Degenerative disc disease: up-front considerations regarding treatment with mesenchymal adipose tissue derived stem cells
Walter Bini
Healthpoint Hospital, UAE
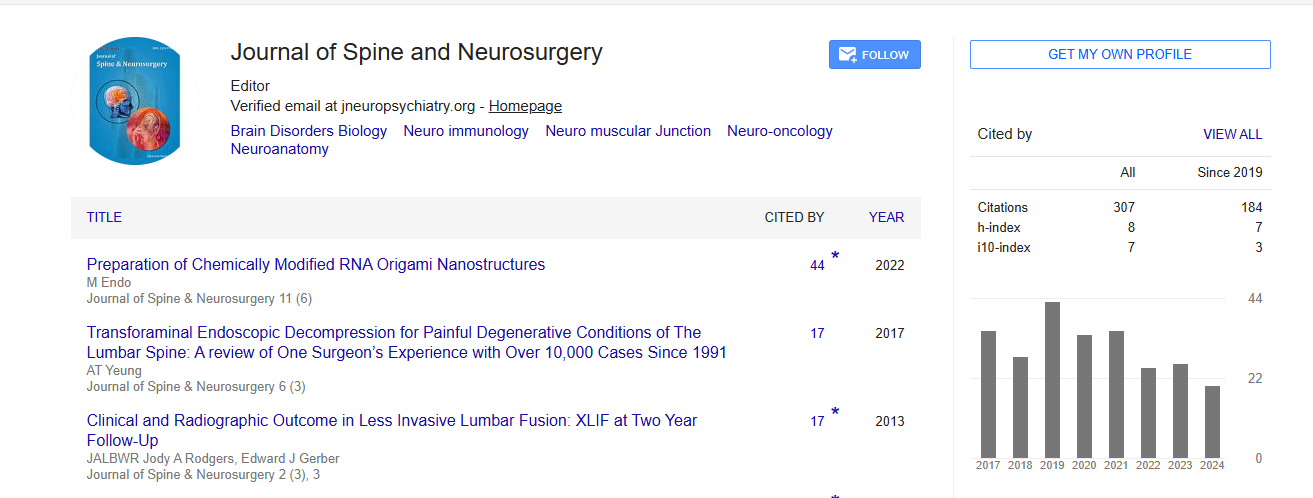
: J Spine Neurosurg
Abstract
Lumbar degenerative disc disease (DDD) poses an ongoing challenge as far as treatment options and alternatives are concerned, especially in younger patients. Over 80% of the adult population presents with one or more episodes of ongoing-progressive low-back pain (LBP). The primary cause is associated with degeneration of the intervertebral disc which is triggered by a decrease of the nucleus pulposus cell population, as evidenced in histological studies. In the presence of a "black disc" without profusion and neurological compromise, microsurgery or even fusion surgery should not be contemplated. Numerous percutaneous techniques have been propagated as a proper way to treat this condition throughout the literature in the past years. They have been primarily focused on the treatment of the pain generated by the involved disc and the subsequent segmental insufficiency, without addressing the degeneration of the disc, and for this reason, have had limited success and remain as pain management tools. Some significant trials in the past (i.e., chondrocyte transplantation trial) and the increasing recent research and achievements with more biological strategies as far as tissue regeneration have motivated the development of a new treatment concept initially applicable to the lumbar spine which will be presented and discussed. Advancements have led to a significant improvement in the understanding of the cell environment and tissue transplantation at a molecular, cellular and immunobiological level. Adipose tissue has already become a central source of clinical and research work involving adipose tissue derived progenitor cells. Endothelial and mesenchymal stem cells derived from adipose tissue are being considered and used in an array of clinical conditions and seem to have clear therapeutic benefits for many disease conditions including those affecting bone, cartilage and muscle. The use of an accessible source with abundant cells which have a high potential for regeneration, clearly is superior in comparison to the chondrocyte option for the lumbar disc. Mesenchymal cells have a high self renewal capacity and a potential for multi lineage differentiation. For this, adipose tissue derived MSCs (ADMSCs) are optimal candidates for tissue regeneration and can be obtained from the patient in a one step procedure-treatment.
Biography
Walter Bini completed his Diploma from Westminster School, Simsbury Connecticut, USA and his Post-graduate Degree from Universidad de Zaragoza, Facultad de Medicina, Zaragoza, Spain. In 2014, he became the Middle East Chairman of ISLASS. He was the Head of Neurosurgery at Sheikh Khalifa General Hospital, UAQ–UAE from 2014–2016. Currently, he is the Lead Neurosurgeon responsible for spinal surgery in the Waldkrankenhaus for special surgeries by Leipzig in Germany and also Visiting Consultant Neurosurgeon of the Orthopaedic Department of Healthpoint Hospital in Abu Dhabi, UAE.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi