Case Report, Int J Ophthalmic Pathol Vol: 7 Issue: 3
A Case of Retinal Dysplasia, Misdiagnosed as Retinoblastoma
Yusra Shafique*, Rubina Gulzar, Ruqaiya Shahid and Farheen Danish
Department of Pathology, 2nd Floor, Dow International Medical College, Dow University of Health Sciences, Karachi, Pakistan
*Corresponding Author : Yusra Shafique
Department of Pathology, 2nd Floor, Dow International Medical College, Dow University of Health Sciences, Karachi, Pakistan
E-mail: memon.yusra@hotmail.com
Received: October 15, 2018 Accepted: November 23, 2018 Published: November 30, 2018
Citation: Shafique Y, Gulzar R, Shahid R, Danish F (2018) A Case of Retinal Dysplasia, Misdiagnosed as Retinoblastoma. Int J Ophthalmic Pathol 7:3. doi: 10.4172/2324-8599.1000227
Abstract
Background: Retinal dysplasia is a congenital ocular pathology that can mimic as retinoblastoma caused by abnormal proliferation of retinal tissue.
Objective: To present a case of retinal dysplasia misdiagnosed clinically as retinoblastoma and underwent enucleation surgery.
Result: A 7 years old female underwent enucleation surgery as she was diagnosed clinically as retinoblastoma. Both of them could present with leucocoria and histologically can show rossettes formation. It is important to differentiate both these entities inorder to avoid enucleation in case of retinal dysplasia.
Keywords: Retinal dysplasia; Leucocoria; Retinoblastoma
Introduction
Retinal dysplasia is a rare cause of childhood leucocoria and close differential diagnoses of retinoblastoma. It is difficult to differentiate retinal dysplasia from many benign and malignant ocular pathologies. Enucleation of retinal dysplasia could be avoided if patient is thoroughly investigated before enucleation.
Case Report
Retinal dysplasia, misdiagnosed as retinoblastoma
A seven years old female presented with a history of unilateral red eye noticed by parents since she was 5 months old and decreased vision. Ocular examination was done of the siblings which was normal. Ophthalmologist noted leukocoria in right eye. Ophthalmic examination under general anaesthesia revealed a yellowish white retrolental mass. Left eye was normal on ophthalmic examination. MRI was not performed. Right eye was enucleated following diagnosis of retinoblastoma and specimen was sent for histopathology.
Gross findings
The gross examination showed eyeball measuring 2.5 × 2.5 × 2 cm. Optic nerve stump measuring 0.3 × 0.3 cm. On sectioning cut surface showed a greyish white area measuring 1.8 × 1 cm in the anterior vitreous, behind the lens; anterior chamber and ciliary body were unaffected. Retina was detached.
Microscopic findings
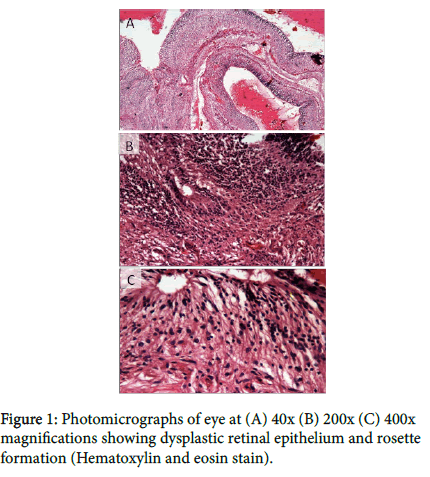
The microscopic examination showed full thickness sections of eyeball with intact anterior and posterior chambers. Retrolental area showed whorls of disorganized, folded and proliferating retinal epithelium. Stroma of disorganized epithelium showed normal glial tissue and many tubular rosettes around the central empty spaces surrounded by peripheral rows of elongated, evenly arranged nuclei. Cells showed uniform rounded nuclei with speckled chromatin, scanty cytoplasm and indistinct cell borders. No nuclear atypia was noted. No atypical mitosis, necrosis or calcification is seen. Ciliary body was surrounded on either side by inflammatory exudate comprising of fibroblasts, proliferating capillaries and inflammatory infiltrate. Optic nerve stump showed nerve fibers and no tumor cells were seen (Figure 1).
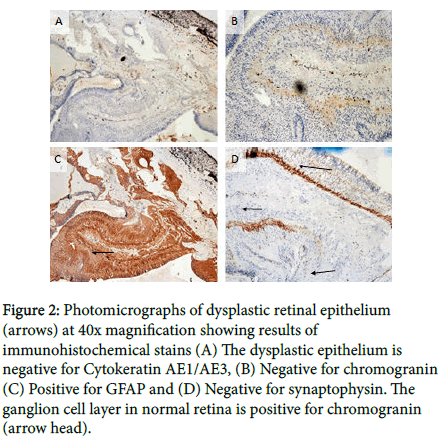
A panel of immunohistochemical stains was performed, Glial Fibrillary Acidic Protein (GFAP) highlighted the glial tissue; chromogranin and synaptophysin were negative in disorganized retinal epithelium. These stains are positive in retinoblastoma (Figure 2) [1]. The diagnosis of retinal dysplasia with retinal detachment was made.
Figure 2: Photomicrographs of dysplastic retinal epithelium (arrows) at 40x magnification showing results of immunohistochemical stains (A) The dysplastic epithelium is negative for Cytokeratin AE1/AE3, (B) Negative for chromogranin (C) Positive for GFAP and (D) Negative for synaptophysin. The ganglion cell layer in normal retina is positive for chromogranin (arrow head).
Discussion
The normal histology of the retina is characterized by the ordered orientation of cells forming a multilayered tissue. On the vitreal surface it is lined by retinal ganglion cells and on scleral surface by retinal pigment epithelium. These two layers establish the polarity of other layers [2]. When this normal orderly arrangement of the retina is disrupted it leads to retinal dysplasia. The term “retinal dysplasia” was first described by Reese and Blodi in 1950 [3]. Bilateral retinal dysplasia is a part of congenital syndrome combining retinal abnormalities with systemic anomalies affecting central nervous system, heart, extremities and other organs. These disorders include Norrie disease, Trisomy 13, Holoprosencephaly and Walker- Warburg syndrome. Unilateral retinal dysplasia is usually not associated with any congenital syndrome [2-5].
Clinically, retinal dysplasia may present itself in a wide range of severity from simple to massive folding of the retina, the central stalks with the retinal tissue extending from the optic disc to the back of the lens and complete retinal detachment, leading to highly disorganized microphthalamic eyes. If the intraocular proliferation is large enough, it may produce leukocoria. Leukocoria that is white reflection from retina can be caused by other lesions beside retinal dysplasia. These include retinoblastoma, persistent hyperplastic primary vitreous, Coats disease, retinocytoma and congenital cataract. Retinal dysplasia is a rare cause of leukocoria [2,6].
Among these the close differential diagnosis of retinal dysplasia is retinoblastoma as the primary histological feature in both is rosette formation. The rosette formation in retinal dysplasia represents an attempt to form embryonic retinal tissue rods and cones. The cells lining the rosettes in retinal dysplasia are uniform, bland and similar to the nuclei lining the outer limiting membrane of the retina. The malignant Flexner-Wintersteiner rosettes which are formed in retinoblastoma are characterized by malignant cells having all the cytological features of anaplasia that are typically associated with malignant neoplasms. On the other hand, the rosettes which are seen in retinal dysplasia also show analogous differentiation which simulates the photoreceptor elements but they are of course, not malignant [7] and they contain multiple cell types. The outer nuclear layer is present centrally and the lumen is lined by outer limiting membrane and the inner nuclear layer is present peripherally [8]. Dysplastic rosettes represent a developmental or embryopathic aberration rather than a true neoplastic aberration.
The rosettes in retinoblastoma are typically positive for Immunohistochemical stain cone opsin and are negative for rod opsin. The dysplastic rosettes show the opposite pattern which mainly expresses rod opsin [6]. Also, muller cell differentiation is not observed in the rosettes of retinoblastoma. In addition to the formation of rosettes, retinal dysplasia occasionally shows an attempt by the faulty neuroepithelium to form a simple cuboidal epithelium resembling that of the embryonic retina or the ciliary body.
Conclusion
The differentiating features of retinal dysplasia from other differential diagnoses are that Coats disease shows cholesterol clefts; fibrovascular cores are observed in persistent hyperplastic vitreous and Retinocytoma has numerous rossettes [9]. Leukocoria and retinal detachment in children require a prompt investigation because retinoblastoma should be differentiated from other non-tumorous conditions as the prognosis and treatment options are different. Usually the underlying disease which causes leukocoria can be detected by ophthalmoscopy alone or in combination with ultrasonography. The dysplastic retinal tissue is a rare congenital defect and may create a clinical and radiological picture of an intraocular mass which closely resembles tumor tissue. The awareness of this disease and its histopathological features are therefore helpful in differentiating between retinal dysplasia and malignant ocular pathology, so as to reach an early diagnosis.
References
- Kivelä T, Tarkkanen A, Virtanen I (1989) Synaptophysin in the human retina and retinoblastoma. An immunohistochemical and Western blotting study. Invest Ophthalmol Vis Sci 30: 212-219.
- Agarwal N, Gupta P, Agarwal A, Pantola C (2011) Retinal Dysplasia–A Mimic of Malignant Ocular Pathology. J Clin Diag Res 5: 367-368.
- Reese AB, Blodi FC (1951) Retrolental Fibroplasia: The Fifth Francis I. Proctor Lecture. Am J Ophthalmol 34:1-24.
- Lloyd I, Colley A, Tullo A, Bonshek R (1993) Dominantly inherited unilateral retinal dysplasia. Br J Ophthalmol 77: 378.
- Lambert NG, Mamalis N, Patel BC, Ramasubramanian A (2015) Unilateral retinal dysplasia mimicking retinoblastoma. J Pediatr 167: 1449
- Ravikumar H (2012) Retinal Dysplasia Mimicking Retinoblastoma. Online J Health Allied Sci 11.
- Jakobiec FA, Zakka FR, D'Amato R, DeAngelis MM, Walton DS, et al. (2011) Unilateral sporadic retinal dysplasia: results of histopathologic, immunohistochemical, chromosomal, genetic, and VEGF-A analyses. J AAPOS 15: 579-586.
- De Graaf P, Van der Valk P, Moll A, Imhof S, Schouten-van Meeteren A, et al. (2007) Retinal dysplasia mimicking intraocular tumor: MR imaging findings with histopathologic correlation. AJNR Am J Neuroradiol 28:1731-1733.
- Prasanna M, Kwatra K, Calton N, Thomas S (2013) Retinal dysplasia mimicking retinoblastoma. Ind J Pathol Microbiol 56: 64-65
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi