Research Article, Int J Cardiovasc Res Vol: 6 Issue: 5
Ventricular Repolarization in Patients with Decompensated Liver Cirrhosis and its Relation to the in-Hospital Outcome: Electrocardiographic Study
Rania Yahia1*, Mohamed Yahia2 and Waleed Abdou2
1Department of Internal Medicine, faculty of Medicine, University of Banha, Banha, Egypt
2Department of Cardiology, faculty of Medicine, University of Menoufia, Shebin Alkoum, Egypt
*Corresponding Author : Rania Yahia
Department of Internal Medicine, faculty of Medicine, University of Banha, Banha, Zip code: 13518, Egypt
Tel: 0020482575470
E-mail: Raniayahia1980@gmail.com
Received: September 18, 2017 Accepted: October 10, 2017 Published: October 15, 2017
Citation: Yahia R, Yahia M, Abdou W (2017) Ventricular Repolarization in Patients with Decompensated Liver Cirrhosis and its Relation to the in-Hospital Outcome: Electrocardiographic Study. Int J Cardiovasc Res 6:5. doi: 10.4172/2324-8602.1000328
Abstract
Background: Prolonged ventricular repolarization has been documented in patients with chronic liver disease. The objective of this study was to study the electrocardiographic QTc interval in patients with decompensated liver disease and its relation to the in-hospital outcome.
Methods: We retrospectively studied 75 patients with hepatic encephalopathy. The QTc interval was measured in a 12-lead electrocardiogram obtained on admission.
Results: Patients were divided into two groups according to their clinical outcome during hospitalization. The first group included 53 (70.7%) patients who survived, and the second group included 22 (29.3%) patients who died. QTc interval was significantly prolonged in died patients than patients who survived (p<0.001). There was insignificant difference between two groups regarding age, sex, smoking status, hypertension, diabetes mellitus and basal laboratory findings except for serum creatinine level (p = 0.006) and MELD score (p = 0.033).
Conclusions: In patients with hepatic encephalopathy, QTc interval was significantly higher in patients who died than in patients who survived, however, in multivariate logistic regression analysis, QTc interval, was not predictors of survival.
Keywords: Liver disease, QTc interval, ventricular repolarization
Abbreviations
HE: Hepatic Encephalopathy, AST: Aspartate Aminotransferase, ALT: Alanine Aminotransferase, INR: International Normalized Ratio, HBsAg: Hepatitis B Surface Antigens, HCV: Hepatitis C Virus, MELD: Model for End-Stage Liver Disease, QTc: QT corrected for heart rate, DM: Diabetes Mellitus, HTN: Hypertension, LV: Left Ventricle, IVSD: Interventricular Septal Diameter, LVEDD: End Diastolic Diameter, LVESD: End Systolic Diameter, EF: Ejection Fraction, PASP: Pulmonary Artery Systolic Pressure
Introduction
A prolonged QT interval was previously encountered in chronic liver disease [1,2]. Hepatic encephalopathy (HE) is a serious condition of decompensated liver cirrhosis that presents as a wide scope of neuropsychological clinical states ranging from negligible encephalopathy to coma. In patients with liver cirrhosis, hepatic decompensation in the form of HE is associated with shorter survival [3]. Interactions between the heart and the liver have been delineated. Affects on the cardiovascular system in advanced liver disease are perceived in the form of left ventricular hypertrophy, impaired diastolic filling, chronotropic inadequacy, pulmonary hypertension, decreased vascular resistance, and cardiac arrhythmias. The term cirrhotic cardiomyopathy describes these changes in the heart; they are related to both histological and fibrotic changes and contribute to risk of electrical heterogeneity and arrhythmia [4-6].
The relationship between cardiac structural heterogeneity and cardiovascular events in patients with liver cirrhosis was studied in some post-mortem research that described edema in the subendocardium, patchy fibrosis in myocytes, and myocardial hypertrophy [7].
The electrocardiographic QT interval could assess abnormal ventricular repolarization. Prolonged ventricular repolarization in chronic liver disease may elicit serious arrhythmias during distressing conditions, and it is a predictor of poor outcome [8].
Aim of the study
The aim of this work was to study the electrocardiographic QTc interval in patients with decompensated liver disease and its relation to the in-hospital outcome.
Materials and Methods
A retrospective, observational study was conducted to 75 patients (44 male and 31 female) with decompensated liver disease who were admitted to Banha University Hospital, Egypt, from November 2014 to February 2016. The study populace was orderd into two groups as indicated by their clinical outcome during hospitalization. The first group included patients who survived, and the second group included patients who died. The two groups of patients were retrospectively evaluated. The study followed the principles of the Declaration of Helsinki and and was approved by our research committee. Consent was obtained from patients who survived and permission from patients’ relatives for those who died. The study excluded patients who had baseline changes in their resting electrocardiograms as left or right bundle branch block, pre-excitation disorders, atrial fibrillation, atrioventricular heart block, and pacemaker musicality. Also we excluded patients with a history of ishemic heart disease or revascularization, heart failure, and patients who received any medications that affect QT interval.
A hepatologist obtained the diagnosis of liver cirrhosis and grading of HE for each patient according to the West Haven classification system, from grade 0 to 4 [9].
The following diagnostic tests were analyzed:
Laboratory investigations
Liver function tests [total bilirubin, direct bilirubin, albumin, aspartate aminotransferase (AST), alanine aminotransferase (ALT), and international normalized ratio (INR) for prothrombin time and concentration], viral hepatitis markers (HBsAg and HCV antibodies), serum creatinine, and complete blood picture. Model for End-Stage Liver Disease (MELD) score [10] was calculated by using laboratory results of creatinine, bilirubin and INR to determine the seriousness of liver cirrhosis. Management of both groups was similar. The principal lines of management were mainly control of precipitating factors for HE, supportive treatment, in addition to lactulose and rifaximine therapy.
Standard 12–lead resting electrocardiography
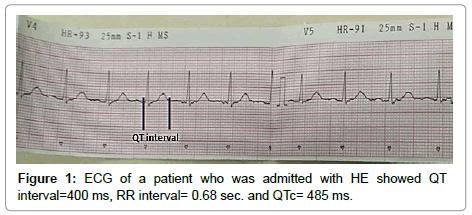
Cardiofax C ECG–1150 machine was used to record 12–lead ECGs on admission at speed of 25 mm/s and 1 mV/cm calibration. Heart rate, PR interval, and QRS time, and QT interval were measured. QT interval was surveyed as the time between the principal redirection of the QRS complex and the purpose of return of the T wave to the isoelectric line. QT intervals were measured in leads where it was plainly recognizable, while patients with U waves, flat, or biphasic T waves were excluded. QT interval corrected for heart rate (QTc) was figured by separating the QT interval in seconds by the square base of R-R interval in seconds [11] (Figure 1).
Two-dimensional transthoracic echocardiogram
Echocardiographic appraisal was performed utilizing a Vivid 3 master N cardiovascular ultrasound framework (Vingmed-General Electric, Norway) with a 3.5 MHz transducer. standard apical and parasternal imaging windows were used. End systolic, and end diastolic measurements of the left ventricle were measured from parasternal long-axis view. Modified Simpson method was used to estimate Ejection fraction.
Statistical analysis
Information were encouraged to the PC and investigated utilizing IBM SPSS software package variant 20 (Armonk, NY: IBM Corp).The Kolmogorov- Smirnov, Shapiro and D’agstino tests were utilized to confirm the ordinariness of dissemination of factors, Comparisons between groups for clear cut factors variables were assessed using Chi-square test (Fisher or Monte Carlo). Student t-test was utilized to think about two groups for ordinarily appropriated quantitative factors. Mann Whitney test was utilized to compare between two groups for unusually appropriated quantitative factors.
The relationship between mortality as dependent variable and QTc intervals, MELD score and serum creatinine as independent variables was decided by Multivariate logistic regression analysis. Results are reported as odd ratio (OR) (95% confidence interval [CI]). P value less than 0.05 was viewed as significant.
Spearman coefficient was utilized to relate between quantitative factors. Receiver operating characteristic curve (ROC) was utilized to decide the demonstrative execution of the markers. Range over half gives adequate execution and zone around 100% is the best execution for the test. Centrality of the acquired outcomes was judged at the 5% level.
Results
The study cohort consisted of 44 males (58.7%) and 31 females (41.3%) with a mean age of 56 (44–67) year presented with decompensated liver cell failure in the form of HE. The etiology of liver cirrhosis was chronic hepatitis C in 69 (92%) patients and chronic hepatitis B in 6 (8%) patients. The subjects were ordered into two groups as indicated by their clinical outcome during hospitalization period. The first group included 53 (70.7%) patients who survived, and the second group included 22 (29.3%) patients who died. The two groups of patients were retrospectively evaluated.
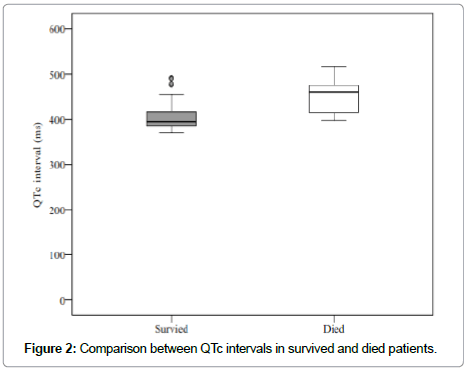
There was insignificant difference between two groups regarding age, sex, smoking status, hypertension, diabetes mellitus and basal laboratory findings except for serum creatinine level (p = 0.006) and MELD score (p = 0.033). QRS duration, QT intervals, LV ejection fractions and dimensions didn’t also differ significantly in studied groups. However, QTc interval was significantly higher in patients who died than in patients who survived (Figure 2). Clinical features, electrocardiographic and echocardiographic data of the studied patients are recorded in Table 1.
| Survived (n = 53) |
Died (n = 22) |
Test of sig. | p | |
|---|---|---|---|---|
| Age | 56(44–67) | 56.5(44–67) | U=577 | 0.944 |
| MELD score | 17.4±4.8 | 20.0±4.2 | t=2.173 | 0.033 |
| Albumin | 2.5(1.8–3.2) | 2.4(1.8–3.2) | U=582.5 | 0.995 |
| Total Bilirubin | 2.3(0.5–6.7) | 1.9(0.7–7.2) | U=522.5 | 0.481 |
| INR | 1.8(0.8–2.7) | 1.7(0.8–2.6) | U=576.5 | 0.939 |
| AST | 79(44–137) | 84.5(56-136) | U=544.5 | 0.654 |
| ALT | 55(23–81) | 47.5(22–79) | U=472 | 0.196 |
| Creatinine | 1.6(0.7–3.3) | 2(0.8–3.8) | U=345 | 0.006 |
| Sex | ||||
| Male | 28(52.8%) | 16(72.7%) | χ2=2.538 | 0.111 |
| Female | 25(47.2%) | 6(27.3%) | ||
| Stage of HE | ||||
| II | 4(7.5%) | 0(0.0%) | χ2=1.780 | 0.398 |
| III | 16(30.2%) | 9(40.9%) | ||
| IV | 33(62.3%) | 13(59.1%) | ||
| Smokers | 9(17.0%) | 2(9.1%) | χ2=0.773 | 0.491 |
| DM | 12(22.6%) | 6(27.3%) | χ2=0.183 | 0.669 |
| HTN | 15(28.3%) | 7(31.8%) | χ2=0.093 | 0.761 |
| Ascites | 22(41.5%) | 10(45.5%) | χ2=0.099 | 0.753 |
| IVSD (cm) | 1.1(0.6–1.5) | 1.2(0.9–1.4) | U=554.5 | 0.736 |
| LVEDD (cm) | 5(4.5–5.5) | 4.9(4.5–5.4) | U=556 | 0.751 |
| LVESD (cm) | 3.0±00.4 | 2.9±0.3 | t=1.106 | 0.273 |
| LVEF % | 66(53–71) | 66(53–74) | U=559 | 0.779 |
| PASP (mmHg) | 27(20–43.) | 26(22–41) | U=525.5 | 0.502 |
| QTc interval (ms) | 395(369–492) | 459(398–516) | U=157 | <0.001 |
| PR interval (ms) | 173.1±23.2 | 172.2±21.1 | t=0.159 | 0.874 |
| QRS duration (ms) | 96.2±10.0 | 98.5±10.1 | t=0.923 | 0.359 |
Table 1: Comparison between the two studied groups according to patient characteristics, electrocardiographic and echocardiographic data.
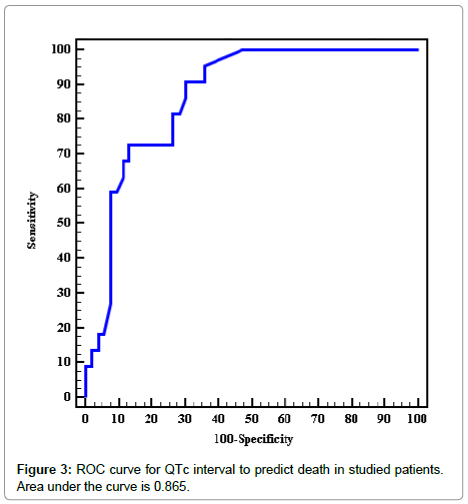
Regarding sensitivity and specificity of QTc interval to expect inhospital mortality, the study showed QTc interval cutoff value >410 ms had sensitivity of 81.82% and specificity of 71.70% to predict inhospital mortality, P<0.001 (Table 2 and Figure 3).
| AUC | p | 95% C.I | Cut off | Sensitivity | Specificity | PPV | NPV | ||
|---|---|---|---|---|---|---|---|---|---|
| LL | UL | ||||||||
| QTc interval | 0.865* | <0.001 | 0.784 | 0.947 | >410 | 81.82 | 71.70 | 54.5 | 90.5 |
Table 2: Agreement (sensitivity, specificity) for QTc interval to predict mortality.
Multivariate logistic regression analysis using in-hospital mortality as dependent variable and QTc intervals, MELD score and serum creatinine as independent variables, the study showed that serum creatinine and QTc had the highest association with mortality (OR, 7.641 and 2.736 respectively). The association between inhospital mortality and all independent variables was statistically nonsignificant, p ≥ 0.05 (Table 3).
| B | SE | P value | OR | 95% CI | ||
|---|---|---|---|---|---|---|
| LL | UL | |||||
| MELD score | 0.516 | 0.388 | 0.184 | 1.676 | 0.783 | 3.587 |
| Creatinine | 2.033 | 1.359 | 0.135 | 7.641 | 0.532 | 109.730 |
| QTc interval | 0.043 | 0.034 | 0.203 | 1.044 | 0.977 | 1.116 |
Table 3: Multivariate logistic regression analysis for mortality.
In correlation analysis, QTc interval was positively correlated with both stage of HE (r =0.239, p=0.039) and serum total bilirubin level, r=0.233 and p=0.044 (Table 4).
| Variables | r | P |
|---|---|---|
| Age | -0.016 | 0.894 |
| Encephalopathy stage | 0.239 | 0.039 |
| MELD score | 0.136 | 0.243 |
| Albumin | -0.018 | 0.877 |
| Total Bilirubin | 0.233 | 0.044 |
| INR | 0.067 | 0.567 |
| AST | 0.046 | 0.692 |
| ALT | 0.104 | 0.373 |
| Creatinine | 0.265 | 0.021 |
| IVSD | 0.023 | 0.844 |
| LVEDD | -0.177 | 0.128 |
| LVESD | -0.153 | 0.189 |
| LVEF | 0.011 | 0.924 |
| PASP | -0.164 | 0.159 |
| PR interval | -0.163 | 0.163 |
| QRS duration | -0.110 | 0.347 |
Table 4: Correlation between QTc with different parameters in all patients.
Discussion
Cardiac abnormalities have frequently been seen in patients with chronic liver disease, and the extent is proportionate to the extent of hepatic cell failure. These abnormalities are detected in the absence of preexisting cardiac diseases. They include increased left ventricular wall thickness, impairment of diastolic function of the heart and sometimes also the systolic function, chronotropic incompetence, and disturbance of the electrophysiological regulation of the heart with alteration of ventricular repolarization and subsequent electrical instability and arrhythmic risk [12].
Repolarization of the myocardium could be evaluated by corrected QT interval (QTc) or corrected QT dispersion (QTDc), which reflects myocardial depolarization and repolarization. The current study provided further information related to guides of dispersion of repolarization and their predictive significance in patients with decompensated liver cirrhosis.
The authors reported prolonged QTc interval obtained at the time of admission in patients with who died, as compared to patients who survived. The current study showed QTc interval cutoff value > 410 ms had sensitivity of 81.82% and specificity of 71.70% to predict in-hospital mortality (P< 0.001).
Previous investigations studied the QT interval in patients with hepatic diseases. The initial study was that of Kowalski et al. who found that the prolonged QT interval was the furthermost broadly documented electrocardiographic deviation in patients with cirrhotic liver [13]. Bal et al. reported prolonged QTc in patients with liver cirrhosis, which returned to normal value in about 50% of them after liver transplantation. Thus the researchers suggested that liver diseases have a pathogenesis regarding the prolonged QTc. They also reported higher mortality in patients with a prolonged QTc interval in those who died compared to those who were alive during a mean follow-up of about 8 years [14].
Day CP et al studied 69 patients with alcoholic liver disease without evidence of structural heart disease; they reported prolonged QT interval and adverse prognosis especially sudden cardiac death in comparison with healthy subjects [15].
Mozos et al. reported that the degree of liver disease in addition to alcoholic etiology was associated with an increased QT interval in patients with liver cirrhosis [16]. Moreover, prolonged ventricular repolarization as assessed by QT interval may initiate life-debilitating arrhythmias amid stressful situations in patients with chronic liver disease, like bleeding, and it was found to be a predictor of poor prognosis [17].
The results of this study agree with Akboga et al., who showed a significant relation parallel of QTc interval with the seriousness of the liver cirrhosis represented by Pugh–Child and MELD scores. However, he also detected a significant association between the seriousness of liver and fragmented QRS among patients, but we didn’t report this , which could be explained by the smaller number of our study in comparison with Akboga et al. in addition, he involved patients with alcoholic liver cirrhosis as an etiology and we didn’t [18].
Bernardi M, et al. suggested role of sympathoadrenergic hyperactivity in prolongation of QT interval in patients with liver cirrhosis irrespective of the etiology, and may have a prognostic significance [19].
Conclusion
The current study provides additional information regard QTc interval and its short term prognostic incentive in patients with decompensated liver disease. In patients with hepatic encephalopathy, QTc interval was significantly higher in patients who died than in patients who survived. In multivariate logistic regression analysis, QTc interval, MELD score and serum creatinine were not predictors of survival.
Conflict of Interest
The authors declare that they have no conflict of interest.
Funding
This research did not receive any specific grant from any funding agency in the public, commercial or not-for-profit sector.
References
- Finucci G, Lunardi F, Sacerdoti D, Volpin R, Bortoluzzi A, et al (1998) QT interval prolongation in liver cirrhosis: reversibility after orthotopic liver transplantation. Jpn Heart J 39: 321–329.
- Mohamed R, Forsey PR, Davies MK, Neuberger JM (1996) Effect of liver transplantation on QT interval prolongation and autonomic dysfunction in end stage liver disease. Hepatology 23: 1128–1134.
- D’Amico G, Garcia-Tsao G, Pagliaro L (2006) Natural history and prognostic indicators of survival in cirrhosis: a systematic review of 118 studies. J Hepatol 44: 217–231.
- Mozos I (2015) Arrhythmia risk in liver cirrhosis. World J Hepatol 7: 662-672.
- Al Hamoudi W, Lee SS (2006) Cirrhotic cardiomyopathy. Ann Hepatol 5: 132-139.
- Wiese S, Hove JD, Bendtsen F, Møller S (2014) Cirrhotic cardiomyopathy: pathogenesis and clinical relevance. Nat Rev Gastroenterol Hepatol 11: 177-186.
- Wong F (2009) Cirrhotic cardiomyopathy. Hepatol Int 3: 294-304.
- Henriksen JH, Fuglsang S, Bendtsen F, Christensen E, Moller S (2002) Dyssynchronous electrical and mechanical systole in patients with cirrhosis. J Hepatol 36: 513–520.
- Blei AT, Cordoba J, Practice Parameters Committee of the American College of Gastroenterology (2001) Hepatic encephalopathy. Am J Gastroenterol 96: 1968-1976.
- Malinchoc M, Kamath PS, Gordon FD, Peine CJ, Rank J, et al (2000) A model to predict poor survival in patients undergoing transjugular intrahepatic portosystemic shunts. Hepatology 31: 864–871.
- Goldenberg I, Moss AJ, Zareba W (2006) QT interval: how to measure it and what is “normal.” J Cardiovasc Electrophysiol 17: 333-336.
- Wiese S, Hove JD, Bendtsen F, Møller S (2014) Cirrhotic cardiomyopathy: pathogenesis and clinical relevance. Nat Rev Gastroenterol Hepatol 11: 177-186
- Kowalski HJ, Abelmann WH (1953) The cardiac output at rest in Laennec’s cirrhosis. J Clin Invest 32: 1025-1033.
- Bal JS, Thuluvath PJ (2003) Prolongation of QTc interval: relationship with etiology and severity of liver disease, mortality and liver transplantation. Liver Int 23: 243-248.
- Day CP, James OF, Butler TJ, Campbell RW (1993) QT prolongation and sudden cardiac death in patients with alcoholic liver disease. Lancet 341: 1423–1428.
- Mozos I, Costea C, Serban C, Susan L (1993) Factors associated with a prolonged QT interval in liver cirrhosis patients. J Electrocardiol 44: 105-108
- Trevisani F, Di Micoli A, Zambruni A, Biselli M, Santi V, et al. (2012) QT interval prolongation by acute gastrointestinal bleeding in patients with cirrhosis. Liver Int 32:1510-1515.
- Akboga MK, Yuksel M, Balci KG, Kaplan M, Gokbulut V, et al (2017) Tp-e Interval, Tp-e/QTc Ratio, and Fragmented QRS Are Correlated with the Severity of Liver Cirrhosis. Ann Noninvasive Electrocardiol 22: 1-6.
- Bernardi M, Calandra S, Colantoni A, Trevisani F, Raimondo ML, et al (1998) Q-T interval prolongation in cirrhosis: prevalence, relationship with severity, and etiology of the disease and possible pathogenetic factors. Hepatology 27: 28-34.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi