Research Article, Jtsdt Vol: 13 Issue: 1
A Study of Post-concussion Symptoms in Mild Traumatic Brain Injury Patients
Chatkhane Pearkao1*, Tassanee Nusitpap1, Surakrant Yutthakasemsunt2, Wiphawadee Potisopha1
1Faculty of Nursing, Khon Kaen University, Khon Kaen, Thailand
2Surgical Unit, Khon Kaen Regional Hospital, Thailand
*Corresponding Author: Chatkhane Pearkao
Faculty of Nursing, Khon Kaen University, Khon Kaen, Thailand
E-mail: porpea@kku. ac.th
Received: 15-Mar-2024, Manuscript No. JTSDT-23-122872;
Editor assigned: 16-Mar-2024, PreQC No. JTSDT-23-122872 (PQ);
Reviewed: 01-Apr-2024, QC No. JTSDT-23-122872;
Revised: 05- Apr-2024, Manuscript No. JTSDT-23-122872 (R);
Published: 12-Apr- 2024, DOI:10.4172/2324-8947.1000386
Citation: Pearkao C, Nusitpap T, Yutthakasemsunt S, Potisopha W, et al. (2024) A Study of Post-concussion Symptoms in Mild Traumatic Brain Injury Patients. J Trauma Stress Disor Treat 13:2.
Copyright: © 2024 Pearkao C. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Objective: Patients with mild traumatic brain injury account for 80% of all traumatic brain injury cases. Patients with symptoms were found to occur following traumatic brain injury. The purpose of this study was to post-concussion symptoms and post-traumatic amnesia.
Method: This prospective observational study was conducted in the Emergency Department (ED) of two tertiary care hospitals in Thailand’s Khon Kaen Province. Patients with mild traumatic brain injuries had phone interviews for the first 24 hours, first week, second week, and fourth week after the injury to assess postconcussion symptoms and post-traumatic amnesia.
Results: 166 patients completed the follow-up assessment four times. The mean severity of RPQ-3 symptoms was significantly reduced (p <.01). RPQ-13. The mean severity score of symptoms increased statistically significantly (p< .01). Amnesia, on the other hand, was discovered in 11.40 percent of patients within the first 24 hours.
Conclusion: Post-concussion symptoms, there was the occurrence of symptoms and their severity for each group, the time difference. Amnesia appears within 24 hours of trauma. These results could be used in discharge planning and referral care for continuing cares.
Keywords: Mild traumatic brain injury; Post-concussion symptoms; Posttraumatic amnesia
Introduction
Traumatic Brain Injury (TBI) is a major public health concern around the world, including in Thailand. Brain injuries affect an estimated 69 million people worldwide each year. It is found primarily in Southeast Asia and the Western Pacific [1]. Traffic is the leading cause of brain injury, particularly in developing countries. However, 2.8 million people with traumatic brain injury have been reported in emergency departments in the United States [2]. The Glasgow Coma Score (GCS) is a tool used to categorize brain injury severity into three levels: 1) mild traumatic brain injury (GCS 13-15), 2) moderate traumatic brain injury (GCS 9-12), and 3) severe traumatic brain injury (GCS 3-8), [3] with mild traumatic brain injury being the most common, accounting for approximately 80% of traumatic brain injury[1,4]. Mild TBI is classified into three levels based on risk factors: low risk, moderate risk, and high risk. Low-risk groups do not to be admitted to the hospital to observe symptoms [5].
Moderate-risk groups may need hospitalization or brain computed tomography. When the patient's symptoms have stabilized, they will be discharged. Patients with mild TBI, according to guidelines developed by the Royal College of Surgeons of Thailand and the College of Neurological Surgeons of Thailand. However, even if the injury is not severe, there is a risk of brain haemorrhage in patients with mild traumatic brain injury. There is also a risk of post-concussion symptoms, [6] which are caused by brain injury and result in abnormalities in brain function, as well as patients with neurological impairments such as unconsciousness and amnesia [7]. Post-traumatic amnesia can be caused by both retrograde and anterograde amnesia [8]. It may occur over a period of hours, days, months, or even years and is a predictor of function following a brain injury, [9] which may affect perception and lower the patient's quality of life. Moreover, it was discovered that there were signs of traumatic brain injury, such as headache, insomnia, irritability, forgetfulness, hyperactivity, and double vision. The symptoms can be divided into 1) physical symptoms, 2) behavioral and emotional symptoms, and) cognitive symptoms [10,11]. According to research, 85% of symptoms following traumatic brain injury appeared within the first week. The most frequent symptoms were headaches, forgetfulness, drowsiness, fatigue, and dizziness [7]. Typically, the symptoms appeared and disappeared within 7 to 14 days [12]. 10-25% of people [13] had symptoms that lasted between three months and a year. It is a problem with lifestyle. Work and obligations prevent patients from participating in activities with others, which typically lowers their quality of life [14].
Caring for patients with mild traumatic brain injuries (moderate and high-risk groups) who were admitted from the emergency room to the trauma ward for observation and close monitoring until discharge, as well as follow-up treatment for two weeks to one month after the patient is discharged and returned to school or work, some people still experience varying degrees of symptoms after a traumatic brain injury, which has an impact on the patient's way of life. Therefore, the researcher is interested in research to understand the symptoms. In patients with mild traumatic brain injury, the severity of post-injury symptoms and post-traumatic amnesia were assessed during the first 24 hours, first week, second weeks, and fourth weeks after the injury. The study's findings will help healthcare providers understand the symptoms and progression of the disease. To prepare, discharge plan, and refer patients in the context of continuity of care.
Methods
Participants
Patients with mild traumatic brain injury were conducted in the emergency department and transferred to the trauma ward. The inclusion criteria were patients with mTBI, moderate risk, and high-risk GCS score of 13 – 15, aged 18-60 years old, having a phone for telephone interviews, having no psychiatric diagnosis before the injury, and having no alcohol withdrawal syndrome. The researcher has calculated the sample size was determined according to the program G* Power version 3.1.9.7 [15], using an effect size of .25, a power of the test of 0.80, and a level of significance (alpha level) of 0.05, the sample size was 158, adjusting the dropout rate of 10% [16], the total sample size was 174.
Procedures
After the human ethics committee's approval, the data collection, the ward nurses initially screened the data from the qualifying sample. The researcher welcomes the sample population. Clarify the study's goals and specifics when the sampling agrees to participate by informed consent obtained in written form before data collection begins. The tools used to collect sample data consisted of three parts as follows:
1. General information and clinical information forms
2. The River mead Post-Concussion Symptom Questionnaire
3. The Galveston Orientation and Amnesia Test (GOAT)
Participants were interviewed by phone to follow up after a traumatic brain injury.
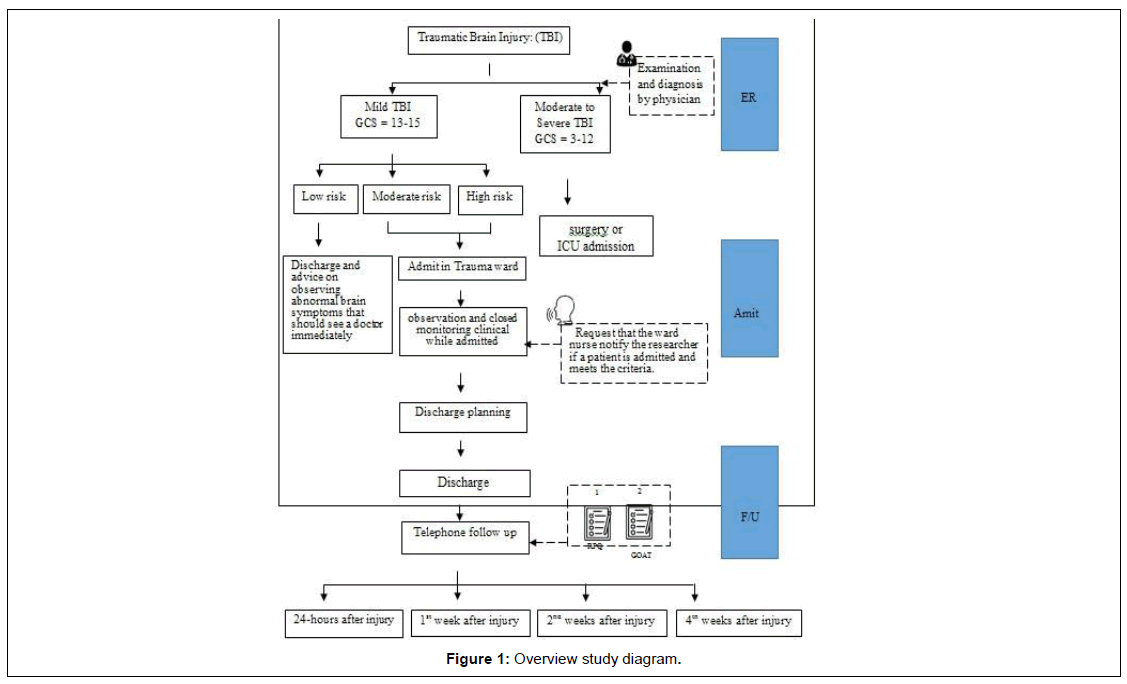
The Rivermead Post-Concussion Symptom Questionnaire (RPQ) and the Galveston Orientation and Amnesia Test (GOAT) are the interviewing tools used in the first 24 hours, first week, second weeks, and fourth weeks after injury. (Figure 1) The researcher explains to the sample how to understand the questions in the assessment form to clarify any misunderstandings. The interview lasts 15 to 20 minutes, and scheduling a time and date that work for the patient must be done before calling the patient for an interview. The information was gathered between June and August 2022.
Measures
The tool used to collect sample data and for analyzed of this study as follows:
1) The River mead Post-Concussion Symptom Questionnaire (RPQ) is an instrument developed by King et al. (1995) [17] and modified scoring version by Eyres et al. (2005) [18], The assessment consisted of 16 symptom questions and two open-ended questions, divided into two groups: RPQ-3 and RPQ-13. There are Likert scale five levels of 0-4 of the score. (0 = not experienced at all, 1 = no more of a problem, 2 = a mild problem, 3 = a moderate problem, and 4 = a severe problem). The RPQ-3 consists of the first three items; the score is potentially 0–12. The RPQ-13 comprises the next 13 items, the score is potentially 0–52, and the total score in RPQ is 0 – 64.
2) The Galveston Orientation and Amnesia Test (GOAT) is an instrument developed by Levin, O'Donnell & Grossman (1979) [19]. There are a total of 10 questions, and a score of less than 75 points is a patient with memory loss after traumatic brain injury, and a score greater than 75 points means the patient has no memory loss after traumatic brain injury.
Data analysis
Analysis was performed using IBM SPSS for Windows computer programs. The general and clinical information of The Galveston Orientation and Amnesia Test (GOAT) was analyzed by frequency, percentage, mean, and standard deviation. The River mead Post-Concussion Symptom Questionnaire (RPQ) was analyzed using repeated measures ANOVA to compare symptoms, onset, and severity after traumatic brain injury during the first 24 hours, first week, second weeks, and fourth weeks. Before the analysis, statistical assumptions were tested. The results of Mauchly's Test of Sphericity were found to be significant. This is not in accordance with the preliminary agreement that the analytical results can be read by the Sphericity calculation method. Therefore, the analytical results are reported using Greenhouse-Geisser.
Results
A post-traumatic brain injury and post-traumatic amnesia study were conducted on patients with mTBI, moderate-risk, and high-risk, and patients were followed up for the first 24 hours, first week, second weeks, and fourth weeks after injury. Because eight samples were not collected from the 174 samples collected, therefore, this study included 166 samples.
The sample was mostly male (60.20%) with a mean age of 32.66 years, and it was found that most had road accident victims protection 60.20% of the health welfare. 76.50% of the samples occasionally wear a helmet or use a seat belt while driving. Traffic accidents were the leading cause of brain injury for 87.30%, by motorcycles accounted for 96.56% of the total traffic accidents. It was discovered 54.20% had consumed alcohol prior to the accident. Most of the samples had a GCS 15 at admission, 74.70%, who had received computed tomography of the brain, 48.20%, the length of stay for 24-48 hours, and 54.20%.
The River mead Post-Concussion Symptom Questionnaire (RPQ) is divided into two groups, RPQ-3 and RPQ-13. RPQ-3 symptoms and severity decreased in the fourth week after post-brain injury. RPQ-13, the most symptoms were found in the second and fourth weeks, indicating a tendency to increase symptoms (Table 1). Memory loss and amnesia were found in the first 24 hours of 19 samples, representing a percentage of 11.40. However, no samples with amnesia were found in the first, second, or fourth weeks (Table 2).
| Symptom | Duration of symptoms after a traumatic brain injury | |||||||
|---|---|---|---|---|---|---|---|---|
| 24 hrs. | 1st week | 2nd week | 4th week | |||||
| N | % | N | % | N | % | N | % | |
| RPQ-3 | ||||||||
| 1. Headaches | 166 | 100.00 | 151 | 91.00 | 124 | 74.70 | 105 | 63.25 |
| 2. Feelings of dizziness | 133 | 80.12 | 129 | 77.70 | 116 | 69.90 | 105 | 63.25 |
| 3. Nausea or vomiting | 44 | 26.50 | 0 | 0 | 0 | 0 | 0 | 0 |
| RPQ-13 | ||||||||
| 4. Noise sensitivity | 0 | 0 | 1 | 0.60 | 2 | 1.20 | 2 | 1.20 |
| 5. Sleep disturbance | 9 | 5.42 | 77 | 46.38 | 128 | 77.10 | 123 | 71.10 |
| 6. Fatigue | 119 | 71.68 | 112 | 67.46 | 112 | 67.50 | 99 | 59.60 |
| 7. Irritable | 0 | 0 | 1 | 0.60 | 2 | 1.20 | 0 | 0 |
| 8. Depressed | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 9. Frustrated or impatient | 34 | 20.50 | 4 | 2.40 | 2 | 1.20 | 5 | 3.00 |
| 10. Forgetfulness | 1 | 0.60 | 2 | 1.20 | 14 | 8.40 | 72 | 43.40 |
| 11. Poor concentration | 1 | 0.60 | 1 | 0.60 | 7 | 4.20 | 65 | 39.20 |
| 12. longer to think | 1 | 0.60 | 1 | 0.60 | 8 | 4.80 | 26 | 15.70 |
| 13. Blurred vision | 1 | 0.60 | 0 | 0 | 0 | 0 | 0 | 0 |
| 14. Light sensitivity | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 15. Double vision | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 16. Restlessness | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| RPQ-3 Scoring | ||||||||
| Mean (S.D.) | 4.71 (±2.00) | 3.11 (±1.33) | 2.05 (±1.27) | 1.67 (±1.26) | ||||
| Min - Max | 1 - 11 | 0 - 6 | 0 - 4 | 0 - 4 | ||||
| RPQ-13 Scoring | ||||||||
| Mean (S.D.) | 1.94 (±1.50) | 2.19 (±1.75) | 2.16 (±1.64) | 2.77 (±2.04) | ||||
| Min - Max | 0 - 7 | 0 - 6 | 0 - 9 | 0 - 9 | ||||
Table 1.Post-concussion symptoms are classified according to the time since the brain injury
| Post traumatic amnesia | Duration after traumatic brain injury | |||||||
|---|---|---|---|---|---|---|---|---|
| 24 hrs. | 1St week | 2nd weeks | 4th weeks | |||||
| N | % | N | % | N | % | N | % | |
| amnesia | 19 | 11.40 | 0 | 0 | 0 | 0 | 0 | 0 |
| Mean (S.D.) | 68.05 (±4.90) | 0 (0) | 0 (0) | 0 (0) | ||||
| No amnesia | 147 | 88.60 | 166 | 100.00 | 166 | 100.00 | 166 | 100.00 |
| Mean (S.D.) | 88.61 (±7.78) | 98.07 (±4.21) | 98.89 (±3.45) | 98.95 (±3.34) | ||||
Table 2. Post traumatic amnesia
Discussion
A study of mTBI patients with moderate and high risk was conducted in the emergency department and transferred to the trauma ward until discharged. The following are post-concussion symptoms and post-traumatic amnesia. After four weeks, the RPQ-3 group had decreased mean score of symptom severity, while the RPQ-13 group had increased mean score of symptom severity. Post-traumatic amnesia was observed within the first 24 hours and was not shown in the later periods (Table 1).
Findings of a study on mild traumatic brain injury patients with post-traumatic brain injury. Amnesia and post-injury symptoms during the first 24 hours, first week, second week, and fourth week after trauma. The most common symptoms, according to the RPQ [17,18], were headache, dizziness, sleep disorders, fatigue, and frustration, which were consistent with previous studies [7,20]. The symptoms observed in the samples did not occur concurrently. In some cases, the symptoms can be found in the early stages after the injury, while in others, the symptoms worsen late stage after the injury. RPQ-3 symptoms included headache, dizziness, nausea, and vomiting, which were most common in the first 24 hours after injury [18]. However, symptoms will decrease over time. The analysis of the RPQ-3 severity comparison results revealed that there was a difference in each period. Until the fourth week, the severity of the onset of symptoms gradually decreased (Table 3). They are anxious, frustrated, and stressed about the situation because of the early stages of injury. They did not get enough rest while in the hospital. Over time, patients understand their health and are able to manage their problems, resulting in a decrease in the severity of their physical symptoms. It was also found that the decrease in physical symptoms was a self-recovery process [21]. We only found nausea and vomiting during the first 24-hour period, explaining that vomiting is a symptom that indicates the possibility of brain abnormalities [4, 5]. An increase in intracranial pressure indicates. For example, when nausea and vomiting occur more than twice, according to Monroe and Kelly's theory (Monroe-Kellie doctrine), when intracranial volume changes, increased intracranial pressure results. The vomiting center is activated when the Medulla oblongata of the brain is pressed [22]. 9% of vomit patients with mild traumatic brain injuries had abnormalities on computed tomography of the brain [5]. There were 34 samples with abnormal brain computed tomography results, indicating cerebral hemorrhage, and most of the samples noticed nausea and vomiting. When the cerebral hemorrhage was resolved or treated. As a result, there was no later nausea or vomiting. RPQ-13 is detected in the late stages of injury [18]. Most of the symptoms appeared after the second week after the injury and tended to increase in severity (Table 3). The samples perceived an increase in the severity of symptoms in the fourth week, such as sleep disorders, forgetfulness, poor concentration, longer thinking, and noise sensitivity. When the patient returns to normal life, such as returning to work or studying, those activities necessitate increased consciousness and concentration. The patients were aware of the severity of their symptoms, which is consistent with the adverse reaction theory of Lenz et al [23]. The influencing factor is the interaction of physiologic, psychological, and situational factors, which results in symptoms or syndromes. On the other hand, they have an impact on individual expression, which includes cognitive functioning, physically as well as socially. The study found that sleep disorders. It is a common symptom associated with traumatic brain injury. The sample had insomnia, which was consistent with the previous study. Insomnia was found in 50% of them [24]. However, the feeling of frustration or impatience, which was a symptom in the RPQ-13 group, was discovered within the first 24 hours of the injury and persisted throughout the fourth week. Patients have acknowledged their medical conditions, injuries, and treatment plans, including medical expenses. This results in the onset of ongoing symptoms following the injury.
| Source | Sum of Squares | df | Mean Square | F | p-value |
|---|---|---|---|---|---|
| RPQ-3 | |||||
| Time | 921.084 | 1.726 | 533.648 | 364.969 | <.001* |
| Error time | 416.416 | 284.793 | 1.462 | ||
| RPQ-13 | |||||
| Time | 61.861 | 2.647 | 23.374 | 16.580 | <.001* |
| Error time | 615.639 | 436.680 | 1.410 |
Table 3. Repeated measure ANOVA of mean severity scores, RPQ-3 and RPQ-13 in first 24 hours, first week, second week, and fourth week after injury (N=166)
According to the study, the following post-concussion symptoms were not found in the sample: depression, light sensitivity, double vision, and restlessness, which is consistent with previous research [20]. Only 11.40% of patients had post-traumatic amnesia in the first 24 hours after injury (Table 1). Amnesia has been reported in samples with mild traumatic brain injury following head trauma, with abnormal brain computed tomography results accounting for 3-13% [5]. So the first, second, and fourth weeks were when the sample returned home and stayed with relatives. The date, time, and location were obtained, and the memory of the accident was reviewed. Which recovered faster, which was consistent with a study in traumatic brain injury patients with post-traumatic amnesia? Being stimulated by a nurse's orientation to the date, time, and location reduced short-term memory more than the control group [25].
Limitations
According to the study, eight samples were not collected due to the assessment in the first 24 hours after injury. There were no signs of post-concussion symptoms and post-traumatic amnesia. The patients were inconvenienced by being given information and being able to return to their normal lives without experiencing any abnormal symptoms. As a result, no additional symptoms were reported. Because they were a follow-up in the following three times, it was impossible to collect complete data.
RPQ is a widely recognized measurement. There was also a limitation on depression symptoms in this study due to an assessment or symptom reporting by samples that were given but did not have symptoms. As a result, no symptoms were reported. Specific depressive assessment tools should be used in the future.
Conclusion
A study of mild traumatic brain injury patients from the ED admitted to the trauma ward and followed up on for the first 24 hours, first week, second weeks, and fourth weeks after injury. The incidence and severity of RPQ-3 and RPQ-13 were different for each group as well as the time after brain injury. Amnesia appears within 24 hours of a traumatic event. These findings could be used in discharge planning and continuing care referrals.
Acknowledgments
The researcher would like to thank all the sample groups who took the time to participate in the questionnaire and staff from the Accident and Emergency Department Surgical trauma wards at two tertiary care hospitals in Khon Kaen province who cooperated in researching to complete the research. The study received approval from both the Khon Kaen University Ethics Committee for Human Research, with certification number HE651114, certified on May 11, 2022, and the Khon Kaen Hospital Human Research Ethics Committee. On June 11, 2022, the research project code KEMOU65016 was approved.
- Dewan MC, Rattani A, Gupta S, Baticulon RE, Hung YC, et al. (2018) Estimating the global incidence of traumatic brain injury. J Neurosurg; 130(4):1080-1097.
- Taylor CA, Bell JM, Breiding MJ, Xu L (2017) Traumatic brain injury–related emergency department visits, hospitalizations, and deaths—United States, 2007 and 2013. MMWR Surveill Summ; 66(9):1.
- Teasdale G, Jennett B (1974) Assessment of coma and impaired consciousness: a practical scale. Lancet; 304(7872):81-4.
- Vaniyapong T, Patumanond J, Ratanalert S, Limpastan K (2019) Clinical indicators for traumatic intracranial findings in mild traumatic brain injury patients. Surg Neurol Int;10.
- Haydel MJ, Preston CA, Mills TJ, Luber S, Blaudeau E, et al. (2000) Indications for computed tomography in patients with minor head injury. N Engl J Med; 343(2):100-5.
- Abdulle AE, de Koning ME, van der Horn HJ, Scheenen ME, Roks G, et al (2018) Early predictors for long-term functional outcome after mild traumatic brain injury in frail elderly patients. J Head Trauma Rehabil; 33(6):E59-67.
- Ponsford J, Nguyen S, Downing M, Bosch M, McKenzie JE, et al (2019) Factors associated with persistent post-concussion symptoms following mild traumatic brain injury in adults. J Rehabil Med; 51(1):32-9.
- Marshman LA, Jakabek D, Hennessy M, Quirk F, Guazzo EP (2013) Post-traumatic amnesia. J Clin Neurosci; 20:1475–1481.
- Weir N, Doig EJ, Fleming JM, Wiemers A, Zemljic C (2006) Objective and behavioural assessment of the emergence from post-traumatic amnesia (PTA). Brain Inj; 20: 927–935.
- Røe C, Sveen U, Alvsåker K, Bautz-Holter E (2009) Post-concussion symptoms after mild traumatic brain injury: influence of demographic factors and injury severity in a 1-year cohort study. Disabil Rehabil; 31: 1235–1243.
- Snell D, Macleod A, Anderson T (2016) Post-concussion syndrome after a mild traumatic brain injury: a minefield for clinical practice. J Behav Brain Sci; 6: 227-232.
- Eisenberg MA, Meehan WP 3rd, Mannix R (2014) Duration and course of post-concussive symptoms. Pediatrics; 133: 999–1006.
- Tator CH, Davis HS, Dufort PA, Tartaglia MC, Davis KD, et al. (2016) Postconcussion syndrome: demographics and predictors in 221 patients. J Neurosurg; 125: 1206–1216.
- Andelic N, Howe EI, Hellstrøm T, Sanchez MF, Lu J, et al. (2018) Disability and quality of life 20 years after traumatic brain injury. Brain Behav; 8: 1-10.
- Faul F, Erdfelder E, Lang AG, Buchner A (2007) G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods; 39: 175–191.
- De Leeuw ED, Hox J, Dillman D (2012) International handbook of survey methodology. Routledge.
- King NS, Crawford S, Wenden FJ, Moss NE, Wade DT (1995) The River mead Post-Concussion Symptoms Questionnaire: a measure of symptoms commonly experienced after head injury and its reliability. J Neurol; 242: 587–592.
- Eyres S, Carey A, Gilworth G, Neumann V, Tennant A (2005) Construct validity and reliability of the Rivermead Post-Concussion Symptoms Questionnaire. Clin Rehabil; 19: 878–887.
- Levin HS, O'Donnell VM, Grossman RG (1979) The Galveston Orientation and Amnesia Test. A practical scale to assess cognition after head injury. J Nerv Ment Dis; 167: 675–684.
- Karr JE, Iverson GL, Berghem K, Kotilainen AK, Terry DP, et al. (2020) Complicated mild traumatic brain injury in older adults: Post-concussion symptoms and functional outcome at one week post injury. Brain Inj; 34: 26–33.
- Nelson LD, Furger RE, Ranson J, Tarima S, Hammeke TA, et al. (2018) Acute Clinical Predictors of Symptom Recovery in Emergency Department Patients with Uncomplicated Mild Traumatic Brain Injury or Non-Traumatic Brain Injuries. J Neurotrauma; 35: 249–259.
- Maskell F, Chiarelli P, Isles R (2006) Dizziness after traumatic brain injury: overview and measurement in the clinical setting. Brain Inj; 20: 293–305.
- Len ER, Pugh LC, Milligan RA, Gift A, Suppe F (1997) The middle-range theory of unpleasant symptoms: an update. ANS Adv Nurs Sci; 19: 14–27.
- Paredes I, Navarro B, Lagares A (2021) Sleep disorders in traumatic brain injury. Neurocirugia; 32: 178–187.
- De Guise E, Leblanc J, Feyz M, Thomas H, Gosselin N (2005) Effect of an integrated reality orientation programme in acute care on post-traumatic amnesia in patients with traumatic brain injury. Brain Inj; 19: 263–269.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at , Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi