showed that higher likelihood of controlled BP was also significantly associated with increased height [OR 95% CI, per 10 cm increase: 1.80 (1.15, 2.82); p = 0.010]. Patients receiving betablockers were significantly more likely to have controlled BP [odds ratio (OR) 95% CI: 4.2 (1.4-12.4); p=0.010]. Having more than one antihypertensive drug was significantly associated with a lower likelihood of BP control.
Table 2: Management of Hypertension (Hypertension Control Status) by Demographic and Clinical Factors. Total Number of Subjects = 105.
| Factor | Mean or percent | OR | 95% CI | p-value |
|---|---|---|---|---|
| Age (per 10 years) | 66.4 | 1.42 | (0.95, 2.13) | 0.090 |
| Weight (per 10 KG) | 78.0 | 1.14 | (0.89, 1.46) | 0.29 |
| Height (per 10 CM) | 159.2 | 1.80 | (1.15, 2.82) | 0.010 |
| Number of BP medications | 2.6 | 0.58 | (0.39, 0.87) | 0.009 |
| Beta Blockers (yes vs. no) | 43.8% | 4.17 | (1.4, 12.41) | 0.010 |
Table 3: Multivariate Logistic Regression Model for Blood Pressure Control.
Discussion
Our study demonstrated that hypertension was significantly more controlled with increased height. Also, beta-blockers appeared to be effective for controlling BP in hypertensive patients (Figure 2). These results confirm findings from other published international studies which reported that the incidence of hypertension is decreased in people with increased height. There are four mechanisms that link increased height with lower risk of coronary heart disease; increased pulmonary function, coronary vessel diameter, insulin like growth factor and genetic factors. Physiologically, Poiseuille’s law states that the resistance to flow in a vessel is directly proportional to the length of the vessel. This can be seen in giraffes, which are the tallest among 47 species of terrestrial mammals. Biologically, a negative relation is proven according to Barker’s hypothesis which states that better conditions in early life (taller) result in better health outcomes in later life (less hypertension). Several studies have focused on the relationship between hypertension and height. These studies reported that height might be inversely associated with prevalence of hypertension [6,8,9]. However, some potential confounders were not fully adjusted in these studies, such as obesity, which might mediate the association between height and hypertension risk. It is well established that obesity is a risk factor for hypertension [10-16].
With the exception of alpha-blockers and beta-blockers, the remaining classes of antihypertensive drugs are similar in their impact on lowering BP which is associated with cardiovascular morbidity and mortality. We found that Patients on beta-blockers were significantly more likely to have controlled BP [odds ratio (OR) 95% CI: 4.2 (1.4- 12.4); p = 0.010]. However, beta-blockers should not be the first line drug for hypertensive patient who do not have angina or recent myocardial infarction. This is mainly because the balance between efficacy and safety for beta-blockers is less favorable in comparison with other anti-hypertensive agents. In general, a combination therapy is more effective in lowering BP than monotherapy and our analysis showed that increased number of antihypertensive medications was associated with a lower likelihood of BP control.
The strength of this study is its methodological contribution and reinforcement of the previously demonstrated relationship between some known patient factors and the likelihood of BP control through detailed analyses a set of hypothesized factors related to that disease. However, our finding on beta-blockers was not in line with the recent guidelines on the management of hypertension where ace-inhibitors are recommended as first line treatment of high BP.
Our study has a number of limitations. First, it is generally difficult to estimate the causal association between height and BP control. Second, all participants in the present study were restricted to middle-aged and older patients, potentially reducing the generalizability of the study findings. Third, height and hypertension might be jointly determined by genetic factors and their association is hard to assess. Also, although we had adjusted for some potential confounders, the observed association between height and BP control might be confounded by other factors that were not measured in our study, such as nutrition in childhood and birth weight. Lastly, this is a relatively small study, and hopefully a future investigation will be conducted including a larger and more representative sample from both the inpatient and outpatient setting with more variant demographic and clinical characteristics.
Conclusion
In this study, poor BP control was independently associated with decreased height. Beta-blockers appeared to be effective for controlling BP in hypertensive patients. Further studies are warranted to confirm these findings.
References
- Song L, Shen L, Li H, Liu B, Zheng X (2016) Height and prevalence of hypertension in a middle-aged and older Chinese population. Scientific Reports 6.
- Song YH (2014) The correlation of blood pressure with height and weight in Korean adolescents aged 10–19 years; The Korean National Health and Nutrition Examination Surveys (2009–2011), Korean J Pediatr 57: 35-40.
- Fujita Y, Kouda K, Nakamura H, Nishio N, Takeuchi H (2010) Relationship between height and blood pressure in Japanese school children. Pediatr Int 52: 689-693.
- Olatunbosun ST, Bella AF (2000) Relationship between height , glucose intolerance, and hypertension in an urban African black adult population: a case for the “thrifty phenotype” hypothesis? J Natl Med Assoc 92: 265-268.
- Perkins JM, Subramanian SV, Davey Smith G, Özaltin E (2016) Adult height, nutrition, and population health. Nutr Rev 74: 149-165.
- El-Bikai R, Tahir MR, Tremblay J, Joffres M, Šeda O, et al. (2015) Association of age-dependent height and bone mineral density decline with increased arterial stiffness and rate of fractures in hypertensive individuals. J Hypertens 33: 727-735.
- Sichieri R, Siqueira KS, Pereira RA, Ascherio A (2000) Short stature and hypertension in the city of Rio de Janeiro, Brazil. Public Health Nutr 3: 77-82.
- Florêncio TT, Ferreira HS, Cavalcante JC, Sawaya AL (2004) Short stature, obesity and arterial hypertension in a very low-income population in North-eastern Brazil. Metab Cardiovasc Dis 14: 26-33.
- Hu G, Barengo NC, Tuomilehto J, Lakka TA, Nissinen A, et al. (2004) Relationship of physical activity and body mass index to the risk of hypertension: a prospective study in Finland. Hypertension 43: 25-30.
- Langenberg C, Hardy R, Kuh D, Wadsworth ME (2003) Influence of height, leg and trunk length on pulse pressure, systolic and diastolic blood pressure. J Hypertens 21: 537-543.
- Silventoinen K (2003) Determinants of variation in adult body height. J Biosocial Sci 35: 263-285.
- Bjerregaard P (2010) Childhood conditions and education as determinants of adult height and obesity among Greenland Inuit. Amer J Hum Biol 22: 360-366.
- Perola M, Sammalisto S, Hiekkalinna T, Martin NG, Visscher PM, et al. (2007) Combined genome scans for body stature in 6,602 European twins: evidence for common Caucasian loci. PLoS Genet 3: e97.
- DeBoer MD, Lima AA, Oría RB, Scharf RJ, Moore SR, et al. (2012) Early childhood growth failure and the developmental origins of adult disease: do enteric infections and malnutrition increase risk for the metabolic syndrome? Nutr Rev 70: 642-653.
- Thrift AG, Srikanth V, Fitzgerald SM, Kalyanram K, Kartik K, et al. (2010) Potential roles of high salt intake and maternal malnutrition in the development of hypertension in disadvantaged populations. Clin Exp Pharmacol Physiol 37: e78–e90.
- James PA, Oparil S, Carter BL, Pharm D (2014)The 2014 JNC 8 and 2017 AHA/ACA Guidelines for Management of High Blood Pressure in Adults. Hypertension Guidelines. Clinical Review and Education 311: 507-520.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi