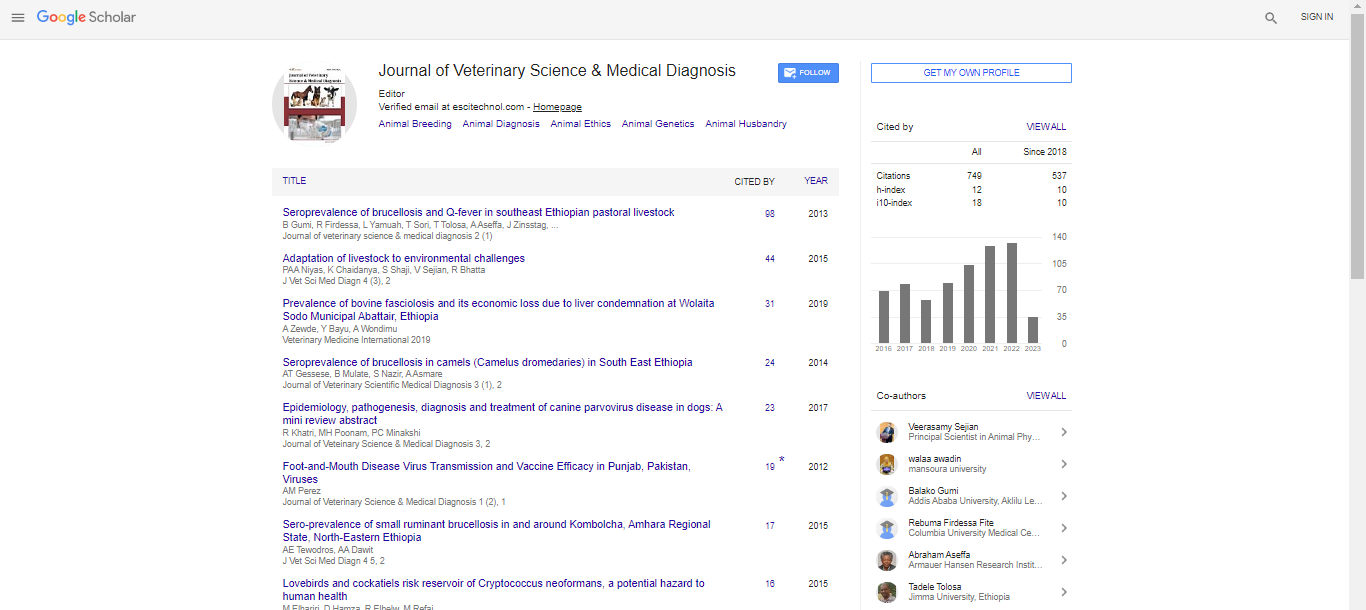
Review Article, J Vet Sci Med Diagn Vol: 11 Issue: 7
A Comparative Study on Different Combinations of Cryoprotectants in Vitrification of Mammalian Oocyte: A Review
Batool Sanaei*, Solmaz Allahverdi Meygooni, Mahsa Nejati and Fatemeh Bashirian Alvares
Department of Molecular and Cellular Biology, University of Science and culture, Tehran, Iran
*Corresponding Author: Batool Sanaei, Department of Molecular and Cellular Biology, University of Science and culture, Tehran, Iran; E-mail: b.sanaei91@gmail.com
Received date: 01 April, 2022, JVSMD-22-56847;
Editor assigned date: 04 April, 2022, PreQC No. JVSMD-22-56847 (PQ);
Reviewed date: 18 April, 2022, QC No. JVSMD-22-56847;
Revised date: 31 May, 2022, Manuscript No. JVSMD-22-56847 (R);
Published date: 07 June, DOI: 10.4172/2325-9590.11.3.019
Citation: Sanaei B, Meygooni SA, Nejati M, Alvares FB (2022) A Comparative Study on Different Combinations of Cryoprotectants in Vitrification of Mammalian Oocyte: A Review. J Vet Sci Med Diagn 11:7.
Abstract
Oocyte cryopreservation is now widely used in Assisted Reproductive Technology (ART). Vitrification of oocyte is now considered to be an efficacious method for eligible patients who want to preserve their fertility for medical and nonmedical indications. However, oocyte vitrification has been facing its own challenges due to the unique structure of oocyte. A successful vitrification program relies on the proper type and combination of cryoprotectants. This review summarizes the results of several existing literature on mammalian oocyte vitrification and post-thaw oocyte development with the main focus on different combinations of cryoprotectants. We aim to compare the effectiveness of various cryoprotectants and to introduce optimal combination of multiple cryoprotectants in vitrification media of mammalian oocyte. Lastly, main properties of permeable and impermeable cryoprotective agents are briefly discussed by highlighting their advantages and disadvantages.
Keywords: Vitrification; Oocyte; Cryoprotectant; Development
Introduction
Fertility preservation is one of the most important and fast-growing area of assisted reproductive technology. The ability to cryopreserve oocyte could make a significant contribution to female fertility preservation in patients undergoing surgery, chemotherapy, or radiotherapy [1-4]. Oocyte cryopreservation is a valuable option for women who tend to delay childbearing [5,6] and patients that suffer from ovarian endometriosis [7], premature ovarian failure, autoimmune or hematologic disorders and gynecological diseases [8]. This technology may also eliminate religious, ethical, legal and moral concerns of embryo freezing [9]. It has been an applicable option for singles and those who are not pleasant to have sperm donation [10]. Moreover, successful oocyte cryopreservation has allowed for the establishment of egg bank and egg donation procedure [11]. In spite of the aforementioned benefits and progressively improved clinical outcomes, there are still several concerns about oocyte freezing. This is due to the specific structure (i.e., large size, low surface to volume ratio, high water content, etc.) and extremely high sensitivity of oocyte to chilling injury [12]. Regarding the unique properties, oocyte is especially vulnerable to physical damages induced by freezing procedure such as intracellular ice formation, solution effects and osmotic shock. Chilling injury, the main concern of successful oocyte cryopreservation, could increase several structural and functional disorders such as depolymerization of microtubules, meiotic spindle disorganization [13-15], chromosome abnormalities [15-17], as well as mitochondrial dysfunction and oxidative stress [18-20]. During cryopreservation, Cryoprotective Agents (CPAs) creates a transient intracellular calcium rise in oocytes which causes premature release of cortical granules, zona hardening and parthenogenetic activation. Hardening of zona pellucida compromise the ability of oocyte to undergo normal fertilization and pre-implantation development. Despite the great progress in the field of cryopreservation, oocyte freezing has been remained a challenging issue. To date, several attempts have been made to improve oocyte cryopreservation protocols which include alteration in equilibration time and temperature, different times of vitrification solutions, use and optimization of various penetrating and non-penetrating CPAs and their combinations, as well as application of various freezing containers that can impact cooling and warming rates. Nonetheless, a standardized freezing procedure for oocyte vitrification has not yet been established. The main concern of vitrification is the cytotoxicity of the high CPA concentration. Since a high concentration of one CPA is extremely cytotoxic, vitrification usually uses a combination of two or more penetrating CPAs to reduce the toxicity of each cryoprotectant. In this review we aim to investigate different combinations of CPAs regarding the outcomes of embryo development and oocyte quality after vitrification. We attempt to introduce an optimized cryoprotectant combination by comparing the results of recent practices in oocyte vitrification. This study also describes main properties and applications of permeating and non-permeating CPAs along with the mechanism by which a cryoprotectant can reduce oocyte injury during cooling-warming process. Further, the principles of cryoinjury and mechanism of cryoprotection will be reviewed in detail.
Literature Review
Cryopreservation techniques
There are two main methods applied to oocyte cryopreservation: slow freezing and vitrification. In slow freezing that relies on the low concentration of CPAs, the temperature is gradually lowered in a stepwise programmed manner (about 2°C/min). This technique is associated with lower toxicity. However, it may lead to cell injury due to intracellular ice crystal formation. In contrast, during vitrification, oocyte exposes to high concentration of CPAs and extremely rapid cooling/ warming rates, which can eliminate intracellular ice formation and chilling injury. This novel technique which involves a vitreous or glasslike solidification- has improved pregnancy, fertilization and implantation rates of post-thaw oocytes, providing excellent clinical outcomes. Different varieties of devices such as Closed Pulled Straw (CPS), Open Pulled Straw (OPS), conventional straws, Electron Microscopy (EM) grids and newly made automatic vitrification device have also been used to obtain relatively high cooling/warming rates during freezing procedure.
Cryoprotectants
Principles and cryoprotection mechanism
All efficient freezing methods must prevent three main obstacles to achieve successful cryopreservation: ice crystal formation, solution effects and osmotic shock. In order to accomplish this, a variety of permeating and non-permeating cryoprotectants have been used for oocyte vitrification. CPAs are basically high water soluble chemical compounds which protect cells against any damage known as "cold shock" during freezing and warming. These chemical compounds are mainly divided into two categories, permeating (intracellular) and non-permeating (extracellular) cryoprotectants. Permeating CPAs-the major ingredients of vitrification solutions- are small molecules that can easily penetrate the cell membrane, and they include Dimethyl Sulfoxide (DMSO), Glycerol (GLY), propylene glycol (PG; 1,2-propanediol; PROH), Ethylene Glycol (EG), acetamide, adonitol and Formamide (FMD). The main role of these CPAs is to reduce ice crystal formation by interfering with hydrogen bonding between water molecules. At low concentrations, they reduce the freezing point of aqueous solutions. However, high concentrations of these CPAs induce a glass-like solidification state bypassing ice crystal formation. Cytotoxicity imposed by high concentration of permeating cryoprotectants has been described as the major obstacle to achieve successful vitrification. In comparison with permeating CPAs, non-permeating CPAs are large molecules, usually bio-macromolecules that provide extracellular protection only. They act by dehydrating intracellular space and consequently inhibition of ice formation during freezing procedure. The most commonly used non-permeating CPAs are mono-saccharides (such as xylose, glucose and galactose), disaccharides (such as sucrose, lactose and trehalose), polysaccharides (such as raffinose, hydroxyl ethylene starch and maltodextrin), proteins (such as albumin and Polyvinylpyrrolidone (PVP)), Polyethylene Glycol (PEG) and mannitol. Since these ingredients are usually less toxic than their penetrating counterparts at the same concentration, overall toxicity would be reduced by combining with permeating CPAs. This also increases the net concentration of permeating CPAs in intracellular space and further assist in preventing ice growth. During the warming, an increase in extracellular water can decrease osmotic pressure, leading to water influx into the cell and swelling, or even rupture of the cell. Therefore, addition of these non-toxic carbohydrates or bio-macromolecules, would help to maintain an equilibrium osmolarity during freezing/thawing process.
Toxicity
Understanding the mechanisms of oocyte chilling injury and cryoprotectant toxicity may lead to development of more efficient and reliable methods for cryopreservation. Also, knowing the precise protective mechanism of cryopreservation could be an important step toward discovering optimal combination of CPAs and reducing cryoprotectant associated freezing injury. Chilling injury refers to physical stress induced by abrupt reduction in temperature during cooling procedure which can lead to water-to-ice phase transition and ice crystal formation. Density of water at solid state (ice) is less than liquid, causing an increase in volume and consequently damage to intracellular organelles. Oocyte is highly sensitive to freezing damages due to the high content of water and its specific structure. During cryopreservation, protection of cell from freeze injury can clearly be achieved by using CPAs beside an optimum cooling/ warming rates. High concentrations of penetrating CPAs present in vitrification solutions reduces the formation of intracellular and extracellular ice, and thereby suppress the oocyte damages. However, the toxic effects caused by these concentrated CPAs are problematic. The developmental competence and oocyte quality may be compromised by the toxicity of high cryoprotectant concentration in vitrification solution. Oocyte cryoprotectant toxicity can be interpreted as diminished survival and fertilization rates, ultra-structural alterations of intracellular organelles such as mitochondria and smooth endoplasmic reticulum, disruption of meiotic spindle apparatus, zona hardening due to the intracellular calcium rise, DNA fragmentation, in vitro aging and epigenetic disorders. Therefore, cryoprotectant toxicity is the main limiting factor for the success of cryopreservation. The potential toxicity of CPAs is directly related to the cryoprotectant type, concentration, temperature and time of exposure. However, the precise mechanism of their toxicity is poorly understood. Despite the fact that permeating CPAs often can be tolerated at exceptionally high concentrations and high temperatures, their toxic effects, particularly at higher temperatures, is well acknowledged and is generally accepted. Beside the specific toxicity (a particular cryoprotectant), CPAs has been proposed to have a non-specific toxicity caused by interfering with hydrogen bonding between water molecules. We follow with a description of specific cryoprotectant toxicity and how to prevent it. Some comparative cytotoxicity studies of the most commonly used permeating CPAs (glycerol/GLY, DMSO, PG, and EG) are also included. Glycerol (C3H5(OH)3), firstly identified by Polge, et al. in 1949 for cryopreservation of poultry spermatozoa, has the lowest oocyte membrane permeability and less toxicity compared to other CPAs. Exposure of oocytes to GLY could result in extremely high shrinkage which is partially associated with membrane damage due to the less permeability than other cryoprotectants. 1,2-Propanediol (PG), a commonly used CPAs, has the highest permeability and less osmotic membrane damage. Nonetheless, PG toxicity in excess of 2.5 M has been associated with a reduction of intracellular pH and subsequently impaired developmental competence of mouse zygotes. Beside the increased intracellular calcium and significant DNA damage of mouse oocytes, PG has higher toxic effects on immature porcine oocytes when compare with EG. However, the combination of PG with EG could significantly reduce its toxicity and improve blastocyst yield of vitrified oocytes. EG (CH2)2(OH)2, has been extensively studied for vitrification of mammalian oocytes. Higher blastocyst production rate for porcine oocytes vitrified with EG as compared to PG, implies lower possible toxicity of this cryoprotectant. However, the permeability of EG is lower than PG and DMSO. DMSO ((CH3)2SO) is the most frequently used permeating CPAs for vitrification of oocytes and embryos. Membrane permeability of DMSO is approximately between PG and EG for human oocyte. Intracellular calcium rise induced by DMSO, EG and PG could compromise the ability of oocyte to normal fertilization by initiate premature cortical reaction and hardening of zona pellucida. DMSO recruits calcium from intracellular store, whereas the sources of calcium rise for PG and EG is extracellular.
Reduction of cryoprotectant toxicity
Non-permeating CPAs play important role in decreasing the required concentration of permeating CPAs, which could in turn reduce potential toxicity of these agents. Osmotic swelling injury is also one of the major issues facing oocyte freezing. Addition and removal of CPAs during vitrification and thawing procedures may lead to severe volume excursion of the cell. Moreover, osmotic stress is mainly associated with type and concentration of CPAs, as cryoprotectants with high concentration and low permeability impose more osmotic damage. The lethal osmotic effects can be prevented by addition of impermeable compounds such as sugars or step-wise dilutions of cryoprotectants. Therefore, non-permeating CPAs provide an osmotic buffer that minimizes the oocyte damages that may otherwise occur in the wake of the osmotic stress caused by the dilution of CPAs during warming process. The extent of the shrink/swell response of the cell varies mainly depending on the permeability rate, size and type of CPA. Since nearly half of the cell is replaced by CPAs during vitrification, the success of cryopreservation can be largely attributed to the choice of the appropriate cryoprotectant. Addition of sucrose as a beneficial non-permeating extracellular cryoprotectant has become standard in oocyte cryopreservation. It can reduce oocyte damage by modulating the osmotic imbalance that occur during thawing, and provide required nutrition to preserved cells at low (-45?) temperatures. Trehalose is a well-known non-penetrating CPA, reported as less toxic and more efficient than sucrose in oocyte cryopreservation. This non-reducing disaccharide discovered by Wiggers in 1832, while studying solutions of the ergot in rye. Trehalose plays an important role in protection against different environmental stresses like drought, heat, osmotic shock and extremely low temperature. The cryoprotective properties of trehalose are mainly related to its stabilizing effects on both cellular proteins and membranes. This stabilization effects can be attributed to the specific interaction of trehalose with biological molecules in lipid bilayer. However, the exact mechanism is still unclear. Microinjection of trehalose into the cytoplasm of human and mouse oocytes has been considered as a novel technique to achieve high survival rate after vitrification. In this manner, trehalose appears to act as a penetrating CPA by preventing ice crystal formation during freezing procedure. Proline, as a natural nontoxic osmoprotectant has also been shown to preserve membrane structure and function by stabilization effects. Supplementation of vitrification solution with proline was found to be effective for improving survival and developmental rates of vitrified mouse oocytes. This antioxidant also provides normal spindle configuration and protects MII mouse oocyte from mitochondrial damage.
Reports on oocyte vitrification using different combination of CPAs
Successful oocyte vitrification depends on the appropriate combination of cryoprotectants. Many strategies have been attempted to minimize the CPA toxicity by optimizing the type and concentration of cryoprotectants. Additionally, several methods have been developed to increase cooling and warming rates, or reduce exposure time of oocytes to the vitrification solution. We focus here on the investigations that examine mammalian oocyte competence after vitrification with different types and concentrations of cryoprotectants.
Ethylene Glycol (EG)+Dimethyl Sulfoxide (DMSO)
EG and DMSO is the most commonly used combination of permeating cryoprotectants which has been successfully applied for vitrification of mouse, human, ovine and bovine oocytes. Most of the above-mentioned studies have reported more than 80% survival and cleavage rates for post-thaw oocytes following vitrification with 15% DMSO, 15% EG and 0.5 M sucrose. Furthermore, analysis of blastocysts derived from vitrified-warmed human oocytes revealed no increase in chromosome abnormalities as an indicator of the safety and efficiency of a vitrification procedure. This finding is consistent with other studies indicating a similar risk of aneuploidy and embryo quality between vitrified and control groups. According to a study conducted by Coticchio, et al. bipolar spindle configuration and chromosome alignment of MII human oocytes may be compromised by vitrification. In addition, mitochondrial dysfunction and a reduction in relative inner membrane potential of in vitro matured human oocytes have been reported by Lei et al. after vitrification. However, Lei, et al.’s study has shown no remarkable differences between fresh and vitrified oocytes with respect to spindle and chromosome abnormalities. Sucrose with the combination of DMSO and EG maintains good cytoprotective properties, even at very low concentration (i.e., 0.5 mM), as shown by Garcia, et al. In this study, cleavage, blastocyst formation rates and quality of embryos obtained from vitrified oocytes were similar to the control group. Meanwhile, functional and ultrastructural analysis of porcine MII oocyte following vitrification with 17% DMSO, 17% EG and 0.4 M sucrose, revealed major alterations in distribution and membrane potential of mitochondria, occurrence of apoptosis, and therefore embryo development. These differences could be partially explained by extremely high cryo-sensitivity of porcine oocyte which can related to higher lipid content of porcine oocyte than other mammalian species. The toxicity-minimized procedure has been also examined by Habibi, et al. for vitrification of mouse oocytes. They found that 15% cryoprotectant (7.5% DMSO, 7.5% EG, 0.5 M sucrose) provide similar survival, fertilization, cleavage and blastocyst rates when compared to commonly used 30% (15% DMSO, 15% EG, 0.5 M sucrose). Although, these values were significantly lower in vitrified oocytes than those of fresh ones. Toxicity of CPAs can also be decreased or prevented by addition of some antioxidant; consistent with Zhang et al. study who found that supplementation of vitrification solution with L-proline was effective in protection against mitochondrial injury and ROS production in vitrified mouse oocytes. This natural osmoprotectant in a vitrification solution containing a mixture of 2 M proline, 7.5% DMSO, 10% EG and 0.5 M sucrose had no adverse effects on spindle configuration and embryo development, while minimizing the concentration and subsequent toxicity of cryoprotectants.
Ethylene Glycol (EG)+1,2-Propanediol (PROH)
EG is often used in conjunction with DMSO or PROH for vitrification of mammalian oocyte. PROH at the same concentration as EG and DMSO (i.e., 1.5 M) could have deleterious effects on fertilization, embryonic development, and chromosomal normality of mouse oocytes. Similarly, the toxic effects of PROH demonstrated by Huang, et al., in which vitrification of in vitro and in vivo matured mouse oocytes using a solution consisting of 2.6 M EG, 2 M PROH, and 0.5 M sucrose, lead to reduced embryonic developmental ability, decreased normal spindle morphology and chromosome configuration. However, viability and incidence of aneuploidy did not significantly differ from that of the non-vitrified control group in Huang et al studies. The toxicity effects of PROH could be avoided by combining its lower concentration (i.e., 0.75 M) with other cryoprotectants, while keeping the total CPA concentration at a cryoprotective level. Substitution of DMSO with PROH in vitrification media of bovine oocytes resulted in a significantly higher blastocyst formation rate, as found by Chian, et al. However, it has been demonstrated that human and bovine oocytes had an equivalent survival and cleavage rates after vitrification in a solution with a mixture of 15% PROH, 15% EG and 0.5 M sucrose or 15% DMSO, 15% EG and 0.5 M sucrose. Therefore, despite the high permeability and less induced osmotic damage, PROH may compromise the success of a vitrification procedure due to toxic effects of high concentration. This issue needs to be considered in preparation of vitrification solution.
Discussion
Ethylene glycol or Dimethyl sulfoxide
While many studies investigated the combination of several cryoprotectants, there have been few direct comparisons of the effectiveness of EG or DMSO alone for vitrification of mammalian oocytes. El-Shahat, et al. compared three vitrification solutions for immature buffalo oocytes which were composed of either 4 M GLY, 7 M EG or 7 M DMSO in combination with 0.5 M sucrose. Oocytes vitrified in DMSO or EG groups resulted in a significantly higher cleavage and blastocyst formation rates than oocytes in the GLY group. EG and DMSO groups also showed an increase in maturation rate, with a significant difference in EG only. This finding can be explained by the lower toxicity of EG than DMSO Both EG and DMSO have higher membrane permeability than GLY. Despite the low toxicity in high concentration, GLY was usually excluded in most of investigations due to inadequate membrane permeability and consequent osmotic damage. Osmotic shock as a mechanism of freezing injury, affects the integrity of plasma membrane and cytoskeletal organization and therefore lowers the proportion of oocytes with normal morphology. Concern about osmotic stress is also important when using EG, as mammalian oocytes generally have a lower permeability to EG relative to DMSO and PROH. Nevertheless, it seems that EG could minimize the damages to oocyte as shown by Kamoshita, et al. [98], who established an efficient method for vitrification of immature mouse oocytes using a calcium-free vitrification solution consisting of 30% EG and 0.5 M sucrose. These findings are further supported by Somfai et al. who found a higher percentage of blastocyst formation for porcine oocytes vitrified in 35% EG compared to 35% PROH. However, these findings were partly contradicted by Cha et al. study who reported higher maturation and blastocyst formation rates for GV and MII mouse oocytes vitrified in a combination of 2.7 M EG and 2.1 M DMSO compared to EG only (5.5 M EG, equivalent to ~30% EG and 1.0 M sucrose). Differences in these observations could be attributed to differences in base medium, as Kamoshita et al. used a calcium-free vitrification solution, which may lead to reduced zona hardening and improved developmental ability of post-thaw oocytes. In a more extensive study the effectiveness of EG, DMSO and PROH was investigated for vitrification of mature human oocytes, either individually or in combination with each other. Evaluation of oocyte quality revealed that EG+DMSO and EG+PROH provide best results in terms of morphological and functional parameters, with the highest survival rate of EG+PROH group. In contrast, the most deleterious effects were obtained by using EG only or PROH+DMSO. The higher survival rate in EG+PROH group may be due to the higher permeability of PROH than DSMO. Moreover, the toxicity imposed by DMSO+PROH appear to be more than EG + DSMO.
Non-permeating CPAs
A combination of non-penetrating and penetrating CPAs was found to further improve viability and clinical outcomes of oocytes vitrification by diminish cytotoxicity of permeating CPAs. Non-penetrating CPAs such as sucrose and trehalose are known to prevent osmotic shock and cell swelling during vitrification and warming procedure. Some studies have suggested that trehalose supplemented mediums are more likely to exert protective effects against cryoinjury than sucrose one. For example, in an experiment conducted by Lestari et al. in order to investigate embryo development of vitrified-warmed mouse oocyte, 0.5 M trehalose in combination with 16.5% EG and 16.5% DMSO was shown to have significantly higher efficacy compared with the same concentration of sucrose. However, in this study, there was a good morphological grading and embryo development in both vitrification solutions. Membrane stabilizing properties of trehalose may explain the increased developmental ability of oocytes after vitrification.
Conclusion
Taken to gather, this review demonstrated that a vitrification solution composed of EG+PROH or EG+DMSO either in combination with sucrose or trehalose are safer to use for oocyte vitrification than DMSO+PROH. It seems that EG could play an important role at improving the outcomes of oocyte freezing, either alone or in conjunction with DMSO or PROH. Regarding the CPAs toxicity, we also suggest that PROH at its lower concentration can be combined with other permeating CPAs such as EG and DMSO. However, the cytotoxicity of PROH can also be further diminished if combined with EG rather than DMSO, due to the lower toxicity of EG than DMSO. Optimization of vitrification media may further improve the post-thaw embryo development and clinical outcomes of oocyte.
Conflict of interest
The authors declare no conflict of interest.
References
- Hickman LC, Llarena NC, Valentine LN, Liu X, Falcone T (2018) Preservation of gonadal function in women undergoing chemotherapy: a systematic review and meta-analysis of the potential role for gonadotropin-releasing hormone agonists. J Assist Reprod Genet 35:571–581.
- Specchia C, Baggiani A, Immediata V, Ronchetti C, Cesana A, et al. (2019) Oocyte Cryopreservation in Oncological Patients: Eighteen Years’ Experience of a Tertiary Care Referral Center. Front Endocrinol (Lausanne) 10:600.
- Khiat S, Provansal M, Bottin P, Saias-Magnan J, Metzler-Guillemain C, et al. (2020) Fertility preservation after fertility-sparing surgery in women with borderline ovarian tumours. Eur J Obstet Gynecol Reprod Biol 253:65–70.
- Rodriguez-Wallberg KA, Hao X, Marklund A, Johansen G, Borgström B, et al. (2021). Hot Topics on Fertility Preservation for Women and Girls-Current Research, Knowledge Gaps, and Future Possibilities. J Clin Med 10:1650.
- Devine K, Mumford SL, Goldman KN, Hodes-Wertz B, Druckenmiller S, et al. (2015) Baby budgeting: oocyte cryopreservation in women delaying reproduction can reduce cost per live birth. Fertil Steril 103:1446–1453.e532.
- Allahbadia GN (2016) Social Egg Freezing: Developing Countries Are Not Exempt. J Obstet Gynaecol India 66:213–217.
- Kim SJ, Kim SK, Lee JR, Suh CS, Kim SH (2020). Oocyte cryopreservation for fertility preservation in women with ovarian endometriosis. Reprod Biomed Online 40:827–834.
- Condorelli M, Demeestere I (2019) Challenges of fertility preservation in non-oncological diseases. Acta Obstet Gynecol Scand 98:638–646.
- Deepinder F, Agarwal A (2008) Technical and ethical challenges of fertility preservation in young cancer patients. Reprod Biomed Online 16:784–791.
- Rajabi Z, Aliakbari F, Yazdekhasti H (2018) Female Fertility Preservation, Clinical and Experimental Options. J Reprod Infertil 19:125–132.
- Cobo A, Remohí J, Chang CC, Nagy ZP (2011) Oocyte cryopreservation for donor egg banking. Reproductive biomedicine online, 23:341–346.
- Iussig B, Maggiulli R, Fabozzi G, Bertelle S, Vaiarelli A, et al. (2019) A brief history of oocyte cryopreservation: Arguments and facts. Acta Obstet Gynecol Scand 98:550–558.
- Aman RR, Parks JE (1994) Effects of cooling and rewarming on the meiotic spindle and chromosomes of in vitro-matured bovine oocytes. Biol Reprod 50:103–110.
- Zenzes MT, Bielecki R, Casper RF, Leibo SP (2001) Effects of chilling to 0 degrees C on the morphology of meiotic spindles in human metaphase II oocytes. Fertil Steril 75:769–777.
- Chen SU, Lien YR, Chao KH, Ho HN, Yang YS, et al. (2003) Effects of cryopreservation on meiotic spindles of oocytes and its dynamics after thawing: clinical implications in oocyte freezing--a review article. Mol Cell Endocrinol 202:101–107.
- Eroglu A, Toth TL, Toner M (1998). Alterations of the cytoskeleton and polyploidy induced by cryopreservation of metaphase II mouse oocytes. Fertil Steril 69:944–957.
- Martínez-Burgos M, Herrero L, Megías D, Salvanes R, Montoya MC, et al. (2011) Vitrification versus slow freezing of oocytes: effects on morphologic appearance, meiotic spindle configuration, and DNA damage. Fertil Steril 95:374–377.
- Jones A, Van Blerkom J, Davis P, Toledo AA (2004) Cryopreservation of metaphase II human oocytes effects mitochondrial membrane potential: implications for developmental competence. Hum Reprod 19:1861–1866.
- Lei T, Guo N, Tan MH, Li YF (2014) Effect of mouse oocyte vitrification on mitochondrial membrane potential and distribution. J Huazhong Univ Sci Technolog Med Sci 34:99–102.
- Gualtieri R, Kalthur G, Barbato V, Di Nardo M, Adiga SK, et al. (2021) Mitochondrial Dysfunction and Oxidative Stress Caused by Cryopreservation in Reproductive Cells. Antioxidants (Basel) 10:337.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi