Pelvic organ prolapse repairs with biologic and synthetic grafts in a large United States population based cohort
Rogo-Gupta L, Dallas KB and Elliott CE
Stanford University, USA
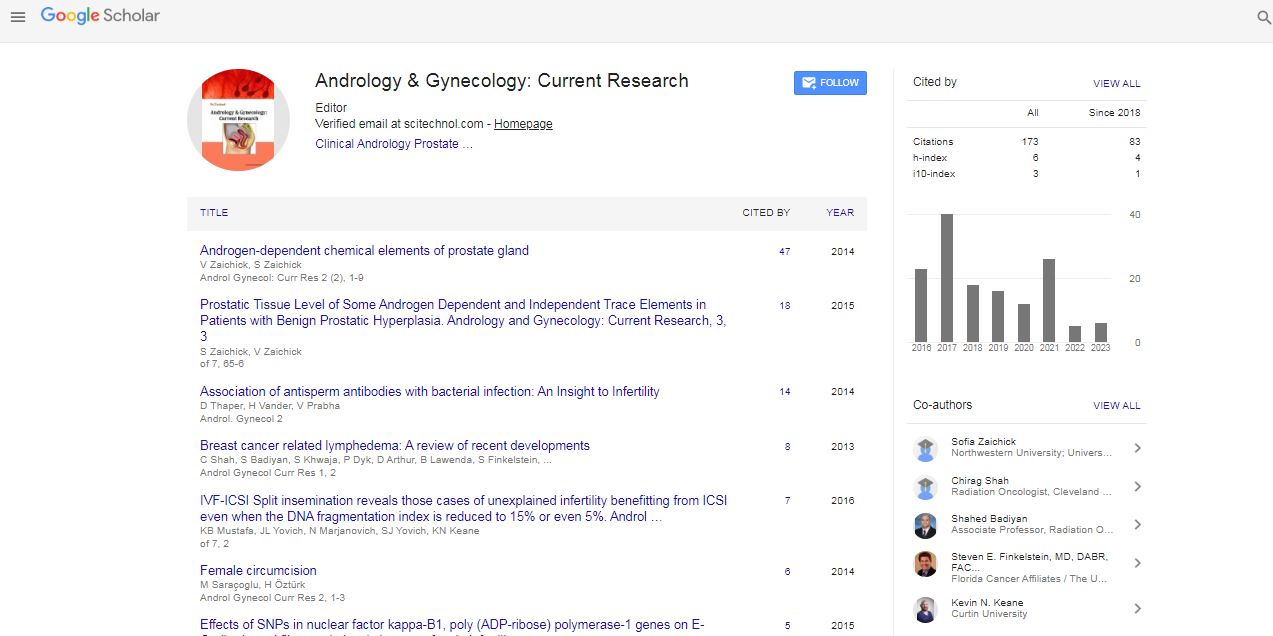
: Androl Gynecol: Curr Res
Abstract
Introduction: There is growing international concern regarding the safety of synthetic mesh pelvic organ prolapse repairs. As such, there is interest in alternatives such as biologics, with the theoretical benefit of improved tissue remodeling with decreased risk of persistent vaginal erosion.
Methods: Using the California (United States) Office of Statewide Health Planning and Development database, we identified all women who underwent inpatient prolapse repair with a graft between 2005- 2011 in California. Billing codes were used to identify subsequent surgeries.
Results: A total of 14,192 women underwent prolapse repair with a biologic (14%) or synthetic graft (86%) with an overall any cause repeat surgery rate of 5.6%. With a median follow-up of 2 years, women with biologic grafts had an increased risk of surgery for recurrent prolapse compared with synthetic mesh (3.6% vs. 2.5%, p=0.01). Conversely, women with synthetic grafts had a higher risk of repeat surgery for a graft complication (3.0% vs. 2.0%, p=0.02). There were no significant differences between the overall risk of repeat surgery in patients who received biologic versus synthetic grafts (5.7% vs. 5.6%, p=0.79).
Conclusion: We demonstrate in a large US populationbased cohort that biologic grafts are associated with an increased risk of repeat surgery for a prolapse recurrence while synthetic mesh is associated with an increased risk of repeat surgery for a complication. These competing risks result in an equivalent overall any cause repeat surgery rate between the groups. This data suggests that neither synthetic nor biologic grafts should be excluded based on this risk profile.
Biography
Rogo-Gupta L completed her MD from the Keck School of Medicine at the University of Southern California, her training in obstetrics and gynecology from Columbia University and subspecialty training in Female Pelvic Medicine and Reconstructive Surgery (Urogynecology) from the University of California, Los Angeles under the mentorship of Dr. Shlomo Raz. She is currently a Clinical Assistant Professor of obstetrics and gynecology and (by courtesy) Urology at Stanford University, serving as the medical director of ambulatory gynecology. She has published over 27 articles in peer-reviewed journals, 57 conference abstracts, seven book chapters and many lectures within and outside the United States.
E-mail: lrgupta@stanford.edu
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi