Research Article, J Clin Exp Oncol Vol: 11 Issue: 1
A Case Study: Pallative Radical Mastectomy with Latissimus Dorsi Flap Reconstruction
Bachu Brahmani* and Avinassh Tippani
Department of Oncology, Sai shree hospitals cancer and surgical gastro centre, Warangal, India
*Corresponding Author: Bachu Brahmani
Department of Oncology, Sai shree
hospitals cancer and surgical gastro centre, Warangal, India,
Tel: 7674909951;
Email: bhuvana.rockers@gmail.com
Received date: 27 September 2021, Manuscript No: JCEOG-21-30598;
Editor Assigned: 29 October 2021, PreQC No: JCEOG-21-30598 (PQ);
Reviewed Date: 12 November 2021, QC No: JCEOG-21-30598;
Revised Date: 26 November 2021, Revised Manuscript No: JCEOG-21-30598 (R);
Accepted Date: 27 January 2022, DOI: 10.4172/2324-9110.11.1.289
Citation: Brahmani B and Tippani A (2022) A Case Study: Pallative Radical Mastectomy with Latissimus Dorsi Flap Reconstruction. J Clin Exp Oncol 11:1.
Abstract
Breast cancer has ranked number one among Indian females with age adjusted rate as high as 25.8/100,000 women and mortality is 12.7/100,000 women, with 25% to 30% presenting with Locally Advanced Breast Cancer (LABC). Toilet Mastectomy is an excellent adjunct to palliative care in Advanced Breast Cancer patients. This is useful for both a proper decrease (debulking) in the tumor cell load and in controlling a recurrent necrotic and/or fungating disease. Here, we share our experience with a patient presenting with MBC and complaining of a recurrent breast fungating disease, aiming to highlight the importance of palliative surgical treatment in systemic breast malignancy.
Keywords: Toilet mastectomy; Fungative breast; Breast Cancer; Palliative Radical Mastectomy; LD Flap Reconstruction.
Introduction
Breast cancer is still the most common malignancy in women. Though management of local disease has been thoroughly studied, management of Locally Advanced Breast Cancer (LABC) is still under much debate. With 1.3 million new cases and almost half a million deaths annually worldwide, breast cancer is one of the most challenging malignancy [1]. Breast cancer has ranked number one among Indian females with age adjusted rate as high as 25.8/100,000 women and mortality is 12.7/100,000 women, with 25% to 30% presenting with Locally Advanced Breast Cancer (LABC) [2-3].
However, survival of patients with LABC is steadily improving [4], with a decrease of the risk of death by 1–2% yearly [5].
Locally advanced breast cancer, is a sub category of breast cancers that usually present with large fungating growth tumors with regional lymphadenopathy, and direct extension of the tumor to the chest wall and/or skin, in the absence of distant metastasis [6]. Fungating malignant lesions are a subclass with ulcerative and necrotic characteristics which manifest with pain, disfigurement, hemorrhage, odor, and infections [7-10].
Surgery is the main stage for LABC with NACT followed by. Toilet Mastectomy is an excellent adjunct to palliative care in Advanced Breast Cancer patients. This is useful for both a proper decrease (debulking) in the tumor cell load and in controlling a recurrent necrotic and/or fungating disease [11-12]. The aim of palliative care is to improve the quality of life and make the subject as comfortable as possible.
Here, we share our experience with a patient presenting with LABC and complaining of a breast fungating disease, aiming to highlight the importance of palliative surgical treatment in systemic breast malignancy. LABC is NACT followed by surgery and Radio therapy. A subset of patients where NACT does not show response tumor program is a challenging situation.
Case Summary
A young female patient of age 33years presented with large fungating right breast mass with foul smell and discharge.
CT scan of the Chest with Contrast revealed
1.Large irregular heterogeneously enhancing necrotic exophytic right breast mass causing deep ulceration.
2.Multiple Necrotic nodules and mass lesion involving at right axilla. Metastatic nodes are formed.
CT scan of abdomen and pelvis (Plain & Contrast) is normal.
Histopathological examination
On gross examination Breast mass measuring 14.5×13.6×5.8 cm covered with a skin flap measuring 10.5×10 cm. Externally the skin flap shows a large ulcerated area measuring 10.5×8 cm. Nipple areola identified separately from ulcerated area. Distance of nipple from ulcerated area is 0.8 cm. Cut surface shows a lesion, which is a firm breast mass at right side measuring 8.6×6.5×5.2 cm grey white, with occasional hemorrhagic areas is seen.
Level ll/lll axillary lymph nodes contain globular mass measuring 6.5×5×4 cm. A cyst wall infiltration contains grey white-grey brown soft tissue measuring 2.5×2×0.3 cm.
Microscopic examination shows extensive areas of necrosis with viable lesion predominantly composed of large polygonal cells arranged around the vessels. There is marked nuclear pleomorphism. Lobules of cartilage with atypical cells are seen in lacunae. Level II/III axillary lymphnode shows metastatic tumor deposits and Chest wall shows involvement of tumor. Histopathology report reveals Metaplastic Carcinoma with Chondrosarcomatous Differentiation-ypT4cN3aMx of right breast.
Histological grade
Nottingham Histologic score- Tubule differentiation-3
-Nuclear pleomorphism-3
-Mitosis figure -3
Total score -9
SBR grade III
Tumor focality- Unifocal
Margins- separately sent superor & inferior margins including posterior surface are uninvolved
Treatment effect in lymphnode- No definite response ion presurgical therapy in metastatic carcinoma
Lymphovascular emboli- Present
Extranodal extension- Present
Pathologic staging (pTNM)
Primary tumor- ypT4c
Regional lymph nodes- ypN3a (metastasis to level III axillary lymphnode)
Distant Metastasis – ypMx
Immuno Histo Chemistry (IHC) report
ER—Negative
PR—Negative
Her2neu—Negative
She was evaluated outside at a private hospital, where she was diagnosed as a Carcinoma of Breast and a trail of 2 cycles of NACT chemotherapy treatment given which showed progression of disease and patient was planned for supportive palliative care. In view of young age of patient a palliative definitive Toilet Mastectomy was done after taking informed consent of patient and patient attendars, to increase the survival rate and give a benefit of core. Toilet Mastectomy was done with level I to III lymphnode dissection. The raw area was closed with LD flap reconstruction.
Post operatively, patient recovered well and discharged. Further patient was given 8 cycles of Adjuvant chemotherapy treatment followed by 50gy of radiation to extra chest wall and supra clavicular area. After 3years of survival and follow up, patient is doing well.

Figure 1: Pre-operative image showing ulcerative fungative breast mass.
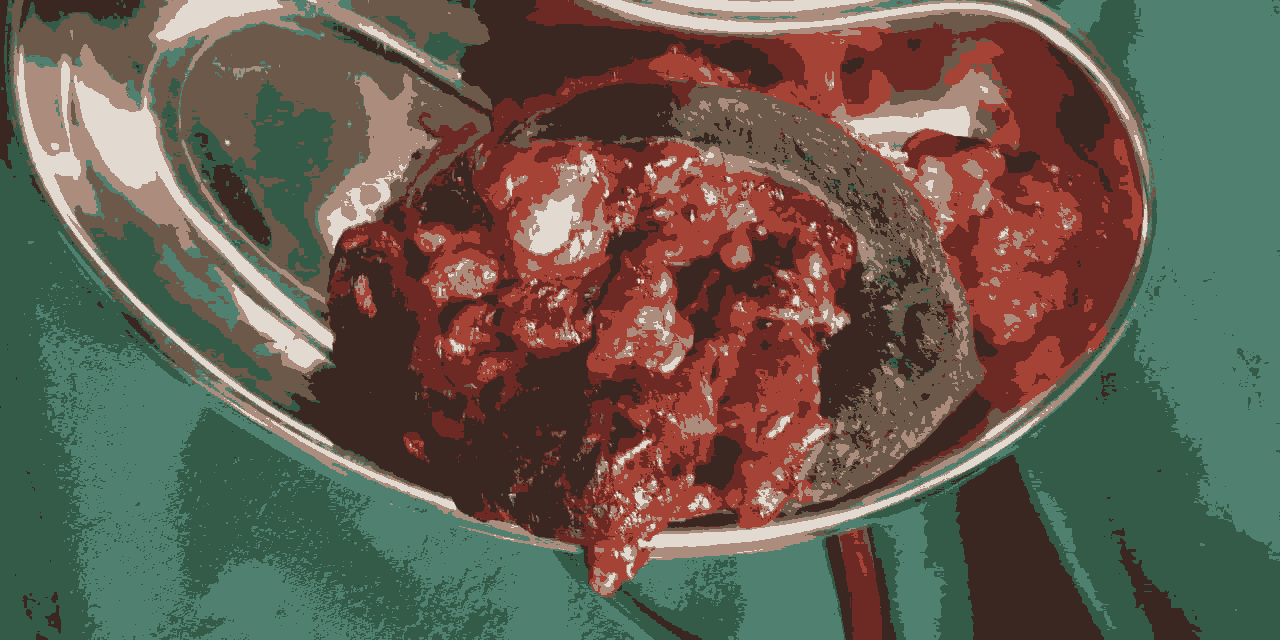
Figure 2: Showing breast mass after surgery.
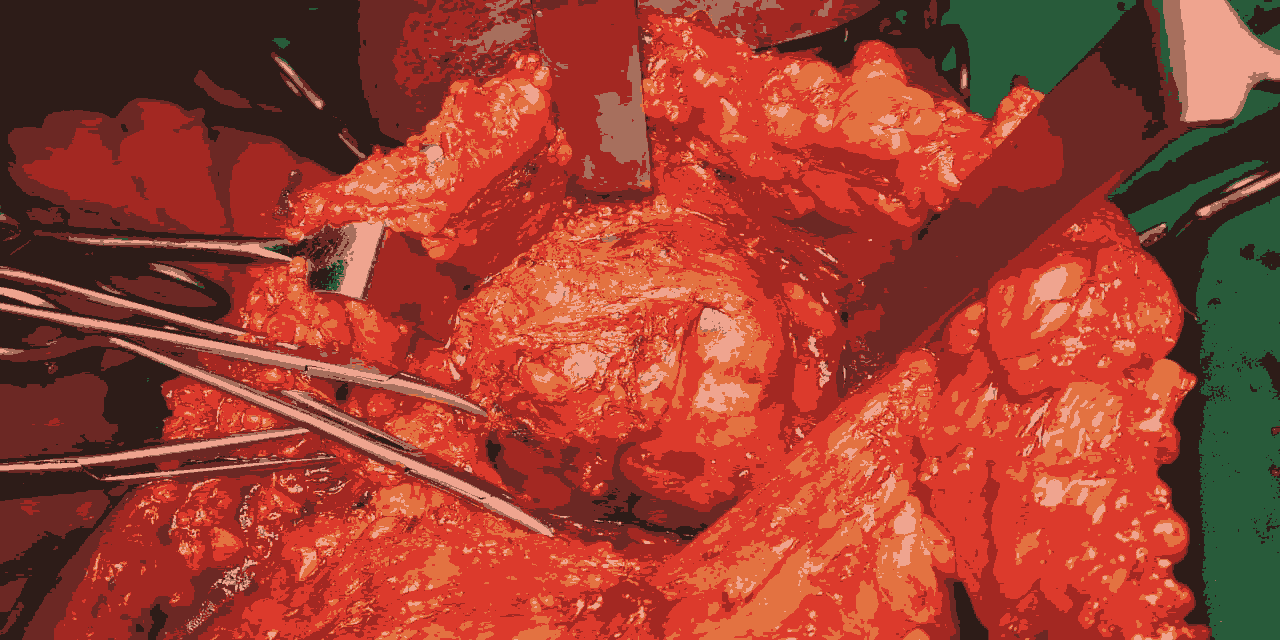
Figure 3: Intra operative image showing the Axillary lymphnode.
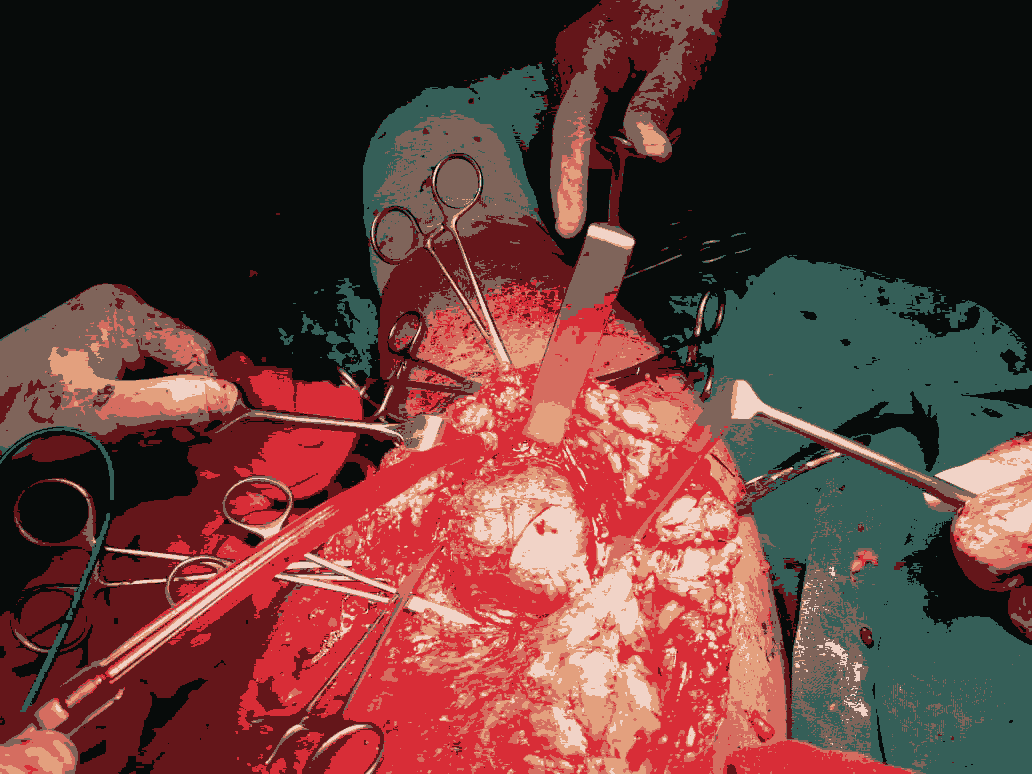
Figure 4: Intra operative image showing the Axillary lymphnode.

Figure 5: Shows raw area after lymphnode dissection.

Figure 6: Shows large Axillary lymphnode mass.
Conclusion
Based on the survival rate of greater than 3 years, a subset of young patients can be planned for palliative radical mastectomy with LD flap reconstruction.
References
- Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, et al. (2018) GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68:394-424.
[Crossref] [Google Scholar] [Indexed]
- Malvia S, Bagadi SA, Dubey US, Saxena S (2017) Epidemiology of breast cancer in Indian women. Asia Pac J Clin Oncol 13:289â??295.
[Crossref] [Google Scholar] [Indexed]
- Valero VV, Buzdar AU, Hortobagyi GN (1996) Locally advanced breast cancer. Oncologist 1:8â??17.
[Crossref] [Google Scholar] [Indexed]
- Andre F, Slimane K, Bachelot T (2004) Breast cancer with synchronous metasÂtases: Trends in survival during a 14-year period. J ClinOncol 22: 3302â??3308.
[Crossref] [Google Scholar] [Indexed]
- Giordano SH, Buzdar AU, Smith TL (2004) Is breast cancer survival improvÂing? Cancer 100: 44â??52.
[Crossref] [Google Scholar] [Indexed]
- Garg PK, Prakash G (2015) Current definition of locally advanced breast cancer. Curr Oncol 22:409-410.
[Crossref] [Google Scholar] [Indexed]
- Merz T, Klein C, Uebach B, Kern M, Ostgathe C, et al. (2011) Fungating wounds multidimensional challenge in palliative care. Breast Care 6:21-24.
[Crossref] [Google Scholar] [Indexed]
- Halverson KJ, Taylor ME, Perez CA, Myerson R, Philpott G, et al. (1993) Survival following breastâ??conserving surgery and irradiation or modified radical mastectomy in patients with invasive breast cancers with a maximum diameter of 1 cm. Mo Med 90:759â??63.
- Halsted CP, Benson JR, Jatoi I (2014) A historical account of breast cancer surgery: Beware of local recurrence but be not radical. Future Oncol 10:1649â??57.
[Crossref] [Google Scholar] [Indexed]
- Delpech Y, Barranger E (2013) Breast cancer surgery. Rev Prat 63:1395â??9.
- Charles-Brunicardi F (2010) Schwartz's Principles of Surgery (9th edtn). Mc-Graw Hill: 17.
- Fischer JE (2007) Mastery of Surgery (5th edtn). Lippincott Williams & Wilkins. Chapter 41-46A.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi 



