Research Article, J Health Inform Manag Vol: 1 Issue: 1
A Transdisciplinary Approach to Healthcare Informatics Practice and Research: Implications for Elder Care with Poly Chronic Conditions
Wan TTH*
Professor and Associate Dean for Research, College of Health and Public Affairs, University of Central Florida, Orlando, USA
*Corresponding Author : Thomas TH Wan
College of Health and Public Affairs, University of Central Florida, Orlando, USA
Tel: 407-823-3678
E-mail: thomas.wan@ucf.edu
Received: March 16, 2017 Accepted: July 04, 2017 Published: July 10, 2017
Citation: Wan TTH (2017) A Transdisciplinary Approach to Healthcare Informatics Practice and Research: Implications for Elder Care with Poly Chronic Conditions. J Health Inform Manag 1:1.
Abstract
Population health management is to target subpopulation groups that have varying healthcare needs. In particular, health care for three categories of elderly patients overburdens the financial and workforce capacities of most communities. One category includes elders with multiple chronic illnesses, living independently. A second category includes elders with functional limitations requiring long-term assistance. Collectively, they comprise 2 to 5 percent of any community. A third category includes elders making transitions across the care continuum, such as moving from a hospital to a rehabilitative facility after surgery. Each patient category presents a unique population group, including common but varying healthrelated problems associated with aging. Thus, their complex needs reflect the design and implementation imperatives for optimizing resources and information exchanges required for enhancing coordinated care.
Keywords: Population health management; Coordinated elder care; Patientcentered care; Health information technology use; Decision support system; Predictive analytics; Transdisciplinary framework; and Health-FINDER system
Introduction
Aging is often associated with the prevalence of chronic conditions. In particular, health care for three categories of elderly patients overburdens the financial and workforce capacities of most communities. One category includes elders with multiple chronic illnesses, living independently. A second category includes elders with functional limitations requiring long-term assistance. Collectively, these two categories of elders comprise 2 to 5 percent of any community. A third category includes elders making transitions across the care continuum, such as moving from a hospital to a rehabilitative facility after surgery. Each patient category presents a unique population group with common and varying health-related problems associated with aging. Their complex needs reflect the design and implementation challenges for designing and implementing a coordinated health delivery system [1].
The growth of the aging population and its demand for chronic care in the globe coupled with a fragmented and poorly coordinated care system have posed threats to health security of the elderly. The opportunities for enhancing care management technologies through health information exchange (HIE) are abound. The need for adopting a patient-centered care modality for seniors and using electronic health records (EHRs) effectively is paramount. The strategic aims of this article are to: 1) Develop a coordinated elder care Health-FINDER system; 2) impart knowledge and skills for integrated care for high-risk elders; 3) provide health information technology (HIT) integration service for primary care physicians and staff for evidence-based care management; 4) design and implement quality improvement initiatives via HIE for elders; 5) prevent and divert inappropriate hospitalization or institutionalization; 6) assist providers with Health-FINDER to promote population health management; 7) engage in interdisciplinary informatics research by partnering with universities and community stakeholders; and 8) leverage the local community, state and federal resources to optimize success of a community-based integrated delivery system. This proposed approach will help channel coordinated care to high-risk seniors requiring acute, sub-acute, and community-based long-term care. Using a transdisciplinary approach and integrating contextual, ecological, and individual determinants into the investigation of variations in health and social service disparities, researchers and practitioners in healthcare informatics and management may form partnerships to promote population health management. This theoretically based development enables scientists to test what works and what doesn’t work in clinical practice. Consequently, the Health- FINDER System could be modulated and disseminated throughout the world. It is through the evidence-based practice and research that clinical and health executive decision-support systems could be formulated and validated. This article outlines eight strategic aims under a transdisciplinary framework to integrate both macro- and micro-level predictors for explaining the variability in personal and population health.
First strategy: Develop a coordinated elder care health- FINDER system
The National Health Information Infrastructure Act stipulates that investment in HIT, including electronic health record (EHR) systems, is critically needed in the United States. [2,3] have confirmed this stipulation. Innovative applications of HIT and HIE may fill the gaps of a fragmented health care system. In addition [4] advocate that barriers to HIT/HIE adoption should be identified and removed. The proposed strategy is a direct response to the need for enhancing the quality of health care and reducing the disparities in health and health care in the United States through meaningful use of EHRs. Thus, relevant information sharing through EHRs may translate data into context-specific information that can empower providers with evidence-based knowledge for improving the practice. Yet, widespread implementation of HIT has been limited because of the lack of knowledge about what types and implementation methods of HIT will improve care management and contain costs for care.
Currently, EHRs have been implemented and used by some physicians who are based solely in hospitals. However, use beyond the hospital-based physicians is not widespread. Massive amounts of patient care data have been gathered, but limited effort has been made to provide information on how to improve health care processes and outcomes. Further, scanty effort has been made to take such information to improve health care and overall patient and population health. Over the past 10 years, concerted efforts have been made to design and implement the concept of patient-centered care through the use of care management technologies [5-7]. In recent years, there has been an explosion of evidence-based medicine and practice. Massive amounts of clinical and administrative data have been gathered. Little has been done, however, to coordinate the relational databases that can generate information for improving health care processes and outcomes. Such systematic information for formulating predictive analytics is needed to build a repository of knowledge for the use of policy decision makers, providers, administrators, facility designers, researchers, and patients. Evidence-based knowledge gives users a competitive edge in making policy, clinical, administrative, and constructional decisions that improve personal and public health [8,9].
An article appearing in the states that practice-based research will generate new knowledge and bridge the chasm between recommended care and improved health [10]. This approach provides a framework for an innovative and meaningful use of resources for moving America to a leadership position in using information technology in education, innovative product development, and effective patientcentered care in the 21st century.
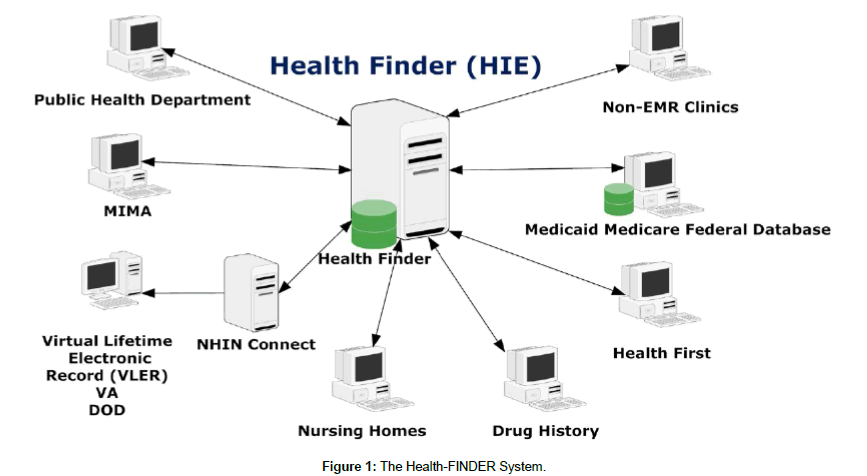
The proposed strategy will shape the analytic work on massive amounts of existing patient-care data to design a patient-centered care management technology model that will be used to coordinate and enhance patient care. This model will rely on EHRs and will include an innovative HIE system integration called Health- FINDER. The integration technology will interoperate with existing data sources, rather than draw down resources to create a new EHR. Health-FINDER will be the hub of the HIE integration solution. It will leverage resources from multiple stakeholders to optimize the system’s success. Strategically, it strives to serve the public good and community welfare, provide positive economic and health impacts on the community, and establish a strong collaboration among all participants and stakeholders. The creation of the Health-FINDER system will achieve several objectives (Table 1). It will need to pull patient and administrative data into a repository, giving a single view to the multiple interdependent back-end data sources that already exist, such as the EHR, drug history, etc. An integrated software is used to design coordinated care modules, monitor and evaluate performance of the subsystems and components, and enhance interoperability to increase meaningful use of EHRs.
| Strategic Aims | Objectives | Metrics |
|---|---|---|
| • Develop a Health-FINDER system for coordinated elder care | • Pull patient & administrative databases into a Master Person Index (MPI) • Use integration modeling software to design coordinated care modules • Monitor & evaluate performance of subcomponents of the system • Build workflows to reach interoperability & meaningful use of EHRs |
• Baseline & then increase completeness of information held in MPI • Level of integration of multiple data sources • Baseline & then increase the percentage of use of the Health FINDER system |
| • Impart the knowledge & skills essential for integrated care for a high-risk group of elders with multiple chronic conditions | • Configure innovative case management technology • Incorporate patient-centered care technologies for primary care • Perform & deliver coordinated care via application system |
• Baseline & then increase number of participants in database • Increase adoption rate • Hit nationwide meaningful use targets established for 2015 • Baseline & then increase user satisfaction with coordinated care • Increase number of services provided |
| • Provide IT integration service through which primary care physicians & staff apply evidence-based care management technologies | • Incorporate patient-centric care technologies for primary care • Apply integrated health & social services to the frail elderly • Increase care coordination & referral networks |
• Adequacy of patient-centered care management technology used • Formal evaluation results • Baseline & increase patient assessment & outcome measures |
| • Design & implement quality improvement initiatives via HIE | • Monitor & assess the project outcomes • Determine the level of satisfaction with coordinated care by users & providers • Identify tractable outcomes relevant to the project • Formulate strategies & plans for continuous improvement |
• Disease-specific outcomes • Adequacy of the quality improvement (QI) plan • Adequacy of the feedback from physician participants • Change in practice for better outcomes • Participation rate of QI activities • Reduce medical errors & treatment problems • Other patient safety measures (poly-pharmacy or drug interaction incidents) |
| • Prevent & divert inappropriate institutional care for the eligible | • Channel coordinated care to high-risk patients who are likely to be institutionalized. • Detect barriers to community-based care • Avoid premature institutionalization |
• Decrease number of skilled nursing facility (SNF) days • Decrease number of repeated visits at clinics • Reduce readmissions |
| • Promote population health in assisting health providers to use Health-FINDER system | • Use syndromic surveillance modeling to establish early warning systems for the outbreak of infectious diseases • Apply GIS techniques to identify service needs • Achieve an optimal return for patient education |
• Reduce number of sentinel health events • Reduce number of ambulatory care sensitive conditions reported |
| • Engage interdisciplinary health informatics research by partnering with community stakeholders | • Design & execute scientific studies • Disseminate research & evaluation studies • Foster the partnership between the academic & community stakeholders • Train health informaticians/ informaticists |
• Number of published papers/book chapters/books generated from healthcare informatics & management research • Number of professional presentations • Frequency of consultations to other organizations or communities |
| • Leverage federal, state & local community resources & assets to optimize the success of the proposed project | • Serve the public good & community welfare • Enhance the visibility of the partnerships • Make economic & health impacts on the community we serve • Establish a strong collaboration with the community & other organizations |
• Connectivity with other HIT systems • Shared use rate • Joint projects developed • Ability to coordinate with multiple entities that are interested in applying HIT/HIE innovations • Regional & national recognition |
Table 1: A Summary of strategic aims, objectives and metrics for evaluation.
Second strategy: Impart knowledge and skills for integrated care for high-risk elders
An overarching goal of the health information system design is to improve the care of seniors with poly chronic illnesses by giving their care providers and managers better access to patient information through an innovative health information exchange system. Primary objectives for this system design are to: 1) improve patient-care outcomes and reduce costs for elders by improving the effectiveness and efficiency of their coordinated care through the use of a federated information network and data electronic retrieval (Health- FINDER) system that interoperates with existing data sources, to share and exchange patient information; 2) enhance best practices in clinical care for elders through simulated learning of clinical case reviews; and 3) promote population health management by using web-enhanced health-education modules for chronic conditions (Figure 1). To encourage the use of innovative care management technologies is to impart knowledge and skills essential for integrated care for a high-risk group of elders with multiple chronic conditions. The high-risk patient population can be identified via the construction and use of frailty index such as a combination of the Activities of Daily Living Scale and the Instrumental Activities of Daily Living Scale, noted as ADL15 [11,12], by employing predictor tree analysis or similar analytical methods. Hopefully, mutually exclusive subpopulations could be singled out as target groups for specific interventions. In other words, a one-size-fits-all intervention approach is undesirable since a diverse group of patient populations may reveal varying service needs and interventions required for achieving optimal health and management of chronic conditions.
Third strategy: Provide Health Information Technology (HIT) integration service for primary care physicians and staff for evidence-based care management
By incorporating patient-centered care technologies for primary care, the performance and delivery of coordinated care solutions are enabled. IT integration service will facilitate primary care physicians and staff to apply evidence-based care management. This will require incorporation of patient-centered care technologies, enabling care givers to apply integrated health and social services to the frail elderly. Further, it will enhance care coordination and referral network utilization [13].
Fourth strategy: Design and implement quality improvement initiatives via HIE for elders
A small number of studies have been conducted to examine HIT effectiveness and impact and/or EHR outcomes [14,15]. Although the studies do not permit definitive assessments of either HIT or EHR outcomes, they do point to the potential for both as a qualityof- care strategy, while acknowledging a developmental curve for the technologies, which have yet to achieve optimal use [16,17]. To that end, innovative applications of HIT and meaningful use of EHRs, deployed within a rigorous evaluation framework should advance our knowledge and move us towards greater optimization while closing critical gaps in context-specific information and practice [18] reviewed the literature on the definition, structure, content, use, and impacts of EHRs and recommended: 1) the needs and requirements of different users should be taken into account in the future development of information systems; 2) different kinds of standardized instruments, electronic interviews, and nursing documentation systems should be included in EHR systems; 3) the completeness and accuracy of different data components should be checked and validated by health care professionals; 4) EHRs should provide important information for health policy planning; and 5) the use of international terminologies is essential to achieve semantic interoperability. The challenge for implementing and diffusing HIT/HIE innovations is further complicated by personal and organizational barriers as noted in the development of EHRs.
The quality improvement initiatives via HIE enable system users to monitor and assess patient care outcomes, determine the level of satisfaction with coordinated care by users and providers, identify tractable outcomes relevant to the system, and formulate strategies and plans for continuous improvement. The FINDER-Based HIE system serves several purposes. One purpose is to prevent and divert inappropriate institutional care for eligible patients. Using the HIE system developed for the elderly, we will channel coordinated care to high-risk patients who are likely to be institutionalized; we will also detect barriers to community-based care, advancing the goals of community care and delivered in the least restrictive environments. The HIE system will seek to avoid premature institutionalization, serving the goal of reducing institutional costs and burdens. The net effect will be to promote population health management. The system supports providers in achieving this goal by assisting them with training, technical assistance, and support to use the Health- FINDER system. To monitor and evaluate quality usage, we could use syndromic surveillance modeling to establish early warning systems for the outbreak of infectious diseases or newly emerging health problems, and to apply GIS techniques to identify services needs and achieve an optimal return in patient education.
Fifth strategy: Prevent and divert inappropriate hospitalization and institutionalization
Since 2015, the Centers for Medicare and Medicaid Services has launched an important initiative called Hospital Penalty Policy for Readmissions [19]. This policy has a significant potential to reduce readmission rates for heart failure, diabetes, joint replacement, and other chronic conditions. However, thoroughly designed and executed systematic reviews and meta analyses are needed to tease out the relevance of human factors that are likely affecting hospitalization or institutionalization for chronic conditions [20].
Sixth strategy: Assist providers with health-FINDER to promote population health management
It is imperative that Patient-Centered Care Management Technology (PCCMT) manages chronic diseases and the associated financial and social impact on individuals, families, organizations, and society better than the current system, which is fraught with high costs and low effectiveness. The PCCMT model depicts a patientcentered care system acting as a well-versed family medical social navigator trained to guide them through their health care choices and coordinate provider care. In the manner of a decision support ‘navigator’ tool that straddles family medical care and social services, the system can manage a multitude of patient-care needs from appointments to proper health education and case management. This multi-dimensional, coordinated approach to care with a patientcentered focus is greatly needed to fill a significant and troublesome gap in the information systems architecture of today, which remains fragmented and relatively ineffective at the cost of the health care system performance, and ultimately, population health management. Indeed, the National Academy of Engineering and Institute of Medicine states: “given the complexity of health care delivery, which involves the coordination and management of large numbers of highly specialized, distributed personnel, multiple streams of information, and material and financial resources across multiple care settings, it is astounding that health care has not made better use of the design, analysis, and control tools of systems engineering” [21]. This view, deploring the under-utilization of systems engineering was reinforced [22], who then addressed the conditions for development of a better organized, high-performing health care system. The performanceenhancing conditions posited by Lee and Mongan involved coordination and monitoring architecture of the type proposed here.
In 2003, the Institute of Medicine identified the deficiencies in health care and made continuity of care a primary goal of its comprehensive call for transforming the quality of care in the United States [23]. In 2006, the American College of Physicians (ACP) established continuity of care as a central theme for restructuring or reengineering health care. Recent research of life-limited patients receiving patient-centric care management showed a notable 38% reduction of hospital utilizations and a 26% reduction of overall costs with high patient satisfaction [24]. Thus, it is imperative to establish scientific evidence in support of the need for expanding EHR/ Patient Health Records (PHR) as part of the patient-centered care management technology.
Seventh strategy: Engage in interdisciplinary healthcare informatics research by partnering with universities and community stakeholders
The conduct of interdisciplinary healthcare informatics research is needed by partnering with community stakeholders [13]. Collectively, we will design and execute scientific studies, disseminate research and evaluation studies, and foster a partnership between the academic and community stakeholders. The academic institution affiliated with a medical center is in a unique position to provide both systems engineering knowledge and tools, and extensive practical experience in the design, testing, validation, and maintenance of complex human-centered and community-centered IT health care systems. Furthermore, it is imperative to employ a comprehensive framework, such as a transdisciplinary approach, to guide the selection of variables from the data files and to generate useful and meaningful knowledge for optimizing clinical practice and improvement.
The realization of an advanced patient-centered health IT infrastructure necessitates faithful adherence to systems-engineering best-practices for complex socio-technical systems design. These practices ensure that 1) the right system is designed, 2) the system performs over its entire design life as expected, and 3) the system is designed, developed, used, maintained, and replaced at minimum cost. Two approaches play a critical role in shaping the program activities: simulation-based concept exploration and model-based systems architecting. Fundamental information technology problems have been observed at the personal, organizational, and community levels for which properly designed and coordinated EHRs can provide meaningful solutions; that is, solutions that are effective, robust, and sustainable. The meaningful use of EHRs is contingent upon multiple factors, including 1) the integrity and coverage of the information system, 2) the graphical-user interface design, 3) interoperability and standardization, 4) security and privacy concerns, and 5) the cost. The ready availability of open-source software and integrators enables the development and implementation of a patient-centered care management technology modality that is needed to coordinate and enhance care for the elderly. It is imperative to reconfigure and integrate massive amounts of patient-care data into an interoperable system in order to effectively and efficiently deliver integrated patient data.
Eighth strategy: Leverage the local community, state and federal resources of partners to optimize success of a community-based integrated delivery system
The partners should be guided by strong scientific and community advisory boards that can facilitate both community engagement and scientific investigations of HIT/HIE demonstrations [25] (physician at the Medical Specialists, Inc., in St. Augustine, Florida) designed a patient-centered care model for rural clinical practices. A health navigator was included and supported by an EMR system to perform coordinated care services for the clinical population with diverse ethnic and racial backgrounds. The patient flow shows how clinical care is rendered, and outcomes are tracked in an integrated computing system. This demonstration project was partially supported by the Florida Blue Foundation to assess clinical outcomes for diabetes. In addition, [6] conducted a thorough evaluation of 400 community health centers’ performance in terms of technical efficiency and financial success and failure. The analysis clearly indicates the need to develop an executive decision-support system to enhance the performance of community health centers.
Evaluation of the Proposed Patient-Centered Care for Elders
A patient-centered care modality for delivering population health management should target elder care first, and then expand to primary care for the general population in the community. The outcome variables are evidence-based valid and reliable (www.ncqa.org) indicators that serve as observable variables to measure safety, effectiveness, efficiency, equity, timeliness, and patient centeredness. In the primary care setting, for example, effectiveness can be measured by HEDIS scores (i.e., A1c, blood pressure, and cholesterol) and frequency of ER visits, hospitalizations, mortality, morbidity, quality of life (QOL), health status, safety by prescription errors, and equity by patient satisfaction surveys, timeliness by waiting time for new/ follow-up appointments, waiting time in provider’s office, efficiency by cost of care, equity by patient survey, and patient-centeredness by patient satisfaction surveys. Table 2 provides details regarding the outcome variables and their relationship to the three major constructs (e.g., access, quality, and cost) in the quality improvement arena.
| PERFORMANCE MEASUREMENT | ||||
|---|---|---|---|---|
| PATIENTS | PROVIDERS | COMMUNITY | ||
| A C C E S S |
Timeliness (reducing waits and sometimes harmful delays for both those who receive care and those who give care) | 1. Patient Satisfaction Survey with > 80 % “Satisfied” (Press- Ganey). 2. Time for new appointment. 3. Open versus closed access. 4. Wait time in office for established patient. 5. Wait time in office for walk in patient. 6. Door to door time. 7. Time to complete referrals. 8. Sample Chart Audit. | 1. Provider Satisfaction Survey with > 80 % “Satisfied.” 2. Sample Chart Audit. | 1. Stakeholder Satisfaction Survey with > 80 % “Satisfied” (Press-Ganey Survey [26]). 2. Sample Chart Audit. |
| Patient Centeredness (providing care that is respectful and responsive to individual patient preferences, needs and values, and ensuring that patient values guide all decisions) | 1. Patient Satisfaction Survey with > 80 % “Satisfied” (Press- Ganey). 2. Sample Chart Audit. | 1. Provider Satisfaction Survey with > 80 % “Satisfied.” 2. Sample Chart Audit. | 1. Stakeholder Satisfaction Survey with > 80 % “Satisfied” (Press-Ganey). 2. Sample Chart Audit. | |
| Q U A L I T Y |
Effectiveness (providing services based on scientific knowledge to all who could benefit and refraining from providing services to those unlikely to benefit-avoiding underuse and overuse respectively) | 1. HEDIS 2007 Scores for Physician practice (NCQA). 2. Health status (SF12). 3. Quality of life (Duke QOL). 4. Patient Satisfaction Survey with > 80 % “Satisfied” (Press- Ganey). 5.Sample Chart Audit. | 1. Provider Satisfaction Survey with > 80 % “Satisfied”. 2. Sample Chart Audit. | 1. HEDIS 2007 Scores for Physician practice (NCQA). 2. Stakeholder Satisfaction Survey with > 80 % “Satisfied” (Press-Ganey). 3. Sample Chart Audit. |
| Safety (Avoiding injuries to patients from care that is intended to help them) | 1. HEDIS 2007 Scores for Physician practice (NCQA). 2. National Patient Safety Foundation Survey. 3. Patient Satisfaction Survey with > 80 % “Satisfied” (Press- Ganey). 4. Sample Chart Audit. | 1. Provider Satisfaction Survey with > 80 % “Satisfied.” 2. Sample Chart Audit. | 1.Stakeholder Satisfaction Survey with > 80 % “Satisfied” (Press-Ganey). 2.Sample Chart Audit. | |
| Equity (providing care that does not vary because of personal characteristics such as gender, ethnicity, geographic location, and socioeconomic status) | 1. Patient Satisfaction Survey with > 80 % “Satisfied” (Press- Ganey). 2. Sample Chart Audit. | 1. Provider Satisfaction Survey with > 80 % “Satisfied.” 2. Sample Chart Audit. | 1.Stakeholder Satisfaction Survey with > 80 % “Satisfied” (Press-Ganey). 2. Sample Chart Audit. | |
| C O S T |
Efficiency (avoiding waste, including waste of equipment, supplies, ideas and energy) | 1. Cost per outpatient encounter (FQHC data from BPHC division of CMS and MGMA data). 2. Number of encounters. 3. ER Visits and Hospitalizations. | 1. Cost per outpatient encounter (FQHC data from BPHC division of CMS and MGMA data). 2. Number of encounters. | 1. Stakeholder Satisfaction Survey with > 80 % “Satisfied” (Press-Ganey). 2. Sample Chart Audit. |
Table 2: National health goals and the associated observable variables.
Cost efficiency metrics should be gathered to demonstrate the reduction in the cost of care associated with the Health-FINDER system. These include: 1) preventable emergency room visits and hospitalizations, including readmissions; and 2) reduced short-term skilled nursing home stays following a hospital stay. The integrated data system will merge a variety of data sources, such as hospital discharges, readmissions, nursing home use, ambulatory care visits, prescription drug purchase and use, and other durable equipment leased or paid. A list of inputs (resources/services used in terms of costs) and outputs (functional outcomes and health-related quality of life indicators) has been identified to perform efficiency analysis and identify the efficiency frontiers as a guide to optimize the performance of health services organization. Again, for illustrative purposes, the targeted disease, type 2 diabetes, is highly prevalent and could be effectively treated at non-institutional settings such as primary care clinics. Patients afflicted by the disease are at a highrisk for hospitalization and poly chronic conditions. A large amount of savings can be generated from the deployment of the proposed patient-centered care modality, as well as the health information technology and simulated learning software (e.g., a web-based decision support system design).
Concluding Remarks
The implementation of a functional and integrated health information system has to be guided by a theoretically-informed framework. Thus, the appropriately collected data could produce useful information and evidence-based knowledge to promote health services outcome and quality improvement. Measurable patientcare outcomes and their benchmarks should be used to evaluate the system’s performance. The multi-site evaluation of a patient-centered care model should be guided by the structure-process-outcome perspective has been developed [26,27]. We should use clinical and administrative data to prescribe best-performance practices based on research evidence. Analysis of clinical and administrative data should be planned to determine factors contributing to improved performance. Analysis can be performed in terms of improved patient outcomes, patient cost, quality of care, and patient safety based on measured performance comparing intervention to controls. The results could serve as a sound evidence-based prescription for performance monitoring and feedback. Knowledge management techniques ensure the right people are receiving the right information at the right time via the right method to ensure the right care plan. The ultimate test of the system is to enhance the ability to use current data to make safe clinical decisions and then track both self-reported and objectively assessed outcomes of those decisions to continue to inform decision-making lies at the epicenter of knowledge management. The more innovative the technology applied, the more flexible and boundless the options to refine efficiency and effectiveness.
In conclusion, two important issues pertaining to the data management and use should be further addressed by the collaborative parties who have generated and collected the data. First, a data governance platform or mechanism should be established to ensure the privacy and security of data gathered. This mechanism should serve as a gatekeeper for the data use and authorization. Researchers should formally submit a formal request for gaining access to the data and provide research reports to the agency designated for this purpose. Second, patients and their providers should have access to person-specific data as part of the personal health records.
References
- Wan TTH (2011) Impacts of health information technology adoption on patient and population health: Designing a health-FINDER system for elder care. Proceedings of INTED2011 Conference.
- Institute of Medicine (2001) Crossing the quality chasm. National Academy Press, Washington DC.
- Institute of Medicine (2006) Improving the quality of health care for mental and substance-use conditions: Quality chasm. National Academies Press, Washington, D.C.
- Institute of Medicine (2009) Crossing the quality chasm: The IOM health care quality initiative
- Breen J, Wan TTH, Zhang NJ, Marathe S (2009) Doctor-patient communication: examining innovative modalities vis-à-vis effective patient-centric care management technology. J Med Syst 33: 155-162.
- Marathe S, Wan TTH, Zhang JN, Sherin K (2007) Factors influencing community health centers’ efficiency: A growth curve modeling approach. J Med Syst 31: 365-374.
- Wan TTH, Lin YJ, Ma A (2002) Integration mechanisms and hospital efficiency in integrated healthcare delivery systems. J Med Syst 26: 127-143.
- Wan TTH (2002) Evidence-based Health Care Management. Kluwer Academic Publishers, Norwell, MA.
- Wan TTH, Connell AM (2003) Monitoring the quality of health care: Issues and scientific approaches. Kluwer Academic Publishers, Norwell, MA.
- Westfall JM, Mold J, Fagnan L (2007) Provider-based research: Blue highways of NIH roadmap. J Am Med Assoc 297: 403-406.
- Drubbel, I,Wit NJ, Bleijenberg N, Eijkemans RF, Schuurmans MJ, et al. (2012) Prediction of adverse health outcomes in older people, using a frailty index based on routine primary care data. J Gerontol (Series A Biomedical Science) 68: 301-308.
- Clegg A (2016) An electronic frailty index (eFI) developed at the Leeds Institute of Health Science based on data from 1 million patients in United Kingdom.
- Wan TTH (2006) Healthcare informatics research: From data to evidence-based management. J Med Syst 30: 3-7.
- Wan TTH (1989) The effect of managed care on health services use by dually eligible elders. Med Care 27: 983-1000.
- Wan TTH, Lin YJ, Wang BBL (2004) The effects of care management effectiveness and practice autonomy on physicians’ practice and career satisfaction. Chronic Care, Health Care Systems and Services Integration. Research in the Sociology of Health Care. Elsevier, New York.
- Lee K, and Wan TTH (2004) Information system integration and technical efficiency in urban hospitals. Int J Healthcare Technol Manage 5: 452-462.
- Lee K, and Wan TTH (2002) Effects of hospitals’ structural clinical integration on efficiency and patient outcome. Health Serv Manage Res 15: 234-244.
- Häyrinen K, Saranto K, Nykanen P (2008) Definition, structure, content, use and impacts of electronic health records: A review of the research literature. Int J Med Inform 77: 291-304.
- Wan TTH, Ortiz J, Du A, Golden A (2017) Variations in rehospitalization of rural Medicare beneficiaries. Health Care Manage Sci 20: 90-104.
- Wan TTH, Terry A, Cobb E, McKee B, Tregerman R, et al (2017) Strategies to modify the risk of heart failure readmission: A systematic review and meta analysis. Health Services Research-Managerial Epidemiology pp: 1-15.
- Reid P, Comptom W, Grossman J, Fanjiang G (2005) Building a better delivery s ystem: A New Engineering/Health Care Partnership. National Academy of Engineering and the Institute of Medicine. The National Academies Press, Washington, D.C.
- Lee TH, Mongan JJ (2009) Chaos and organization in the health care, Massachusetts Institute of Technology, The MIT Press, Cambridge, UK.
- Institute of Medicine (2003) Health professions education: A Bridge to Quality. National Academies Press, Washington, D.C.
- Sweeney L, Halpert A, Waranoff J (2007) Patient centered management of complex patient s can reduce costs without shortening life. Am J Manag Care 13: 84-92.
- Wan TTH, Rav-Marathe K, Marathe S (2016) A systematic review on the KAP-O framework for diabetes education and research. Medical Research Archives 3: 1-22.
- Press Ganey Patient Experience Survey (2017).
- Donabedian A, Ann Arbor (1980) The Definition of quality and approaches to its assessment, Health Administration Press, MI, US.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi