Case Report, J Clin Image Case Rep Vol: 1 Issue: 2
Adnexal Torsion in Early Pregnancy: The Diagnostic and Management Challenges: A Case Report and Literature Review
Felix Mwembi Oindi1* and Abraham Mwaniki Mukaindo2
1Resident, Department of Obstetrics and Gynecology, Aga-Khan University, Nairobi, Kenya
2Consultant Obstetrician and Gynecologists, Department of Obstetrics and Gynecology, Aga-Khan University, Nairobi, Kenya
*Corresponding Author : Felix Mwembi Oindi
Department of Obstetrics and Gynecology, Aga Khan University, Nairobi, PO Box 30270-00100, Kenya
Tel: +254 723 499 586
E-mail: droindi@gmail.com
Received: August 10, 2017 Accepted: August 31, 2017 Published: September 07, 2017
Citation: Oindi FM, Mukaindo AM (2017) Adnexal Torsion in Early Pregnancy: The Diagnostic and Management Challenges: A Case Report and Literature Review. J Clin Image Case Rep 1:2.
Abstract
Introduction: Adnexal torsion (AT) is a gynecologic emergency with a nonspecific presentation especially in pregnancy. Given the serious implications of delayed therapy on ovarian function and maternal morbidity, the diagnosis of AT should be considered in all pregnant women presenting with acute lower abdominal pain. We present a case of AT complicating an early pregnancy and further delve into literature to highlight the challenges encountered in the management of AT in early pregnancy.
Case Report: A 26 year old priming ravida presented at 8 weeks gestation with acute right sided low abdominal pains for 2 day duration. Her subsequent workup suggested AT necessitating a laparoscopic evaluation where right adnexectomy was carried out due to hemorrhagic and necrotic changes. She was subsequently put on progesterone therapy though she suffered a miscarriage on the 5th day following the surgery. She recovered well from the surgery.
Conclusion: Adnexal torsion is a serious gynecologic emergency in pregnancy. It should be suspected in all cases of acute abdominal pain in pregnancy alongside the other differentials. Early operative intervention should be instituted preferably by laparoscopy in order to preserve ovarian function.
Keywords: Adnexal torsion (AT); Low abdominal pain; Adnexectomy
Introduction
Adnexal torsion (AT), defined as twisting of the ovary and the fallopian tube, is an uncommon gynecologic emergency that can occur in normal pregnancy. It may result in partial or total strangulation of blood supply with possible progression to ischemic necrosis and loss of ovarian function [1]. However, the diagnosis and subsequent management of AT is often delayed in pregnancy with potential deleterious effect on ovarian function and the pregnancy [2]. Timely intervention by detorsion has been demonstrated to result in preservation of ovarian function.
We present a case of a pregnancy complicated by AT and further conducts a literature review to highlight the challenges encountered in managing such conditions.
Case
A 26 year old woman in her first pregnancy presented at 8 weeks gestation, by her last menstrual period date, with severe right side low abdominal pains for 2 day duration. She had associated nausea and vomiting but no fever. The pain was aggravated by movement with mild relief on over the counter analgesics. Significantly, her conception followed fertility treatment for delayed conception (one year) using clomiphene citrate. She had no history of prior medical conditions or surgeries.
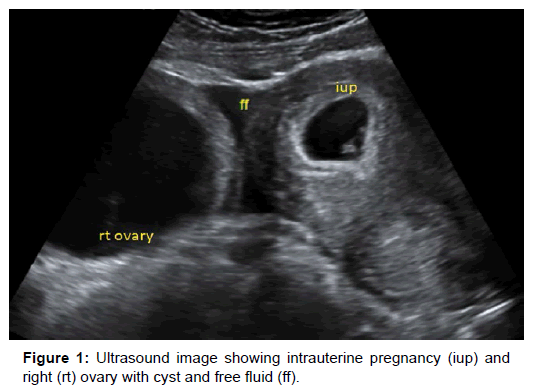
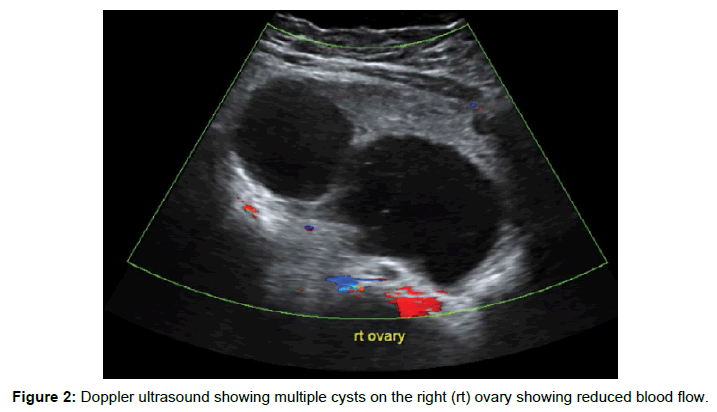
Initial assessment revealed a normal general examination with normal vital signs as shown: blood pressure of 110/60 mm/Hg, axillary temperature of 36.5°C, pulse of 68 beats/minute, respiratory rate of 18 breaths/minute and oxygen saturation 99% on room air. She had mild abdominal distension and tenderness. The laboratory parameters were essentially normal with a white cell count of 7300/ μl, hemoglobin of 12.1 g/dl and hematocrit of 36.7%. The kidney and liver function tests were essentially normal. The pelvic scan showed an early intrauterine pregnancy at 8 weeks gestation (Crown Rump Length of 17.2 mm) and a polycystic right ovary with free fluid in the peritoneal cavity (Figure 1). Doppler assessment revealed reduced blood flow suggesting partial ovarian torsion (Figure 2).
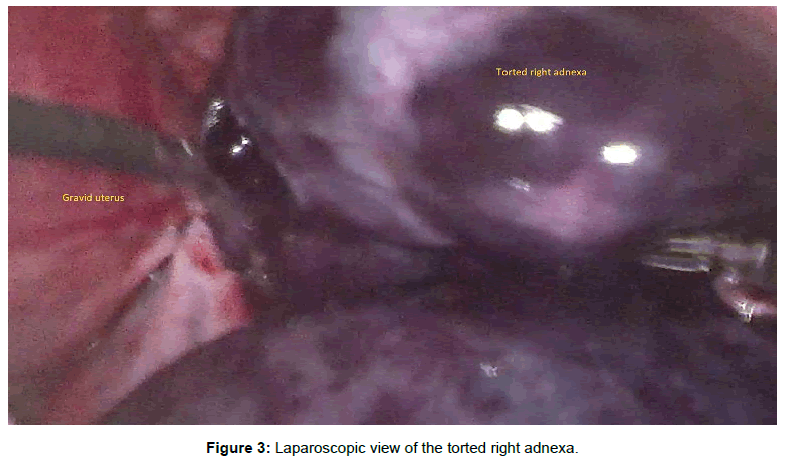
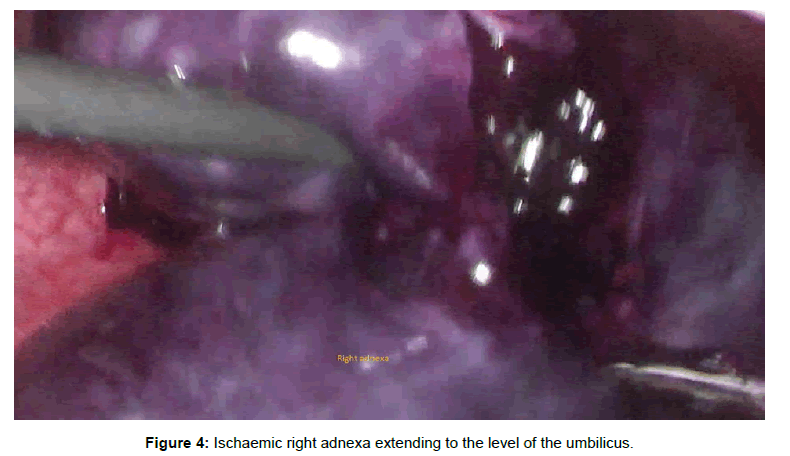
A diagnosis of mild ovarian hyper stimulation syndrome (OHSS) with possible torsion was made in view of the history of ovarian stimulation with clomiphene citrate, the polycystic ovaries and free peritoneal fluid on ultrasonography. The patient was initially put on conservative management with parenteral analgesics and intravenous fluids. However, the symptoms persisted necessitating laparoscopic evaluation for suspected right AT within 12 hours of hospitalization. The right adnexa were found to be torted with a hemorrhagic necrotic appearance (Figure 3) while the left was grossly normal. The torted right adnexa extended to the level of the umbilicus (Figure 4).
Right adnexectomy was subsequently performed and 600mls of blood aspirated. The intraoperative pressure was maintained at 12 mmHg. Her post-operative recovery was uneventful and was put on daily vaginal progesterone (Susten 400 mg). She however developed per-vaginal bleeding from the fifth postoperative day resulting in a complete miscarriage. The subsequent recovery was uneventful and the histo-pathological examination of the surgical specimen confirmed hemorrhagic infarction.
Discussion
AT is a rare cause of acute pelvic pain in pregnancy. It affects around one in every 5000 pregnancies with the highest occurrence in the first and early second trimesters [2]. The present case presented in the first trimester (8 weeks). The compressive effect of the gravid uterus in the late second and third trimesters is partly protective of AT by limiting the mobility of the ovarian pedicle [3]. However, some cases of AT have been reported in the third trimester principally attributed to persistent ovarian cysts [2-4].
The occurrence of AT is increased in the presence of ovarian cysts and neoplasms [1]. Pregnancy in patients known to have ovarian cysts has been shown to be a risk factor for AT [1]. Equally, the development of new ovarian cysts in pregnancy increases the risk of AT. Indeed, conditions known to increase the occurrence of ovarian cysts such as ovulation induction are associated with increased prevalence of AT [1,3]. Our patient presented with a right ovarian cyst that would have potentially increased her risk of developing AT. Moreover, she had used ovulation induction prior to her conception, a known risk factor for the occurrence of ovarian cysts and possible subsequent AT [5,6]. However, despite the polycystic nature of the ovaries, she had no other clinical features of ovarian hyper stimulation syndrome (OHSS) known to occur in a few cases following ovulation induction.
The occurrence of AT, just like in our patient, has a right sided preponderance due to the longer right ovarian ligament and the protective effect of the sigmoid colon on the left adnexa [2,7,8]. The presentation is quite nonspecific with the diagnosis primarily based on a high index of suspicion [9]. It can mimic clinical features of acute appendicitis, degenerated fibroids, renal calculi and obstructive bowel disease [5].
The most common symptom is lower abdominal pain of varying intensity with or without nausea, vomiting, fever and supra pubic tenderness. Nausea and vomiting are common symptoms in pregnancy and may therefore contribute to delays in the diagnosis of AT. The laboratory investigations are equally unyielding with some cases having leukocytosis.
Ultrasound examination is a key tool in the evaluation of adnexal masses in gynecology both during and outside pregnancy [9,10]. Trans-vaginal ultrasonography is the preferred approach in the early pregnancy though combination with the trans-abdominal might be appropriates in a few cases especially those presenting with huge ovarian cysts. The addition of colour Doppler may be a useful adjunct in the diagnosis of AT depending on the stage of vascular compromise [5]. However, even a normal Doppler flow result cannot exclude the possibility of torsion hence the emphasis on having a high index of suspicion.
Suspected AT in pregnancy should be emergently treated. Laparoscopic approach is preferred to laparotomy due to the advantages of shorter hospital stay, reduced adhesion formation, less post-operative pain and ileus hence quicker post-operative recovery [11,12]. As per the Guidelines Committee of the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) recommendation [4], the intraoperative pressure should be maintained at 10-15mmHg. In the present case the intra-abdominal pressure was kept at 12mmHg during the operation. Detorsion should be attempted in all cases of AT followed by cystectomy whenever applicable. However, in a few cases especially where necrosis is identified, adnexectomy may be appropriate to prevent peritonitis and further maternal morbidity [2,8]. In such cases, where the corpus luteum has been removed, progesterone supplementation should be instituted especially in the first trimester [11]. However, as the present case, pregnancy loss may still occur.
In conclusion, AT is a common gynecologic emergency that should be suspected in pregnant women presenting with acute abdominal pain. In order to preserve the functions of the affected organs, early operative intervention preferably by laparoscopy should be performed.
References
- Yuk JS, Shin JY, Park WI, Kim DW, Shin JW, et al. (2016) Association between pregnancy and adnexal torsion: A population-based, matched case-control study. Medicine 95: e3861.
- Passarinho RM, Afonso E, Reis L, Santos SI (2012) Adnexal torsion in third trimester of pregnancy. BMJ Case Reports.
- Vlachodimitropoulou KE, Gupta M, Hollingworth A, Gorry A (2016) Ovarian torsion in the third trimester of pregnancy leading to iatrogenic preterm delivery. Case Reports in Obstetrics and Gynecology 2016: 8426270.
- Kahramanoglu I, Eroglu V, Turan H, Kaval G, Sal V, et al. (2016) Isolated adnexal torsion in a 20-week spontaneous twin pregnancy. International Journal of Surgery Case Reports 23: 138-140.
- Spitzer D, Wirleitner B, Steiner H, Zech NH (2012) Adnexal torsion in pregnancy after assisted reproduction - case study and review of the literature. Geburtshilfe und Frauenheilkunde 72: 716-720.
- Gil Navarro N, Garcia Grau E, Pina Perez S, Ribot Luna L (2017) Ovarian torsion and spontaneous ovarian hyperstimulation syndrome in a twin pregnancy: A case report. International Journal of Surgery Case Reports 34: 66-68.
- Mutiso SK, Mwembi OF (2017) Pediatric ovarian torsion in a nine-year-old girl: A twisted tale of pain. Int J Case Rep Images 8: 348-351.
- Tsai HC, Kuo TN, Chung MT, Lin MY, Kang CY, et al. (2015) Acute abdomen in early pregnancy due to ovarian torsion following successful in vitro fertilization treatment. Taiwanese Journal of Obstetrics & Gynecology 54: 438-441.
- Ginath S, Shalev A, Keidar R, Kerner R, Condrea A, et al. (2012) Differences between adnexal torsion in pregnant and nonpregnant women. Journal of Minimally Invasive Gynecology 19: 708-714.
- Hoover K, Jenkins TR (2011) Evaluation and management of adnexal mass in pregnancy. American journal of Obstetrics and Gynecology 205: 97-102.
- Yakasai IA, Bappa LA (2012) Diagnosis and management of adnexal masses in pregnancy. Journal of Surgical Technique and Case Report 4: 79-85.
- Habek D, Bauman R, Rukavina Kralj L, Hafner T, Turudic T, et al. (2016) Acute Abdomen in the 17th Week of Twin Pregnancy due to Ovarian Torsion - A Late Complication of IVF. Geburtshilfe und Frauenheilkunde 76: 1345-1349.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi