Case Report, J Liver Disease Transplant Vol: 6 Issue: 2
A Case of Hepatic Artery Thrombosis after Liver Transplantation
Inductivo-Yu II* and Tan RIF
Department of Internal Medicine, National Kidney and Transplant Institute, Philippines
*Corresponding Author : Ira I Inductivo-Yu, M.D
National Kidney and Transplant Institute, Room 3233, Diliman, Quezon City, Philippines
Tel: +63 2 9810300
E-mail: ira_inductivo@yahoo.com
Received: May 15, 2017 Accepted: June 06, 2017 Published: June 13, 2017
Citation: Inductivo-Yu II, Tan RIF (2017) A Case of Hepatic Artery Thrombosis after Liver Transplantation. J Liver Disease Transplant 6:2. doi: 10.4172/2325-9612.1000150
Abstract
Introduction: Hepatic artery thrombosis (HAT) is the most serious vascular complication after liver transplantation. The most common presentation is elevation of liver function tests. When the diagnosis of hepatic arterial thrombosis is established, prompt intervention should be performed.
Case Presentation: In this case report, we present a 37-year-old male with Chronic Hepatitis B infection who underwent a successful liver transplantation, and later developed multiple complications. The most significant of which is hepatic artery thrombosis. He underwent revascularization, supported by heparin and prostaglandin infusion. Succeeding doppler ultrasound surveillance showed patency of right hepatic artery flow.
Conclusion: Early identification of hepatic artery thrombosis should be paid attention after liver transplantation to prevent its complications. Once the diagnosis is established, prompt intervention such as retransplantation or revascularization should be performed.
Keywords: Report; Hepatic artery thrombosis; Liver transplantation; Revascularization
Introduction
Hepatic artery thrombosis (HAT) is the most serious vascular complication after liver transplantation with an overall incidence of 2% to 9%. It is also the most frequent arterial complication in liver transplantation. It represents one of the main causes of graft loss and transplant recipient mortality [1]. The mechanism of HAT development is not fully understood. Liver disease patients are said to be in an unstable rebalanced hemostasis and transplant recipients experience a hypercoagulable state. Several risk factors for developing HAT have been identified. These include previous episode of HAT, number of arterial anastomoses and low donor weight [2].
HAT may either be classified as early hepatic artery thrombosis (E-HAT) when diagnosed within the first 21 days after transplantation and late hepatic artery thrombosis (L-HAT) if diagnosed beyond 21 days after transplantation. L-HAT is generally associated with a milder clinical course with a more insidious onset due to the development of collateral arteries. In a retrospective cohort study in 2014, a total of 102 episodes of HAT were reviewed, 31 episodes (30.4%) were identified as E-HAT, and 71 episodes (69.6%) were identified as L-HAT [2].
Most of the patients who developed HAT presented with increased serum transaminase levels and fever. This may or may not be associated with cholestasis. HAT may present with symptoms such as cholestasis, relapsing bacteremia, liver abscess, biliary tract complications such as stenosis or necrosis and fulminant hepatic failure [2-4]. Differential diagnosis includes primary graft nonfunction and acute severe rejection [5]. In this case report, we present a case of a 37-year-old chronic Hepatitis B with liver cirrhosis, who underwent orthotopic liver transplantation [6]. Perioperatively, he developed several complications including hepatic artery thrombosis.
Case Presentation
The patient is a 37-year-old male with liver cirrhosis secondary to chronic hepatitis B. He has previous admissions as a result of variceal bleeding and hepatic encephalopathy. He has been on treatment with Entecavir for 6 months prior to his liver transplant. Undetectable levels of HBV DNA was documented prior to the procedure.
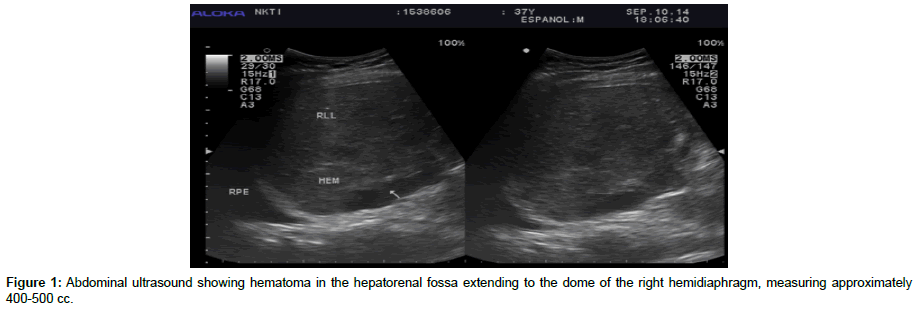
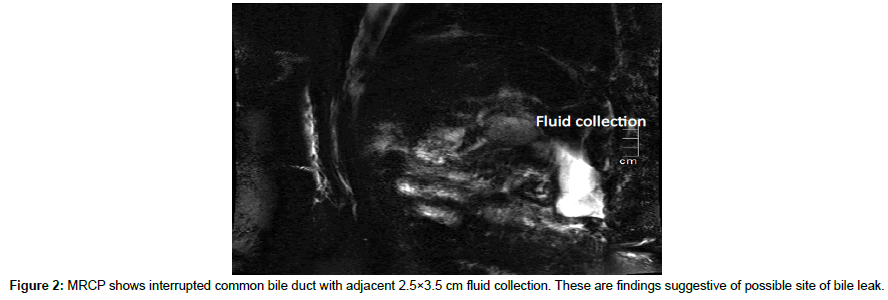
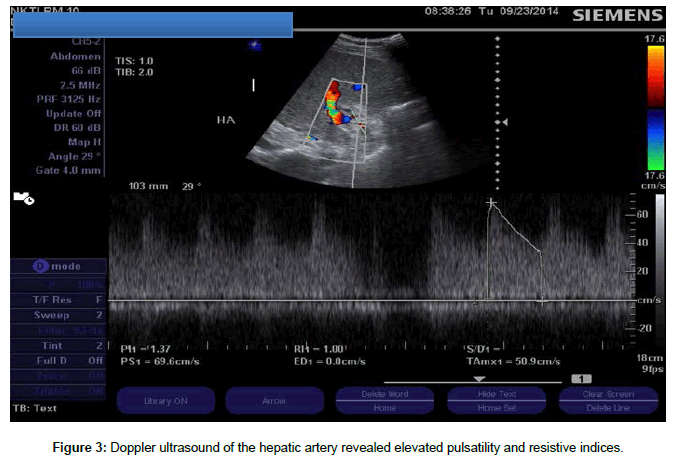
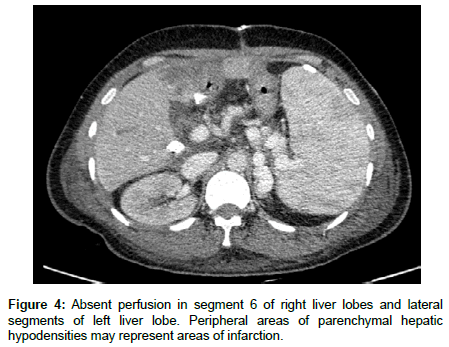
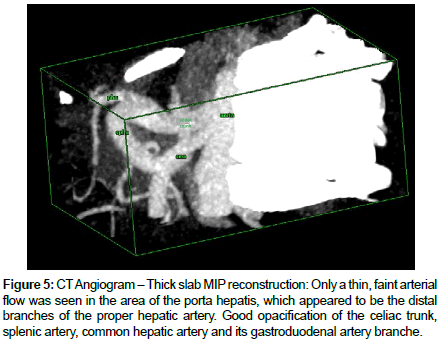
The patient underwent a successful total hepatectomy, orthotopic liver transplant, cadaveric donor. Due to the structural differences among the vessels and the biliary tract of the recipient and the donor, different anastomosis were adapted and are as follows (recipient – donor): 1. Main portal vein- main portal vain; 2. Graft hepatic vein Ostia to the SVC by piggy back technique 3. Right hepatic artery to splenic artery; 4. Left hepatic artery to left gastric artery; 5. Main hepatic duct to proximal common bile duct. Estimated blood loss was 6 liters intra operatively. Because of the portal hypertension and severe coagulopathy pre transplant, multiple blood products were transfused (8 units leukodepleted pRBC, 4 units FFP, and 4 units platelet apheresed). Daily monitoring of liver enzymes and blood chemistries were requested. Hepatitis B Immunoglobulin (HBIg) was administered on a per protocol schedule. Tacrolimus trough was monitored and dose adjustments were done accordingly. Regular evaluation of the transplanted liver and vessel patency was done via doppler ultrasound. During the first postoperative day, abdominal ultrasound revealed an expanding intraabdominal hematoma (Figure 1). Patient underwent emergency re exploration with ligation of bleeders. A total of 1.5 liters of hematoma was evacuated. During this surgery, 3u leukodepleted prbc, 6 u FFP and 6 units platelet concentrate were transfused. On the third week postoperatively, greenish drainage from JP drain was discovered. MRCP revealed biliary leak involving the anterolateral aspect of anastomotic site of the common bile duct (Figure 2). Patient eventually underwent biliary reconstruction. Two days after the biliary reconstruction, the patient’s liver transaminases were noted to be elevated. The SGOT and SGPT values increased from 47 IU and120 IU to 374 IU (8x elevated) and 482 IU (4x elevated) respectively within 2 days post biliary reconstruction. Doppler ultrasound revealed absence of intrahepatic arterial flow and high resistivity indices. (Figure 3) Confirmatory CT angiography was done which revealed right hepatic artery thrombosis (Figures 4 and 5).
Figure 5: CT Angiogram – Thick slab MIP reconstruction: Only a thin, faint arterial flow was seen in the area of the porta hepatis, which appeared to be the distal branches of the proper hepatic artery. Good opacification of the celiac trunk, splenic artery, common hepatic artery and its gastroduodenal artery branche.
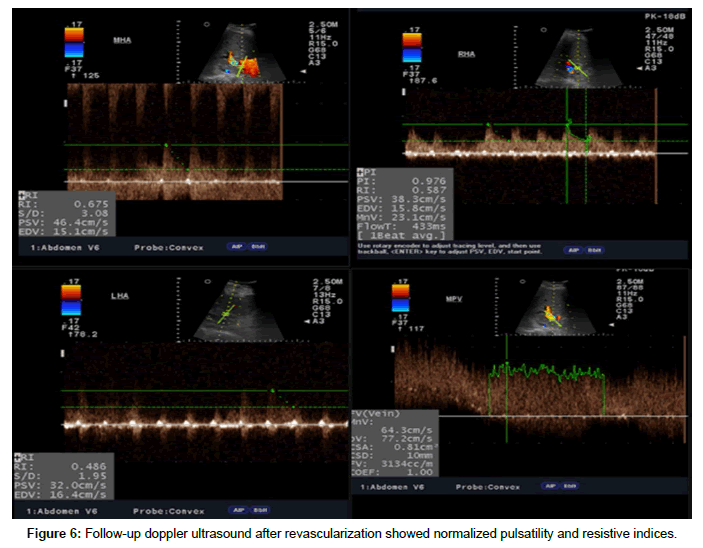
The patient was started immediately on heparin drip. This was titrated and bleeding parameters were closely monitored. The transplant team contemplated on urgent retransplantation; however the unavailability of a liver donor prompted the decision to perform revascularization. The patient underwent emergency exploration and revision of the hepatic artery anastomosis with mesh overlay. After revascularization, heparin drip was resumed and Prostaglandin (Aprostadine ®) infusion was started. Succeeding doppler ultrasonography showed good flow in the hepatic vessels and portal vein (Figure 6). The liver enzymes and liver function tests gradually decreased and normalized. Prostaglandin drip and heparin drip were eventually discontinued after 7 and 11 days respectively with regular Doppler monitoring of the graft vessels. Patient was then maintained on cilostazol for antiplatelet prophylaxis. The patient fully recovered and was eventually discharged. Presently, the patient is maintained on Tacrolimus, Myfortic Acid, Prednisone, Entecavir, and Cilostazole. He is also receiving regular Hepatitis B Immunoglobulin (HepBIg) injections to prevent disease recurrence on the graft. He did not require further rehospitalizations, had regained full functional capacity.
Discussion
Hepatic artery thrombosis after liver transplantation is considered as a devastating event associated with significant morbidity and mortality. HAT usually occurs early in the post-operative period. The clinical presentation of HAT varies. It may present as a mild elevation of serum amino transferase and bilirubin levels to fulminant hepatic necrosis. Late thrombosis may occur after transplantation and is usually associated with bile duct strictures or with recurrent sepsis. In this case, the sudden transaminitis and the bile leakage that necessitated biliary reconstruction were the manifestations of HAT.
It was initially proposed that surgical technique was the most important risk factor for HAT. In our case, the variances in the anatomic structures in the donor and the recipient resulted to an unconventional anastomosis, which increased the risk of developing HAT. Another factor that could have contributed to HAT is the multiple transfusions given during the transplantation and the succeeding re-explorations. The patient was severely coagulopathic necessitating transfusions of different blood products. Factor VII administration could have lessened the bleeding episodes and lowered the transfusion requirements, however, this was not available at the center and the cost is very prohibitive in a developing country like the ours. Increased transfusion requirement for packed RBCs and FFP during surgery was identified as an independently risk factor associated with increased incidence of HAT [7].
An early diagnosis with immediate treatment is the key to proper management of HAT. Routine Doppler ultrasonography was done with the patient to evaluate the vessel patency and identify occlusion or thrombus formation as earliest as possible. Doppler ultrasonography is the initial imaging test in patients in whom HAT is suspected after liver transplantation. It is an inexpensive, portable, and non-invasive technique with a high sensitivity for the detection of HAT. It has the capability of evaluating the patency of the hepatic artery, portal vein, hepatic veins, and inferior cava vein. It could also assess the liver parenchyma, bile ducts, subphrenic and subhepatic spaces, and the possible existence of intra-abdominal fluid collections [4]. CT Angiography is necessary for accurate diagnosis and remains to be the gold standard in the diagnosis of HAT [3,8]. In both imaging studies, the accuracy of the reading is highly dependent on the expertise of the radiologist. Re-transplantation is the gold standard treatment for HAT. Urgent retransplantation in such cases improves the survival rate by 30% to 50% [8]. However this procedure is limited by both organ availability and is highly dependent on the patient’s general condition. Conversely, revascularization can be achieved through arterial reconstruction, surgical thrombectomy, or radiologically guided thrombolysis. Prompt revascularization decreases the incidence of serious, irreversible septic complications and graft loss [1,2,5]. Pharmacological prophylaxis, by the use of antiplatelet or anticoagulant agents, is an important tool to reduce incidence of HAT and prevent graft loss [1]. However, its use in the early postoperative period can be considered hazardous because of the risk of postoperative bleeding owing to the fact that liver transplant recipients often have a severely impaired coagulative function at the time of transplantation. On the other hand, antiplatelet prophylaxis can effectively reduce the incidence of late HAT after liver transplantation, particularly in those patients at risk for this complication. There were no hemorrhagic complications associated with the use of aspirin [1,9,10].
The use of postoperative prophylactic anticoagulation therapy is beneficial in preventing HAT after liver transplantation. Anticoagulation is associated with an improvement in the outcomes mainly when used for high-risk patients. However, bleeding complication can occur with unmonitored use of anticoagulants such as heparin [1,11]. In our case, the risk of ultimately losing graft viability prompted the use of continuous heparin. He was then maintained cilostazol to prevent thrombosis recurrence. The use of prostaglandin in hepatic artery thrombosis has been proposed. However, there is no firm recommendation yet regarding its use. PGE1 is said to ameliorate, or reverse, severe ischemic injury after liver transplantation. The roles of PGE1 in liver transplantation are its cytoprotective effect for the hepatocytes, suppression of the cell-mediated cytotoxicity, and inhibition of cytokine release from activating macrophages and facilitate hepatic regeneration. They also inhibit superoxide anion radical generation from polymorphonuclear leukocytes. Lastly, prostaglandin is considered to be a powerful vasodilator and it inhibits platelet aggregation [12]. In other studies, hepatic arterial infusion of PGE1 appears to be more advantageous in oxygen delivery to the liver compared with intravenous infusion [13]. Prostaglandin hepatic arterial infusion was not attempted since at present, the center lacked the experience for this route of PGE administration. However, continuous PGE intravenous infusion proved successful in maintaining good hepatic arterial flow with no side effects encountered.
Conclusion
The key to the management of hepatic artery thrombosis still lies on early detection. Routine monitoring of liver enzymes and evaluation of hepatic blood flow may be done by Doppler ultrasonography. Once the diagnosis is established, the decision whether to perform retransplantation or revascularization depends on factors such as donor availability, condition of the patient and the duration of time once HAT is identified to intervention. The use of antiplatelets and anticoagulants in preventing HAT after liver transplantation has been established. Further clinical studies and recommendations on the use of prostaglandin in HAT are needed.
References
- Abdullah AA, Moustafa MM, Simon RB (2015) Anticoagulation and antiplatelets as prophylaxis for hepatic artery thrombosis after liver transplantation. World J Hepatol 7: 1238-1243.
- Mourad M, Liossis C, Gunson B, Mergental H, Isaac J, et al. (2014) Etiology and management of hepatic artery thrombosis after adult liver transplantation. Liver Transpl 20: 713-23.
- Proposito D, Segurola CL, Garcìa IG, Jimènez C, Pinto IGL, et al. (2000) Diagnosis and treatment of hepatic artery thrombosis after liver transplantation. Chir Ital 52: 505-525.
- Stange B, Glanemann M, Nuessler N, Settmacher U, Steinmuller T, et al. (2003) Hepatic Artery Thrombosis After Adult Liver Transplantation. Liver Transpl 9: 612-620.
- Tzakis A, Gordon R, Shaw W, Iwatsuki S, Starzl T (1985) Clinical Presentation Of Hepatic Artery Thrombosis After Liver Transplantation In The Cyclosporine Era. Transplantation 40: 667-671.
- Silva M, Jambulingam P, Gunson B, Mayer D, Buckels JA, et al. (2006) Hepatic Artery Thrombosis Following Orthotopic Liver Transplantation: A 10-Year Experience From a Single Centre in United Kingdom. Liver Transpl 12: 146-151.
- Yi Yang, Zhao J, Yan LN, Ma YK, Huang B, et al. (2014) Risk Factors Associated with Early and Late HAT after Adult Liver Transplantation. World J Gastroenterol 20: 10545-10552.
- Angeles García Criado, Rosa Gilabert, Carlos Nicolau, Isabel Real, Pedro Arguis, et al. (2001) Early Detection of Hepatic Artery Thrombosis After Liver Transplantation by Doppler Ultrasonography. J Ultrasound Med 20: 51-58.
- Shay R, Taber D, Pilch N, Meadows H, Tischer S, McGillicuddy J, et al. (2013) Early aspirin therapy may reduce hepatic artery thrombosis in liver transplantation. Transplant Proc 45: 330-334.
- Vivarelli M, Barba G, Cuchetti A, Lauro A, Del Gaudio M, et al. (2007) Can antiplatelet prophylaxis reduce the incidence of hepatic artery thrombosis after liver transplantation? Liver Transpl 13: 651-654.
- Khalid A Abou Ella, Mohamed I Al Sebayel, Carlo B Ramirez, Hussien M Rabea (2001) Hepatic artery thrombosis after orthotopic liver transplantation. Saudi Medical Journal 22: 211-214.
- Takaya S, Doyle H, Todo S, Irish W, Fung JJ, et al. (1995) Reduction of Primary Nonfunction With Prostaglandin E1 after clinical Liver Transplantation. Transplanta Proc 27: 1862-1867.
- Kato T, Sato T, Kurokawa T, Najo H, Asanuma Y, et al. (2003) Efficacy of continuous infusion of prostaglandin E1 through the superior mesenteric artery against ischemic liver cell necrosis after hepatic artery occlusion. Transplantation 76: 1340-1345.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi