Case Report, Int J Cardiovasc Res Vol: 7 Issue: 2
Troponin and St Segment Elevation in a Diabetic Ketoacidosis Patient without Acute Coronary Syndrome
1Division of Endocrinology and Metabolism, Xiamen Chang Gung Hospital, Xiamen, China
2Xiamen Justcan Health Management CO. Ltd., China
*Corresponding Author : Liu Yuping (BS)
Division of Endocrinology and Metabolism, Xiamen Chang Gung Hospital, Xiefei Road No.123, Haicang discrict, Xiamen City, China
Tel: +8615359885356
E-mail: yuping@adm.cgmh.com.cn
Received: March 01, 2018 Accepted: March 13, 2018 Published: March 19, 2018
Citation: Yuping L, Yichun T (2018) Troponin and St Segment Elevation in a Diabetic Ketoacidosis Patient without Acute Coronary Syndrome. Int J Cardiovasc Res 7:2. doi: 10.4172/2324-8602.1000342
Abstract
Diabetic ketoacidosis (DKA) is a major acute complication in diabetes. The acute coronary syndrome is a risk factor for DKA with a higher associated mortality rate. Also diabetic mellitus is a high risk factor to acute coronary syndrome. Thus, we need to recognize severe cardiac events in a timely fashion when DKA happen. Although DKA initially shows similar symptoms and signs to acute coronary syndrome, including hyperkalaemia, electrocardiographic ST segment elevation and increased cardiac enzymes. We report a patient who presented with a ST segment elevation and cardiac enzymes levels elevation due to DKA without acute coronary syndrome.
Keywords: Diabetic ketoacidosis; Hyperkalemia; ST segment elevation; Acute coronary syndrome
Case-Presentation
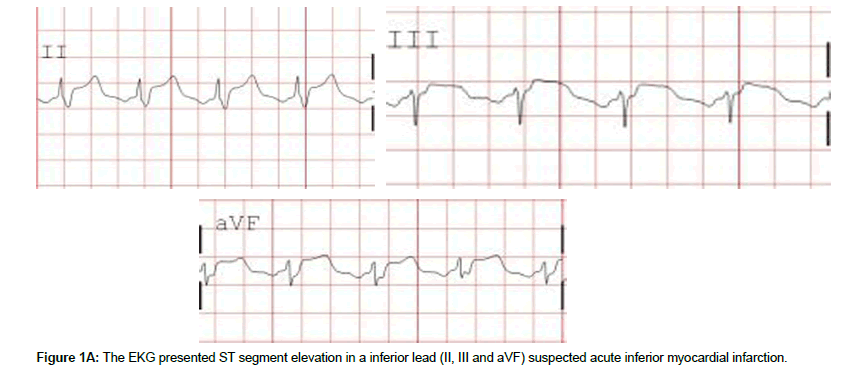
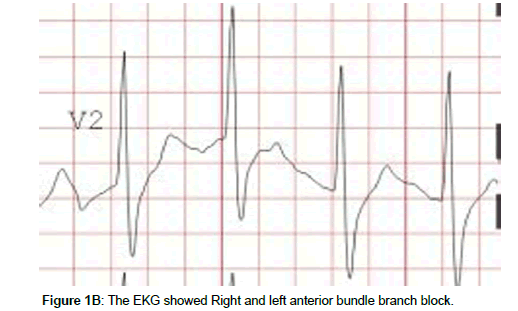
A 68-year-old Chinese man with delirium and continuous nausea and vomiting for 2 days was presented to the Endocrinology Department in our hospital. The medical history included type 2 diabetic for 8 years and recently diagnosed neuropathy. He was treated with premixing 30 U insulin injections twice daily. The patient had not discontinued the insulin injections until presentation. Physical examination of the abdomen of the patient was normal. The initial electrocardiogram (ECG) revealed vascular risk factors. In addition to the long diabetic history, he smoked one pack of cigarettes daily. Through initial assessment, he had delirium with tachycardia (118 beats/minute), tachypnea (20 breaths/minute), and hypotension (89/30 mmHg). ST segment elevation (Figure 1A, B) in inferior leads (II, III, and aVF) suggested an acute inferior myocardial infarction, with right and left anterior bundle branch block. A urine dipstick test showed ketones. Venous blood glucose test showed a very high glucose concentration (1188 mg/dL). The arterial blood gas analysis indicated metabolic acidosis (pH = 7.14, carbon dioxide partial pressure = 13.2 mmHg, oxygen partial pressure = 147.6 mmHg, bicarbonate concentration = 4.5 mmol/L, and base excess = -24.4 mmol/L) with an anion gap of 34 mmol/L. The cardiac enzymes levels were showed as follows: troponin-I, 112.5 pg/ml; and CK-MB, 27.4 ng/ml. An echocardiogram demonstrated that the ejection fraction was 70%. We provisionally diagnosed as DKA, possibly precipitated by an acute myocardial infarction.
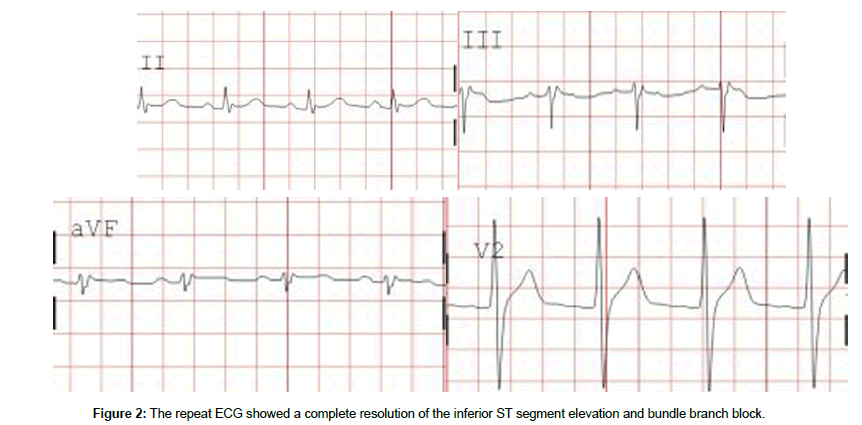
Since our patient had a haemorrhage involving the digestive tract, aspirin, clopidogrel, and low molecular weight heparin were contraindicated. We then treated the patient with fluid replacement using normal saline, intravenous insulin at 4 units/h, and a statin (atorvastatin) to stabilize plaque. The biochemical profile of serum was showed: potassium, 6.3 mEq/L; sodium, 114 mEq/L; urea, 28 mmol/L; creatinine, 338 mmol/L; and glucose, 1188 mg/dL. Cardiac sonography showed no segmental wall motion abnormality and an intense ejection fraction. The amylase and lipase levels were elevated (2152 U/L and 2265 U/L, respectively). The ECG pattern and elevations of cardiac enzymes levels represented two risk factors of coronary heart disease. However, the diagnosis of acute myocardial infarction was in question due to a normal ECG on the second day (hospital day). Active digestive tract bleeding was a contraindication to coronary angiography to assess anterior damage and other possible severe complications, such as heart failure. A repeat biochemical test after 8 h was showed in the following values: sodium, 135 mEq/L; potassium, 4.45 mEq/L; Creatinine, 82 md/dL; and glucose, 396 mmol/L. A repeat ECG showed a complete resolution of the inferior ST segment elevation and bundle branch block (Figure 2). The cardiac enzymes concentrations in the third day after admission were normal, indicating the complete recovery of the patient. When he was discharged 7 days after admission, both the ECG and biochemical results were normal as well.
Discussion
Our case demonstrated ST segment elevation and increased cardiac enzymes levels with DKA, but without coronary artery disease. DKA is an acute complication in diabetes and results in higher mortality rate from some risk factors, such as a lag in hospitalization, severity of ketoacidosis, and peripheral vascular insufficiency [1]. Myocardial infarction is also one of the other risk factors .Indeed, Johnson reported that one of the major cause of all deaths occurring within 48 h of hospitalization for DKA is myocardial infarction [2].
We test the metabolic profiles of blood using arterial blood gas analysis. The PH is around 7.14, which indicated metabolic acidosis. The venous blood glucose level is 1188 mg/dL, much higer than the normal concentration. In addition, the urine dipstick for ketones was positive. Based on this information, the patient was diagnosed as DKA. On the other hand, the patient initially appeared to have ST segment elevation and an increased cardiac troponin-I level, including EKG changes and cardiac enzymes abnormalities, which may suggest an acute myocardial infarction. Indeed, there was case reported that ST segment elevation following Sino ventricular rhythm in a patient with DKA [3]. However, in this case, upon correction of the acidosis treated with insulin and water, the ECG and cardiac enzymes normalized, which excluded an acute inferior myocardial infarction. Hyperkalemia affects myocardial conduction and repolarization complicating DKA, which result in impaired myocardial contractility and Sino ventricular arrhythmia or sudden death.
Intraventricular conduction damage presents as widening of the QRS wave, which is also called a right bundle branch block, and is combined with left anterior or posterior hemi-block [4]. Hyperkalaemia can progressively lead to electrocardiographic changes. The T wave is initially higher and symmetric. The P wave disappears when the potassium concentration is > 7.5 mmol/L. The worst outcome is a deadly cardiac arrhythmia, including a Sino ventricular rhythm or sudden death. Also, the hyperkalaemia caused a ST segment elevation, which is called a pseudo infarction pattern due to the infusion of the terminal R’ portion of the QRS with the T wave [5]. The EKG change was affected by a primary repolarization abnormality or an artifact. A possible mechanism for the same finding has been hypothesized. Hyperkalaemia combined with stress cardiac troponin elevations without acute myocardial infarction due to DKA is strongly correlated with a subsequent major cardiovascular event [6]. Moller reported that acidosis and very high levels of free fatty acids caused cardiac membrane damage and cardiac biomarker release [7].
Anthony concluded that elevated cardiac troponin-I level in patients diagnosed as decompensated diabetes and without evidence of acute coronary syndrome is strongly correlated with a subsequent major cardiovascular event, such as acute coronary syndrome. Thus, elevated level of troponin-I during metabolic abnormalities identifies a group of patients at an increased risk for poor long-term outcomes or MACE post-discharge. Whether these patients may benefit from the early detection or not, risk stratification and preventive interventions remains to be investigated in the future [6].
Conclusion
The case involved DKA complicated by hyperkalaemia and cardiac enzymes levels elevation without acute coronary syndrome. The patient is at increased risk for mortality due to MACE in the future. Therefore, we should pay attention to prevent such an event. Medication options should be thoroughly studied in the future.
Acknowledgements
We would like to thank the staff of the medical unit for their help in the management of this patient. This research was not supported by any founding disclosure.
References
- Seth P, Kaur H, Kaur M (2015) Clinical Profile of Diabetic Ketoacidosis: A Prospective Study in a Tertiary Care Hospital.Journal of clinical and diagnostic research. JCDR 9: 1-4.
- Johnson DD, Palumbo PJ, Chu CP (1980) Diabetic ketoacidosis in a community-based population. Mayo Clinic proceedings 55: 83-88.
- Tatli E, Altun A, Yilmaztepe M (2007) ST segment elevation following sinoventricular rhythm in a patient with diabetic ketoacidosis. Cardiology journal 14: 497-499.
- Froelicher VF (1980) An introduction to the applications, methodology and interpretation of exercise electrocardiography. Cardiology 66: 223-235.
- Levine HD, Wanzer SH, Merrill JP (1956) Dialyzable currents of injury in potassium intoxication resembling acute myocardial infarction or pericarditis. Circulation 13: 29-36.
- Eubanks A, Raza F, Alkhouli M, Glenn AN, Homko C, et al. (2012) Clinical significance of troponin elevations in acute decompensated diabetes without clinical acute coronary syndrome. Cardiovascular Diabetology 11: 154.
- Moller N, Foss AC, Gravholt CH, Mortensen UM, Poulsen SH, et al. (2005) Myocardial injury with biomarker elevation in diabetic ketoacidosis. J Diabetes Complications 19: 361-363.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi