Review Article, J Spine Neurosurg Vol: 8 Issue: 3
A Single Sagittal Parameter for Decision Making in Adult Spinal Deformity
David Christopher Kieser1*, Louis Boissiere2, Caglar Yilgor C3, Daniel Larrieu4, Takashi Fujishiro2, Ahmet Alanay3, Emre Acaroglu5, Frank Kleinstueck6, Ferran Pellise´7, Francisco Javier Sanchez Perez-Grueso8, Anouar Bourghli9, Derek Cawley2, Jean-Marc Vital2, Olivier Gille2 and Ibrahim Obeid2
1Department of Orthopaedic Surgery and Musculoskeletal Medicine, University of Otago, Christchurch School of Medicine, Christchurch, New Zealand
2L’Institut de la Colonne Vertébrale, CHU Pellegrin, 33076 Bordeaux, France
3Acibadem University School of Medicine, Istanbul, Turkey
4L’Institut de la Colonne Vertébrale, Bordeaux University Hospital, Place Amélie Raba-Léon, 33076, Bordeaux, France
5Spine Surgery Unit, Ankara Acibadem ARTES Spine Center, Ankara, Turkey
6Spine Center, Schulthess Klinik, Zurich, Switzerland
7Spine Surgery Unit, Hospital Universitario Val Hebron, Barcelona, Spain
8Spine Surgery Unit, Hospital Universitario La Paz, Madrid, Spain
9Orthopedic and Spinal Surgery Department, Kingdom Hospital, Riyadh, Saudi Arabia
*Corresponding Author : David Kieser Department of Orthopaedic Surgery and Musculoskeletal Medicine, Canterbury District Health Board, 2 Riccarton Avenue, Christchurch, New Zealand Fax: 0064 3 467 9709 Tel: 0064 21 149 9829 E-mail:kieserdavid@gmail.com
Received: March 21, 2019 Accepted: May 14, 2019 Published: May 20, 2019
Citation: Kieser DC, Boissiere L, Yilgor CC, Larrieu D, Fujishiro T, et al. (2019) A Single Sagittal Parameter for Decision Making in Adult Spinal Deformity. J Spine Neurosurg 8:3.
Abstract
Objective: Decision-making in adult spinal deformity (ASD) remains challenging with complex algorithms and scores inhibiting every day use. Thus, there is an appetite for a simplified parameter to be identified that can guide surgical decision-making. This study therefore questions whether a simplified sagittal modifier (SSM) or relative spinopelvic alignment (RSA) could offer a reliable tool to determine operative intervention in patients with ASD. Methods: Multicenter, prospective study of consecutive ASD patients. Inclusion criteria were ASD patients presenting with at least one criteria: Cobb ≥ 20°; SVA ≥ 5 cm; TK ≥ 60° or PT ≥ 25°. A total of 1238 patients (431 non-operative and 807 operative) were classified according to their SSM and RSA. A Chi2 test was performed for surgical indication (operated or not). p<0.05 value was considered significant. Results: For non-operative patients: 235 (55%) were classified as aligned with SSM and 323 (75%) with the RSA; 157 (36%) vs. 39 (9%) respectively as moderate and 39 (9%) vs. 69 (16%) respectively as severe malalignment. For operative patients: 252 (31%) vs. 388 (48%) respectively were classified as aligned, 289 (36%) vs. 96 (12%) respectively as moderate and 266 (33%) vs. 323 (40%) respectively as severe malalignment with each respective modifier. Both modifiers were significant (p<0.01) for decision-making. Conclusions: Both the SSM and RSA are significantly correlated to the intention to surgically treat patients with ASD. RSA is a simple and powerful parameter that is more discriminant than SSM in decision-making. RSA should be considered as a parameter that can guide the decision for surgical intervention in patients with ASD.
Keywords: Scoliosis; Spinal fusion; Spine
Introduction
Adult spinal deformity (ASD) combines a broad group of spinal pathologies causing malalignment in the frontal and/or sagittal plane. ASD can, in some cases, lead to severe disability requiring surgery. The degree of such disability is measured through health related quality of life (HRQL) scores and the more disabled patients are the more likely they are to receive surgical treatment [1]. ASD can objectively be evaluated by performing full-spine x-rays, in the standing position, to measure specific radiographic parameters [2]. Over recent years, the univariate correlation between radiographic parameters and HRQL scores has been prevalent in the literature. Glassman was the first to highlight the linear relationship between the sagittal vertical axis (SVA) and the Oswestry disability index (ODI) [3]. The studies that followed reinforced the necessity to take account of sagittal malalignment, as this has repetitively been shown to correlate with HRQL scores [4].
Despite the multitude of ASD classification systems proposed, the SRS-Schwab is the only radiographic classification system that is accurately correlated with HRQL scores [5]. It is for this reason, that this system is currently the most commonly employed classification for ASD. When the classification was first described, the three sagittal modifiers (pelvic tilt (PT), SVA and pelvic incidence minus lumbar lordosis (PI-LL)) were the parameters correlating the most with HRQL scores. In summary, lack of lumbar lordosis, with spinal and pelvic malalignment appeared at this time to be the best way to describe malalignment severity. However, a drawback for this classification was its complexity, because of the number of classification possibilities it offers. Indeed with 27 classification possibilities just for sagittal alignment, too many subgroups ensued making it difficult to use on a day-to-day basis. Thus, although overall the classification was significant for decision making, inside each subgroup it is impossible to know if a patient should receive surgery or not [6].
Recently a simplification of the SRS-Schwab classification was proposed by summing up the number of “+” resulting from SVA, PT and PI-LL modifiers. This simplified sagittal modifier (SSM), divided in three categories (aligned 0+, moderate deformity 1 to 3+ and severe deformity 4+ or more), offered to reduce the number of sagittal classification possibilities from 27 to 3. This modifier was compared to the SRS-Schwab classification and no loss of information was found from this simplification [7]. Thus, the SSM appeared as a potential parameter to guide decisionmaking on a day-to-day basis.
Since the SRS-Schwab classification, many other radiographic parameters have been described [8]. The development of a multicenter database offered the possibility to enhance the number of included patients allowing multivariate analyses. These studies have revealed that the impact of sagittal malalignment on HRQL scores is important, but that simply adding up different sagittal parameters fails to adequately evaluate deformities [9,10].
The relative sagittal alignment (RSA) parameter described by Yilgor and colleagues [11] is a PI based global parameter that evaluates the amount of malalignment based on a patient’s ideal global tilt (GT) (RSA=GT-ideal GT with ideal GT=0.48 × PI-15). Four subgroups are described: negative <-7°, aligned -7-10°, moderate deformity 10.1-18°, severe deformity>18°. The RSA therefore has the potential to be a single parameter that represents the disability due to sagittal malalignment.
We therefore questioned the validity of the SSM and RSA at predicting surgical decision making. Thus, the purpose of this study was to compare the accuracy of the SSM and RSA to identify patients for whom a surgical intervention has been advocated in the European Spine Study Group (ESSG).
Materials and Methods
Study design
A multicenter study of prospectively collected ASD patients from six spine centers. Institutional review board approval was obtained at each site for patient enrolment and data collection. Inclusion criteria were patients, presenting with at least one criteria: Coronal cobb ≥ 20°; SVA ≥ 5 cm; Thoracic kyphosis (TK) ≥ 60° or PT ≥ 25°. Exclusion criteria were patients for whom no surgical decision had been made at the time of enrolment.
Analysed variables
Baseline data from all patients were analyzed including SSM, RSA, ODI and surgical indication (operative versus non-operative patients). The definitive outcome variable was the intention to treat with surgical intervention.
Patient classification
All patients were categorized following SSM and RSA surgical indication (operative or not). Considering each parameter specificities, the patients were divided into aligned (0+for SSM and negative (<-7°) or aligned -(7-10°) for RSA), moderate deformity (1- 3+for SSM and moderate deformity (10.1-18°) for RSA) and severe deformity (4-6+for SSM and severe (>18°) for RSA). All patients for whom an operative decision was made were included in the operative patient group.
Statistical analysis
A Chi-squared test was performed to evaluate the relationship between SSM, RSA modifiers and surgical indication. An ANOVA was performed to analyze the relationship between ODI and categories for operative and non-operative patients. P<0.05 value was considered significant.
Results
A total of 1238 patients were included in this study (431 nonoperative and 807 operative). The average age was 50 years (range 18-87 years).
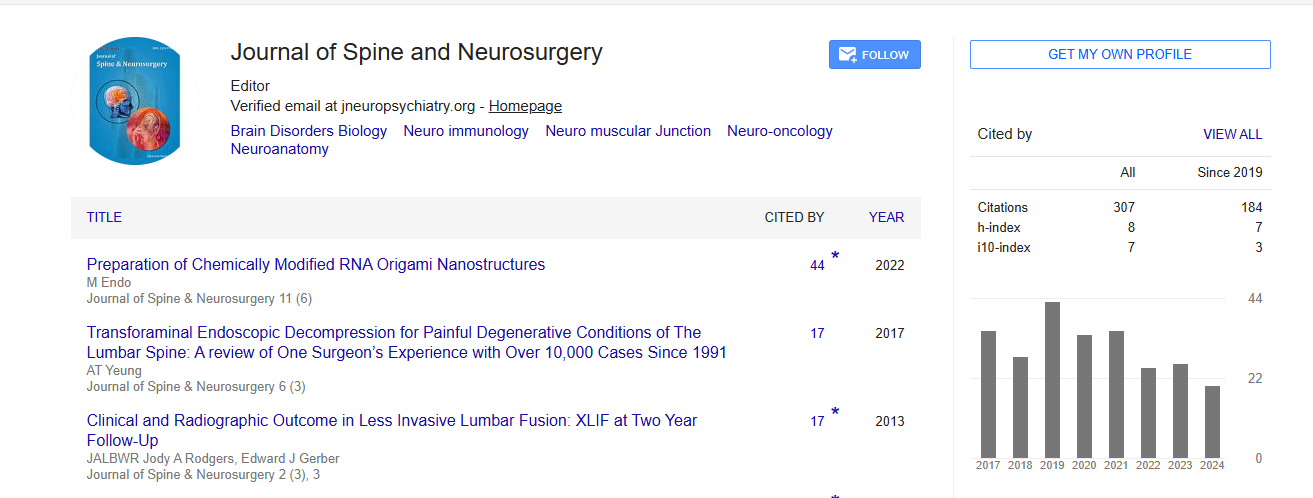
For non-operative patients: 235 patients (55%) were classified as aligned with SSM and 323 patients (75%) with RSA respectively; 157 patients (36%) compared to 39 patients (9%) as moderate malalignment and 39 patients (9%) compared to 69 patients (16%) as severe malalignment respectively (Table 1). For operative patients: 252 patients (31%) were classified as aligned with SSM and 388 patients (48%) were classified as aligned with RSA respectively, 289 patients (36%) compared to 96 patients (12%) as moderate malalignment and 266 patients (33%) compared to 323 (40%) as severe malalignment respectively. Both modifiers were significant (p<0.01) for decision making in each category.
Non-operative patients |
|||
|---|---|---|---|
| SSM | 235 (55%) | 157 (36%) | 39 (9%) |
| RSA | 323 (75%) | 39 (9%) | 69 (16%) |
| Operative patients | |||
| SSM | 252 (31%) | 289 (36%) | 266 (33%) |
| RSA | 388 (48%) | 96 (12%) | 323 (40%) |
Table 1: Patient distribution regarding SSM, RSA and surgical indication.
For both SSM and RSA, the ratio between operative patients and non-operative patients gradually increases with worsened sagittal balance (Figure 1). The percentage of aligned patients undergoing operative intervention highlights the presence of two groups of operated patients: 1 group for sagittal malalignment issues and another group without sagittal malalignment concerns. Thus, neither the SSM nor the RSA can completely explain the intention to treat.
Discussion
Our results show that both the SSM and RSA are significantly related to the decision to offer operative intervention in patients with ASD, testifying the necessity to take account of sagittal balance when treating these patients. Over recent years, the relationship between sagittal malalignment and ASD has been extensively described. The univariate correlation between radiographic parameters and HRQL scores has driven the concept that, the sagittal balance is the most important factor to take into consideration when deciding on operative intervention. Many radiographic parameters have thus subsequently been described, in order to obtain the highest possible correlation with HRQL. However, the search for a single parameter to aid operative decision-making remains elusive.
More recently, the advent of large multi-center cohorts has allowed multivariate analysis and has highlighted the variable impact of radiographic parameters on HRQL scores. These studies have emphasized that the decision to treat is not solely based on sagittal malalignment, but rather a combination of factors including patient age, symptoms, coronal cobb angle, comorbidities and previous surgeries. This explains why patients in our study who are sagittally aligned do not necessarily undergo operative intervention. However, although not the sole determinant of operative intervention, all radiographic sagittal parameters correlate with HRQL scores in multivariate analysis [10]. Thus, sagittal balance needs to be considered as one of the factors in decision-making. But, simply adding the value of sagittal parameters, like it is proposed in SRSSchwab classification, does not provide more information on patients’ disability due to malalignment. Furthermore, the relationship between these parameters and the recommendation to perform surgery is not the same as equating these parameters with improved HRQL scores.
If a single parameter could by itself represent the disability inflicted by sagittal malalignment, this parameter would need to be adapted to evaluate a broad range of pathologies. Indeed, the analysis of a lumbar arthrogenic kyphosis is different from the analysis of a higher thoracic post-traumatic kyphosis. For this reason, we decided to use the SSM, which refers to the gold standard classification actually employed for ASD evaluation. The SSM has been validated and gives as much information for decision making as the original SRS-Schwab classification. It simultaneously evaluates spinal malalignment (SVA, PI-LL) and pelvic compensation (PT). A drawback for this parameter is that it includes three measurements and not a single, which has been recently advocated by multivariate analysis. So, the RSA appeared to be a potential single sagittal parameter that takes into account spinal malalignment and pelvic compensation.
We found that both the SSM and RSA were significant in deciding whether operative intervention is required. But, the RSA seems to be more discriminant, with less aligned patients being offered operative intervention than those classified according to the SSM. However, this must be interpreted with caution because an important limitation of this study is that malalignment categories include different patients, which makes comparisons between the two classifications difficult. The values used in this manuscript are those proposed for SSM and RSA in the literature. These values have been validated and were therefore, difficult not to consider. For the RSA, we proposed three categories in contrast to the four categories described by the original authors. We decided to classify the patients considered as negatively aligned (RSA <-7°), as aligned. The concept of preoperative negative malalignment that was introduced in the description of the GAP score appeared as a rather new concept that would be difficult to compare to the SSM score. Typically, life is considered a kyphosing event, but special attention should be made in the future to characterize this specific point.
Conclusions
Both the SSM and RSA are significantly correlated to the intention to surgically treat patients with ASD. RSA is a simple and powerful parameter that is more discriminant than SSM in decision-making. RSA should be considered as a parameter that can guide the decision for surgical intervention in patients with ASD.
Acknowledgments
Glynny Kieser for her editorial input.
References
- Acaroglu E, Yavuz AC, Guler UO (2016) A decision analysis to identify the ideal treatment for adult spinal deformity: is surgery better than non-surgical treatment in improving health-related quality of life and decreasing the disease burden? Eur Spine J 25: 2390-2400.
- Mac-Thiong JM, Roussouly P, Berthonnaud E (1976) Sagittal parameters of global spinal balance: normative values from a prospective cohort of seven hundred nine Caucasian asymptomatic adults. Spine (Phila Pa 1976) 35: E1193-1198.
- Glassman SD, Bridwell K, Dimar JR (2005) The impact of positive sagittal balance in adult spinal deformity. Spine (Phila Pa 1976) 30: 2024-2029.
- Schwab FJ, Blondel B, Bess S (1976) Radiographical spinopelvic parameters and disability in the setting of adult spinal deformity: a prospective multicenter analysis. Spine (Phila Pa 1976) 38: E803-812.
- Schwab F, Ungar B, Blondel B (2012) Scoliosis Research Society-Schwab adult spinal deformity classification: a validation study. Spine (Phila Pa 1976) 37: 1077-1082.
- Terran J, Schwab F, Shaffrey CI (2013) The SRS-Schwab adult spinal deformity classification: assessment and clinical correlations based on a prospective operative and nonoperative cohort. Neurosurgery 73: 559-568.
- Boissiere L, Obeid I, Acaroglu E (2016) Validation and Simplification of SRS-Schwab Classification. SRS 51st Annual Meeting & Course. Prague, Czech Republic. 2016.
- Obeid I, Boissiere L, Yilgor C (2016) Global tilt: A single parameter incorporating spinal and pelvic sagittal parameters and least affected by patient positioning. Eur Spine J 25: 3644-3649.
- Takemoto M, Boissiere L, Vital JM (2017) Are sagittal spinopelvic radiographic parameters significantly associated with quality of life of adult spinal deformity patients? Multivariate linear regression analyses for pre-operative and short-term post-operative health-related quality of life. Eur Spine J 26: 2176-2186.
- Boissiere L, Takemoto M, Bourghli A (2017) Global tilt and lumbar lordosis index: two parameters correlating with health-related quality of life scores-but how do they truly impact disability? Spine J 17: 480-488.
- Yilgor C, Sogunmez N, Boissiere L (2017) Global alignment and proportion (GAP) score: Development and validation of a new method of analyzing spinopelvic alignment to predict mechanical complications after adult spinal deformity surgery. J Bone Joint Surg Am 99: 1661-1672.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi