Case Report, J Trauma Stress Disor Treat Vol: 6 Issue: 2
An Introduction to the Background to BART: Bilateral Affective Reprocessing of Thoughts as a Dynamic form of Psychotherapy Including a Case Report on 17-Year-Old Female Victim of Physical and Psychological Abuse
A G O’Malley*
CAMHS Psychiatrist, Mascot Child and Family Services Ltd, 70 Whitehurst roads, Heaton Mersey, Stockport, SK4 3NZ, United Kingdom
*Corresponding Author : A G O’Malley
CAMHS Psychiatrist, Mascot Child and Family Services Ltd, 70 Whitehurst road, Heaton Mersey, Stockport, SK4 3NZ, United Kingdom
E-mail: bart@artomalley.com
Received: January, 18, 2017 Accepted: March 13, 2017 Published: March 20, 2017
Citation: GO’Malley A (2017) An Introduction to the Background to BART: Bilateral Affective Reprocessing of Thoughts as a Dynamic form of Psychotherapy Including a Case Report on 17-Year-Old Female Victim of Physical and Psychological Abuse. J Trauma Stress Disor Treat 6:2. doi: 10.4172/2324-8947.1000168
Abstract
Background: This article describes an integrated form of dynamic psychotherapy, BART, which has components of both top-down reprocessing from EMDR and trauma-focused CBT combined with bottom-up approaches such as somatic experiencing and sensorimotor psychotherapy. The unique components of BART are described, with particular emphasis on the interaction between gut instinct, heartfelt sensation and head thoughts. BART is described in terms of what the individual letters stand for. Information processing at the levels of the gut, the heart and the brain are illustrated anatomically with diagrams of the heart-brain and the gut-brain with the brainstem. The anatomical structure of the gut mesentery is discussed along with the implications for information reprocessing in BART psychotherapy. The path of the vagus nerve is illustrated along with the endocrine system. BART psychotherapists can use knowledge of these structures to lessen the impact of trauma on physical and mental ill health. Compositions of neuroreceptors in the heart-brain or cardiac neural plexus are described. The role of the gastrointestinal tract in processing food and how it deals with emotional reactions are discussed. A link to the insular cortex in each cerebral hemisphere or head-brain is hypothesised as the mechanism of communication between the gut and brain. The influence of the heart’s magnetic field is discussed in relation to BART.
Results: A case example of a 17-year-old girl who has experienced physical and psychological abuse is described. Over three sessions and six hours of BART psychotherapy her symptoms of moderate PTSD are reduced from scores of 53/88 to a normal 21/88 on the revised impact of events scale.
Conclusion: Areas for future development of the theory and practice of BART psychotherapy are discussed.
Keywords: BART psychotherapy; Traumatic stress disorders; Top-down and bottom-up reprocessing; Gut-brain; Heart-brain and head-brain
Introduction
BART is an acronym for bilateral affective reprocessing of thoughts. The first component represents various forms of bilateral stimulation from continuous auditory stimulation at the level of the mastoid processes, just behind each ear, to peripheral tactile stimulation using zappers applied at various frequencies. The second component represents access to the person’s affective experience. Third, in ways that will be explained, repeated iteration of emotions, sensations, and feelings are reprocessed so that, finally, new thoughts emerge (recognition). This allows the patient or client to strive psychotherapeutically towards peak performance, which is the ultimate goal or target of therapy.
BART has been developed by the author over the last eight years and has been used both in a traumatic stress clinic in a range of Child and Adolescent Mental Health Services and in a pilot Parental and Infant Mental Health Clinic set in the Brooker Centre (an in-patient ward for adult psychiatric patients in Halton General Hospital, Runcorn). This last service was a unique collaboration between the author and both Dr Sheena Pollet, consultant psychiatrist in psychotherapy, and Thelma Osborn, specialist in maternal mental health. This service was granted ethical approval by the Department of Adult Mental Health at the 5 Boroughs Partnership NHS Foundation Trust. The service was awarded a staff recognition award by the 5 Boroughs Partnership NHS Foundation Trust and was acknowledged by NHS North West [1] as an example of good practice. The director of Adult Healthcare proposed that the service was nominated for a Health and Social Care Award in 2009. During the three and a half years the service was in operation, I delivered BART psychotherapy mainly to mothers who had experienced significant trauma in giving birth and who had attachment difficulties. I will give feedback from some patients later in this paper. During the last 8 years over 200 patients have been treated with BART psychotherapy. In order to do further research involving a randomized clinical trial, I am planning to recruit a cohort of psychotherapists who have certified training in EMDR, body based therapy such as sensorimotor psychotherapy, somatic experiencing or AEDP (accelerated experiential dynamic psychotherapy) mindfulness or metallization and trauma focused CBT. This will enable these therapists to more easily pick up the fundamentals of BART psychotherapy which is strongly rooted in affective neuroscience and neurobiology.
The technique that BART uses is a combination of top-down processing EMDR and trauma-focused CBT along with bottomup approaches such as somatic experiencing and sensorimotor psychotherapy. Each of the letters in BART conveys a specific component of the psychotherapeutic approach.
B-Bilateral: Bilateral stimulation is applied for the duration of the therapeutic session. This might be 90 minutes for adults and 30-60 minutes for children and adolescents. The patient or client places tactile hand-held buzzers adjacent to the registered area of greatest distress. Commonly, this can be in the region of the gutbrain (abdomen) or heart-brain (chest); it is less likely for the headbrain to be the area of most sensory disturbance among patients. It has been my clinical experience that patients with symptoms of obsessive-compulsive disorder are overwhelmed by thoughts that are experienced as physical discomfort in the orbitofrontal cortex. The therapeutic process here is to start with top-down reprocessing of emotions, sensations, feelings and thoughts. The cerebellum or little brain is known to both dampen down the instinctive impulses generated at a brainstem level. Also according to Randy L. Buckner, 2013, from the University of Harvard [2] showed that most of the fibres from the cerebellum connect with the association cortex. This challenged conventional wisdom that the cerebellum solely contributes to planning and execution of movement. This Bilateral cerebellar stimulation is applied continuously during the session and helps to trigger the brain to be in a trance like or rapid eye movement (REM) state and keep the cerebellum active while the patient is engaged in cognitive, emotional and sensorimotor tasks. Purkinje cells from the cerebellum connect to prefrontal area 46. It was found that most of the human cerebellum is linked to the cerebral association networks. These include an executive control and default mode networks. Schmahmann, [3] hypothesized in relation to the cerebellum: “so may it regulate the speed, capacity, consistency and appropriateness of mental or cognitive processes….the overshoot and inability in the motor system to check parameters of movement may thus be equated, in the cognitive realm, with a mismatch between reality and perceived reality and the erratic attempts to correct the errors of thought or behaviour, perhaps a dysmetria of thought.”
When patients experience the alternating stimulating of bone resonating headphones they report that the thoughts and cognitions inside their head are changed positively. This could be a way to reverse the thought dysmetria proposed by Schmahmann.
A-Affective: Affective refers to a non-conscious experience of intensity that has both unformed and unstructured potential. At the start of the BART psychotherapy process it is difficult to put words on the affective, and the process involves helping the client or patient to scaffold the gut experience or sensation that is experienced at an instinctual level. The patient is asked to recount the traumatic experience in a loose narrative form without exploring the intensity of the experiences, and this allows them patient to stay within their window of affect tolerance and emotional regulation and stabilisation. Then they are asked to play a movie of the events in their mind’s eye to allow the most distressing affect to surface.
Massumi [4] equates affect with intensities: Affect is the body’s way of preparing itself for action in a given circumstance by adding a quantitative dimension of intensity to the quality of an experience. The body has a grammar of its own that cannot be fully captured in language because it doesn’t just absorb pulses or discrete stimulations; it infolds contexts…
Affects are comprised of correlated sets of responses involving the facial muscles, the viscera, the respiratory system, the skeleton, autonomic blood flow changes and vocalisations that act together to produce an analogue of the particular gradient or intensity of stimulation impinging on the organism.
It is with the knowledge of this affective response on the mind, body and soul that the BART psychotherapist begins to delineate the client or patient’s feelings, emotions and/or sensations. These are dealt with by the next stage of the process.
R-Reprocessing: The activation of affect enables the unconscious information to be perceived at a conscious level and typically the information is first felt instinctively as a gut feeling. Patients may use language such as ‘I am sick to my stomach’ and are encouraged to be aware of their breathing. Reprocessing involves revisiting and re-evaluating sensations of loss, unresolved grief, trauma, panic, anxiety and fear until the subjective unit of distress scale (SUDS) has decreased to the extent that the sensations, feelings, emotions or muscle impulses are no longer distressing. Often this can be achieved over a few hours of intense psychotherapy, and some blocks to processing may need to be addressed. For example, the patient may need to return to or retrace the It may be necessary to float back to the first time or the worst time they had the recalled experience. This allows new associations to emerge; and as the buzzers are moved to new bodily locations, the area of the brainstem and thyroid gland becomes activated. This is crucial to helping patients overcome the speechless terror that many patients who are unable to access the speech networks of the left cerebral cortex because of an increased perfusion of blood at the level of the brainstem that is part of the instinctive survival reflex. Many patients describe this as a lump in their throat. This reassures the BART psychotherapist that information registered at a gut and heart level is now ready to be activated from the brainstem and thyroid gland level to the prefrontal cortex.
T-Thoughts: Thoughts are stimulated by the movement of dendritic spines, which bend and sway as if affected by the mechanical sound waves produced by the continuous bilateral cerebellar resonance at the level of the mastoid processes. Forces are transferred between dendritic spines, and their microtubules store energy like a spring. Mechanical stimulation of one dendritic cortical spine is hypothesised to facilitate transfer of cognitive information to the prefrontal cortex where new learning and reflection can occur [5]. Towards the end of the reprocessing session, BART psychotherapy appears to activate thalamocortical binding. The stimulation to achieve this should take place at 40-100 Hz frequency (gamma wavelength). Further research is necessary to identify the optimum frequency of the stimulation requited to achieve this; currently, a frequency in the gamma wavelength range (40-100 Hz) is used. Patients often report tingling sensations at the level of the cerebral cortex towards the end of a 120-minute session. It can be hypothesized that this is related to the development of new neural pathways enhanced by the BART psychotherapy session. Recently the optimum results have been achieved by intensive therapy where a number of sessions approximately over 20 hours of BART psychotherapy are delivered on consecutive days. This resulted in normalization of impact of events scales in relation to complex trauma in the case reports discussed previously.
The relationship between the patient or client and therapist depends a lot on intuition for its effectiveness in helping to establish a therapeutic alliance. This is a key goal of BART psychotherapy and its activation via bilateral cerebellar stimulation. It is also the mechanism whereby the mind perceives either the agreement or disagreement of several ideas. It is how we become aware of the truth of things immediately, without reasoning and deduction. In a “sense”, it is assumed in the body’s experience - the technique of BART psychotherapy is grounded in acknowledging this experience.
There is an increasing awareness of the need to move from chaos towards coherence in the lives of our patients and clients and this can be represented by an integration of the gut-brain, the heart-brain and the head-brain. The organs of the body must cohere (that is, be in close contact) for information to flow freely and to form a connection or coherent mass. In a coherent state, we optimise energetically - that is, emotionally, mentally and physically. The heart-brain, head-brain and gut-brain all synchronise and operate efficiently when they are internally coherent. Synchronicity can be achieved when BART psychotherapy is used - either as a trauma therapy or to enhance peak performance. In the body’s neural networks, about 85-90 per cent of neural fibres travel from the lower body to the brain, especially via the different components of the vagus nerve. These neural pathways dominate our decision-making, our creativity, and our emotional state. During traumatic stress, different forms of information can be blocked at any point along the affected neural pathway.
The basic premise underpinning the mechanism of action of BART psychotherapy is that information is processed in three ways: reactively by the gut-brain, emotionally and subjectively by the heartbrain, and analytically and logically by the head-brain.
The human nervous systems can be conceptualised as the gutbrain, which first registers sensations and feelings as a “gut reaction” or instinct. This is followed by the heart-brain, or sympathetic and parasympathetic nervous system, which registers these sensations and feelings in the chest – for example, those relating to emotions of loss and delayed grief. The central and peripheral nervous systems work together to analyse information, which the head-brain can then formulate as thought and express in speech, which represents the outcome of logical and objective thought and rational analysis. It is the linking of these separate processes that is unique to BART psychotherapy. For example, it is by recognition and inhibition of the sensation of butterflies in the stomach during reprocessing that we can ultimately achieve the objectives of engaging heart-brain and head-brain reprocessing capabilities of both the heart-brain and the head-brain.
The bilateral activation at the level of the mastoid processes resonates at the level of both cerebellums. This information appears to further access processing in the temporal, occipital, and parietal lobes. Finally, patients often report a tingling sensation in their frontal lobes. This appears to coincide with a release of energy from both the third eye and forehead chakras, correlating anatomically with the pituitary and hypothalamic glands. The techniques underlying this process are explained further in The Art of BART [6].
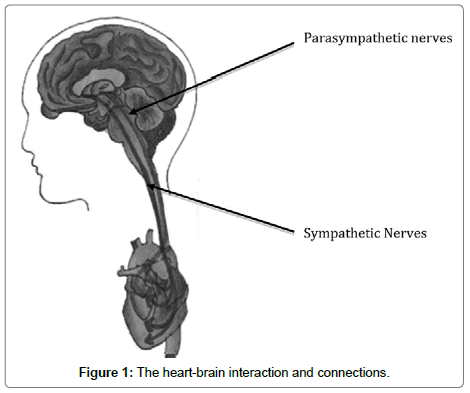
The anatomical connections in patients or clients can be illustrated as follows: connection between the cardiac nervous system (heart-brain) and the central nervous system (head-brain) (Figure 1). The local circuit neurons in the heart are involved in coding of longterm memory in the hippocampus. The heart’s functional memory via these heart neurons ensures that intuitive or heartfelt feelings are processed in the heart-brain. They also link directly with the gut-brain and head-brain networks. This builds on the widespread cultural belief that feelings registered at a heart level are as powerful if not more powerful than those of the gut-brain and head-brain.
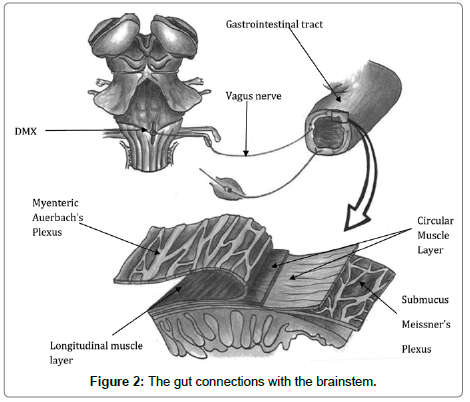
Connections between the brain in the gastrointestinal tract (gut-brain) and the brainstem (head-brain) are illustrated (Figure 2). This is highly significant in anxiety resolution: there are layers of protection for the intrinsic neurones of gut plexuses from the contents of the gut mucosa. When the neural plexi afferents from and efferents to the head, gut, and heart are all connected, then maximal flow of information occurs. This appears to be possible using BART psychotherapy. The head-brain links up with the other systems via the sympathetic and parasympathetic nervous systems. The dorsal motor nucleus of the tenth cranial, or vagus, nerve has its origin in the brainstem and synapses in the muscle wall of the gastrointestinal tract (GIT). In Figure 2, the black arrow shows a magnified section of the GIT containing the intrinsic neurones of the gut plexus. There are longitudinal and circular muscle layers containing Meissner’s plexus in between them at the sub mucosa layer, which has only parasympathetic fibres. Auerbach’s plexus also lies between the circular and longitudinal layers at the muscular are propria layer and has both sympathetic and parasympathetic input from the central nervous system.
The enteric nervous system (ENS), or gut-brain, has thirty different neurotransmitters and 90 per cent of the body’s serotonin, as well as 50 per cent of its dopamine receptors. It also has taste receptors which sense sweetness on the tongue and levels of glucose in the blood-stream. These taste receptors regulate insulin and are a good example of how the ENS really acts as our gut-brain and is capable of independent action. The processing of the gut instinct, or gut reaction, to incidents is a prerequisite for the BART therapeutic approach and is fully explained in the recently published Beyond Art of BART, [7].
Research by Cryan and Dinan [8] reveals how the gut micro-biota communicates with the CNS through neural, endocrine, and immune pathways. This provides scientific evidence for an influencing role in the regulation of anxiety, mood, cognition, and pain. The microbiotas are integrated into the illustrated gut-brain axia and impact on the brain in states from satiety to stress.
A range of mechanisms have been proposed by which gut flora affect the CNS:
Altering composition of the gut flora: They can compete for dietary ingredients such as growth substrates; they can produce vitamins, reduce inflammation, and stimulate innate immune responses. All these can change gut–brain signalling.
Immune activation: The immune system interacts bidirectionally with the CNS. Also, indirectly, the gut flora affects the immune system, altering cytokine levels. These are both pro- and anti-inflammatory and directly impact brain function.
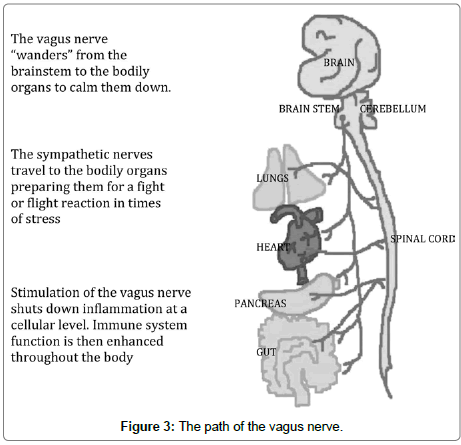
Vagus nerve: As illustrated above in Figure 3, this regulates bronchial constriction, heart rate, and gut motility. About eighty per cent of nerve fibres are sensory, conveying sensory information about the body organs to the CNS. Many of the effects of gut flora are dependent on vagal activity. The mechanisms of vagal afferent activation by gut microbiotica have yet to be elucidated.
Metabolism of tryptophan: This essential amino acid is a precursor of serotonin. This metabolic pathway becomes dysregulated in many brain and gastrointestinal tract disorders. Two key enzymes involved in the metabolism are activated by inflammatory mediators and corticosteroids.
Microbial metabolites: Gut flora are essential in the production of bile acids, choline, and short chain fatty acids. Complex carbohydrates are digested and fermented in the colon by gut microorganisms into neuroactive short chain fatty acids.
Microbial neurometabolites: These neurotransmitters act on the enteric nervous system and may have anti-nociceptive properties.
Bacterial cell wall sugars: These may modulate neural signalling or act on afferent axons.
Anne Robinson [9] Mon 1 August 2016 Guardian reports that overuse of antibiotic and obsession with cleanliness is damaging microbial gut diversity worsening such conditions as depression, multiple sclerosis obesity and rheumatoid arthritis. Most microbes are beneficial and the gut-brain weighs in at 1-2kg, which is the same as the head-brain. Babies are first exposed to maternal gut bacteria as they travel down the birth canal. Those born by caesarean section appear to be more prone to illnesses.
Sarkar et al [10] of University College Cork states that good brain health depends on good gut health. The gut microbiome affects every aspect of brain functioning and human behaviour. It appears that people with high level of bifidobacteria in the gut withstand psychological stress better than those with low levels. It is also true that diversity of the microbiome is associated with physical strength and cognitive flexibility. Work still needs to be done to find out how gut bacteria send signals to the brain. However, I believe the techniques outlined in the head, heart and guts of BART psychotherapy provide a pathway for this signalling. Professor Cryan believes that in the next five years we will learn a lot more about which specific bacteria are important. It will then be possible to test our personal microbiota and supplement any deficiencies. Over a similar time frame I am optimistic that BART psychotherapy will develop hand in hand with these specific blood tests.
The elusive anatomical structure of the gut mesentery has recently been fully described by Prof Calvin Coffey [11]. It is associated with the small intestine and colon and unlike the early depictions by Leonardo da Vinci and Toldt [12] in 1879 it has now been shown as contiguous. Discoveries in the future in relation to the mesentery can now be unified from different disciplines under the heading mesenteric science. Its full role in colorectal cancer, inflammatory bowel disease, diverticular disease, cardiovascular disease, diabetes, obesity and metabolic syndrome has yet to be clarified. The mesentery originates from where the superior mesenteric artery is attached to the aorta. This “root region” may correspond to the root chakra outlined in the The Art of BART [6]. The mesentery and intestine appear to be continuous from the diaphragm to the pelvic floor. This provides support for the effectiveness of gut reprocessing during sessions of BART psychotherapy. While the intestine is endodermal in origin, the mesentery comes from the mesodermal germ layer. The layers of the intestine and mesentery communicate via the connective tissue layer or serosa. Thus when I encourage patients to imagine difficult or distressing emotions sensed in the abdomen as a knot in the stomach, I will state, “Imagine bringing these feelings up to the surface of the abdomen where they will start to change and become less intense.” Now there exists an anatomical pathway from the stomach to the mesentery to the peritoneum that in theory conveys these subjective emotions. I believe this is evidence for the emotional and sensory model of the gut-brain proposed in BART.
It is at the intersection of the intestine and mesentery that blood vessels arteries veins and capillaries exist from the duodenum down to the rectum. The mesentery has a role in detecting intestinal bacteria and regulating movement of T and B, natural killer, and dendritic cells to intestinal mucosa [13]. The neuroanatomy of the mesenteric peripheral nervous system is little understood. The lymphatic, neurological, vascular, connective tissue connections in the mesentery emphasise its central importance as a human organ. It may be part of the endocrine and immunological and metabolic systems also. Further study will elucidate its structure and function. It is my hypothesis that BART psychotherapy is the only therapeutic approach that fully integrates physical and mental health. This is achieved by activation of the gut-brain (micro biome and mesentery), heart-brain via the cardiac nervous system and head-brain at the level of the cerebellum, brainstem and cerebral cortex.
Knowledge of all these mechanisms of interaction of the gutbrain’s enteric nervous system on the central nervous system lends credence to my hypothesis that reprocessing of the guts emotional response can help to reduce any dysregulation of the gastrointestinal system. Also, continuing reprocessing of distressing sensations in relation to trauma at the level of the stomach can be signalled to the heart and brain via the vagus nerve. This will enable digestion and metabolism of these sensations at a cognitive level.
The vagus or tenth, cranial nerve leaves the brainstem and tends to calm down all the organs of the body. The sympathetic nerves have the opposite effect. This is because Figure 3 is in black and white. and get the person ready to engage the “fight” response or mobilise the heart, lungs, and muscles for “flight” (Figure 3).
The five organs illustrated may represent the five stages of BART psychotherapy and peak performance. Thus:
1. Activation of the gut instinct or gut reaction at level of the gut mesentery as explained earlier.
2. Stimulation of the pancreas with release of insulin and proposed direct link to anterior inferior and posterior inferior sections of insular cortex in cerebrum.
3. Energising of heart and lungs organ with reprocessing of anxiety, loss and grief.
4. Figure 3 shows the path of the vagus nerve. Activation gives rise to inspiration and expiration of the lungs, and helps to stabilise any functional impairment due to anxiety, rapid breathing or panic attacks.
5. Continuous bilateral stimulation of head-brain at the level of the cerebellum so that the patient or client can take on board all of the information reprocessed at lower bodily energy or organ levels.
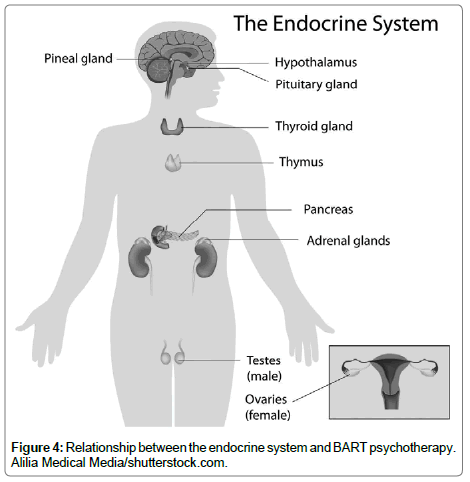
The techniques of BART psychotherapy are designed to boost the immune and endocrine systems and allow for neuronal rewiring (Figure 4). Both cerebral hemispheres and the gastrointestinal tract develop from the neural crest at ten weeks gestation. Thus, they have the potential to communicate interneuronally. It takes both the gut mucosa and the brain four years to develop protective myelin sheaths. Thus, children younger than four are especially prone to infections, food allergies and intolerance, and the developing brain is susceptible to abuse and neglect. The heartbeat develops at eight weeks gestation and sets the basic rhythm experienced throughout life. The heart has its own independent neural network. BART psychotherapy enhances the gut, heart, and brain neuronal and energetic communication. At the head-brain level, BART psychotherapy promotes interhemispheric integration. The patient or client is mindful of feelings and reprocessed thoughts.
The intrinsic nervous system of the heart triggers a heartbeat from the eighth week of gestation. The 40,000 functional group of autonomous nerve cells in the heart can register heartfelt emotions and sensations linked to loss and traumatic grief. The heart has evolved from a single tube in fish, two chambers in frogs, three chambers in reptiles, to the four-chamber human heart. With each evolutionary stage has come greater neuronal sophistication.
The pancreas and intestines are part of the gut-brain. They give rise to the patient or client’s gut instinct or reaction. The pancreas produces insulin, which may be directly detected by the insular cortex of the head-brain. The gut’s enteric plexus contains one hundred million nerve cells. These can function independently to the central and cardiac nervous systems. This is particularly true in children. Most parents will recognise the scenario: John or Mary does not want to go to school. It is Monday morning and they are complaining of a pain in their tummy. Concerned, you pay a visit to the doctor. The examination proves inconclusive and the diagnosis of acute nonspecific abdominal pain, or ANSAP, is made. I would interpret the pain in emotional terms and, as a child has not yet fully developed the capacity for abstract thought, they are unable to put into words the reasons for their emotional distress. Using the techniques described in this article, psychotherapists will discover how to link the sensations of the gut-brain to the thought processes in the head-brain.
The adrenal glands and kidneys are positioned bilaterally and can give rise to a patient or client who says, “I feel it in my water”. The circulating adrenaline transmits these feelings of fight, flight, fright, freeze, falling, and feigned death around the endocrine system. BART psychotherapy promotes the reprocessing and resolution of sensations, feelings, emotions, and thoughts at each brain level.
The activation of the root, or base, chakra energies may be related to processing of testosterone from the testes in the male and oestrogen from the ovaries in the female. This is especially relevant in patients who are victims of sexual abuse, which remains unresolved (Figure 4).
Composition of neuroreceptors in the heart-brain, or cardiac neural plexus.
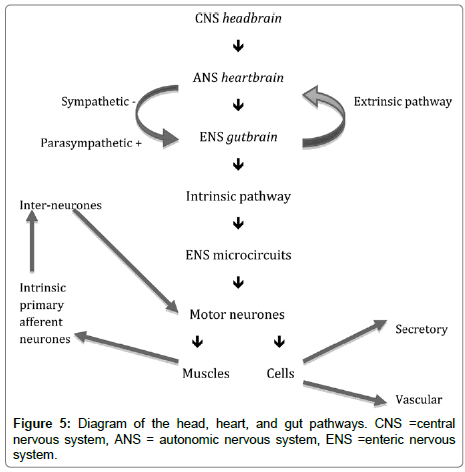
Twenty per cent of heart neurons are receptive, that is, detect mechanical pressure in the heart. Chemoreceptor neurons account for the remaining eighty per cent. These are sensitive to hormones and neuro-transmitters. This information accumulates in the heartbrain for decision making at a local level. It connects to brain, gut, skin, lungs, and other visceral organs, subsequently. The patient benefits by paying attention to this bodily information. The heartbrain synchronises with the patient’s head-brain and thalamus. Fluent heart rate variability (HRV) results. Mindful breathing helps induce a harmonious mental state in the patient, and regulates HRV, helping to calm the patient or client’s dysregulated, emotional state. Quantum coherence may lead to the occurrence of synchronised electrical activity emanating from the heart to the thalamus to the frontal cortex. This allows for better focusing and reprocessing of patient or client reactions, which are appropriate to the situation and within their window of tolerance (Figure 5).
Role of the gastrointestinal tract in processing food and emotional reactions and hypothetical link to insular cortex in cerebral hemispheres, or head-brain.
The gut absorbs and processes food, which increases glucose concentrations in the bloodstream. The pancreas produces insulin (from the islets of Langerhans). The insular cortex in the brain may directly perceive this hormone. It is divided into the anterior insular cortex (AIC) and posterior insular cortex (PIC) and helps to give us insight into our basic gustatory feelings. Indeed, its phylogenetic origin is from the gustatory cortex, which, in mammals, enables the processing of taste and leads to the perception of disgust.
A recent review by Kennedy et al. [14] examined the neural pathways connecting the brain to the gut and vice versa. Thus, the gut viscera influences brain functioning. Stress, mood, thoughts, and emotion affect gut function via the vagal pathways of the autonomic nervous system. The immune system affects functioning of the enteric nervous system, which then influences the central nervous system. Other mediators include neurotransmitters and neuropeptides such as serotonin, noradrenaline, and corticotrophin-releasing factor. This led to the hypothesis of cognitive dysfunction and stress as important in the aetiology of gut disorders such as irritable bowel syndrome.
Both AIC and PIC components of the insular cortex have a role to play in the integration of social emotions, from empathy, disgust, and pain to experiences of joy, compassion, admiration, and fairness. The left and right AIC may code for positive and negative affect in the prefrontal cortex (PFC), as suggested by Davidson [15]. This provides further scientific evidence for the benefit of continuous bilateral cerebellar stimulation in the twin approaches of BART psychotherapy for resolving trauma and achieving peak performance.
The insular cortex has visceral and sensory neural connections. It encodes body temperature, sensations from the musculature, viscera, and levels of arousal. This leads to a gradual process of interoceptive awareness, which is consistent with the five stages of BART psychotherapy. Initial gut instinct such as visceral or somatic bodily feelings is at the genesis of human emotional experience. Integration and appraisal of this information allows the patient or client to progress to interpretation and action based on their instinctive or conscious experience. Thus, a sensation such as “stomach tension” could be associated with feelings of fear or pleasure. The individual patient or client is helped by the BART psychotherapist to correctly identify the emotional memory linked to the stomach sensation.
The insular cortex plays a critical role in mapping internal bodily somatic and feeling states. Once mapped, they can form the basis for predictions of further bodily reactions to emotional or sensory stimuli directly related to the self.
It appears that painful stimuli map on to the PIC while affective stimuli related to the self-map on to the AIC. It is my hypothesis that this part of the cortex was named after the pancreas, which produces insulin. It is as if this hormone, which monitors glucose levels in the gut, has a direct neural link to the insular cortex to provide the same role for cortically expressed emotions. Thus, there is an integration of feeling, empathy, and uncertainty in the insular cortex. This is appraised by the cerebral hemispheres, as explained in The Art of BART [6].
The insular cortex has emerged as the key structure in the brain to be activated for trauma resolution, according to one of the world’s foremost experts on emotion and behaviour, Professor Ray Dolan, of Queen’s Square Hospital for Neurology and Neurosurgery in London. It is involved in processing internal bodily signals (interoception). In addition, it integrates the patient or client’s mental map with incoming sensory information to create a definitive sense of self [16,17]. He was one of a triumvirate of neuroscientists awarded the Brain Prize on 6 March 2017 [18] for research into the pathways of motivation and reward in the brain.
This is the putative site for registration of gut feelings in the brain. Coherence allows information from the head-brain, heart-brain and gut-brain to be synchronised and balanced.
The autonomic nervous system (ANS), endocrine and immune systems are similarly coordinated. Eventually, the aim is for them all to fire at the same rate. Those that fire together wire together (i.e., work well interactively). Synergistic adaptive growth ensures that, with healthy evolution, HRV varies when an emotional stimulus is about to be shown. Thus, four or five seconds before it is actually shown, the prefrontal cortex (PFC) registers this intuitively. The PFC then modulates heart rhythm 250 ms later. We become attuned (from sound or stretch) to the heart’s rhythm.
Unconsciously stored information is intuitive until it is reprocessed from the body-mind into our consciousness. BART psychotherapy accelerates that process in the fourth stage of activating our brain’s axons, which are rewired for transmission (cf. stage four of BART psychotherapy).
Figure 5 shows how the gut has sensory and motor control independent of the peripheral and central nervous systems. The intrinsic and extrinsic pathways are shown.
Doc Childre [19] founded the Institute of Heart math in 1991 and sought to explore the effect of stress on human body systems. The heart is the most powerful generator of electromagnetic energy in the human body. As such, it is uniquely positioned to connect the gut-brain, head-brain, emotions, feelings, sensations, and spiritual aware-ness. To quote Childre and Rozman [20], since emotional processes can work faster than the mind, it takes a power stronger than the mind to bend perception, override emotional circuitry and provide us with intuitive feeling instead. It takes the power of the heart.
The heart’s magnetic field: The magnetic field emanating from the heart is 5,000 times larger than that from the brain and measurable up to several metres from the body [21] (McCraty, Atkinson, & Tomasino, 2001). Augmentation of this magnetic field is a goal of future BART psychotherapy. The heart’s electrical field is sixty times greater in amplitude than the electrical activity generated by the brain. The heart communicates with the brain and body in four ways via:
• nervous system or neurologically;
• pulse waves of blood pressure or biomechanically;
• hormones or biochemically;
• electromagnetic fields or energetically
This diagram illustrates how the heart-brain is a focal point for communication with both the enteric nervous system or gut-brain and also the cerebral cortex or head-brain. It is a key concept in BART that the heartfelt sensations are a bridge to feelings and emotions and cognitive insights processed at the level of the insular cortex in the head-brain. It is also likely that reprocessing of the negative feelings and cognitions associated with traumatic experiences can lead to post traumatic growth with the development of compassion for example. Patients are encouraged to imagine via guided visualization that now their traumatic stressful experiences have entered resolution a window of opportunity exists to achieve optimal or peak performance in their chosen goals and future templates.
Case Example
My patient who suffered chronic physical and psychological abuse by her father.
I met with a female patient age 17 with her mum. From an early age dad was psychologically and physically abusive. She remembered being humiliated from the age of 6. On another occasion she tried to run away. He caught her, pinned her against a wall and punched her. When she didn’t want to attend a school event she ran up to her room to escape. Her dad grabbed her by the ankles from the top of the stairs and proceeded to drag her downstairs. She was terrified and feared for her life. This abuse went on until she was 14 and only ended when she witnessed her dad attempt to strangle her mother. After that event my patient, her mum and her 2 younger sisters left the house in the middle of the night to stay with relatives. My patient has had limited contact with her dad since.
Course in therapy
My patient asked if her mum could sit in on the first session. I asked both to complete the Impact of Events scale, Appendix 1. I have modified this so that it can be used to amalgamate the impact of a series of events across the lifespan. My patient was asked to reflect on the impact of all the abuse she had experience from her dad from ages 6-14. Her scores were:
A. Intrusive thoughts (Table 1)
| Question No. on Revised Impact of Events Scale | Question on Revised Impact of Events Scale | Initial score |
|---|---|---|
| 1 | Any reminders brought back feelings about them | 3 |
| 2 | I had trouble staying asleep | 3 |
| 3 | Other things kept making me think about | 3 |
| 6 | I thought about them when I didn’t mean to | 0 |
| 9 | Pictures about them popped into my mind | 3 |
| 16 | I had waves of strong feeling about them | 2 |
| 20 | I had dreams or nightmares about them | 3 |
| Subtotal | 17 | |
Table 1: Intrusive thoughts.
B. Avoidance Behaviour (Table 2)
| Question No. on Revised Impact of Events Scale | Question on Revised Impact of Events Scale | Initial score |
|---|---|---|
| 5 | I avoided letting myself get upset when I thought about them or was reminded of them | 3 |
| 8 | I stayed away from reminders of them | 2 |
| 11 | I tried not to think of them | 3 |
| 12 | I was aware that I still had a lot of feelings about these events but I did not deal with them | 2 |
| 13 | My feelings about them were kind of numb | 1 |
| 22 | I tried not to talk about them | 4 |
| Subtotal | 15 | |
Table 2: Avoidance Behaviour.
C. Symptoms of Hyperarousal (Tables 3 and 4)
| Question No. on Revised Impact of Events Scale | Question on Revised Impact of Events Scale | Initial Score |
|---|---|---|
| 4 | I felt irritable and angry | 2 |
| 10 | I was jumpy and easily startled | 3 |
| 14 | I found myself acting or feeling like I was back at that time | 3 |
| 15 | I had trouble falling asleep | 3 |
| 18 | I had trouble concentrating | 3 |
| 19 | Reminders of them caused me to have physical reactions, such as sweating, nausea (sickly feeling), a pounding heart or trouble breathing | 4 |
| 21 | I felt watchful or on guard | 3 |
| Subtotal | 21 | |
Table 3: Symptoms of Hyperarousal.
| Total Score (/88) | Diagnosis |
|---|---|
| 53 | Moderate PTSD |
Table 4: Diagnosis.
I believe analysis of these scores can point towards the risks inherent in this case. My patient had dealt with these symptoms by avoidance. However now she was in direct contact with her dad over the last few years her symptoms had been rekindled. Also the 2 items where she scored maximum indicating extreme distress were an inability to talk about these adverse events [22] and extreme physical reactions [19]. It is this speechless terror that is a hallmark of PTSD and one of the indicators of a positive response to the BART therapeutic model.
Session 1: We agreed that we would work on the memory of when my patient was 6. She felt humiliated by her memories of how her father treated her. I noticed that she went red in her face and neck as these feelings including embarrassment came to the surface.
As mum observed the session my patient described how her dad would persistently criticize her in front of others and during mealtimes. The feelings of anxiety moved to her abdomen, throat and chest. She tracked these with the buzzers held in each hand. The SUDS level started at 7/10. As the processing continued the sensations associated with the distressing emotions changed. The SUDS reduced to 6 then 5/10.
I showed the diagram of the brain divisions and asked my patient to identify the strongest unresolved emotion. As she felt anger she connected to a previous memory stored unconsciously.
Age 15 her first ‘proper boyfriend’ had been staying at her house. She wanted to break up with him. He persuaded her to maintain the relationship. They were arguing. My patient saw her sister break her phone charger. She became enraged and jumped on her younger sister. My patient was later told that she was pulled away from her sister. She had no memory of the experience and was clearly in a dissociative state at the time. The intense feelings of anger associated with this experience were felt in the body and reprocessed into anxiety, embarrassment and confusion. The buzzers were placed in turn on her chest, throat and on either side of her head. The confused feelings moved from the front of her head or PFC to the back of her head or occipital cortex. She felt the anger disappear.
As we reconnected to the memories of how she was treated when age 6 she was able to re-experience the sensations, emotions and feelings of panic, anxiety and embarrassment. These were integrated at the level of the body mind.
I explained the metaphor of how these experiences at 6 had become derailed and off the tracks. Via continuous bilateral stimulation the memories and associated feelings, emotions and sensations had been lifted back on track. The normal flow of information could track along the neural networks of the peripheral and central nervous systems. They would end up stored in the long-term memory of the filing cabinet known as the hippocampus and cerebral cortex.
As I asked my patient to revisit these memories from age 6 she rated SUDS as 1/10 and finally 0/10. Mum was delighted with her progress and my patient and I agreed to process the memories with the highest emotional charge or distressed affect at our final 2 sessions.
Session 2: My patient arrived on her own to the session. We agreed to start with the memory where she had told her parents that she didn’t want to go to the school award ceremony. Her dad became aggressive and chased her up the driveway when she refused to get into the car. She attempted to escape by running up the stairs. She previously said he had grabbed her by the ankle but now she remembered he had dragged her down the stairs by the wrist. She felt scared and confused. She experienced this affect in the gut and right forehead as she tried to make sense of what had happened. In the end she managed to escape by running upstairs and going to her bedroom. She couldn’t understand why he had behaved this way over a minor incident. As she reprocessed these feelings she felt anxiety at a heart or chest level. She realized that over the years thinking of her dad induced sweating, panic and an overwhelming sense of anxiety. She would become angry and challenge him.
I introduced the idea of a somatic interweave. She stretched out her hands as if pushing him away and realized that this was one of her coping strategies. The SUDS level started at 9/10. Now she was able to let a lot of the anger go and the SUDS dropped to 1/10 before becoming 0/10. It was now as if the memory had been stored in the filing cabinet in the back of my patient’s mind. It was no longer a disturbing presence in the front of her mind.
The second memory was when my patient was 9 and her dad again exploded with unpredictable anger. He had slapped his younger daughter on the arm and then dragged my patient down stairs by her ankles. He then pinned her up against the wall and started hitting her. My patient described ‘steeling’ herself to cope with the beating. She had her face pushed against the wall as he punched her repeatedly on the back. At times she ‘blanked’ out. This is a protective form of reduced awareness known as passive freeze. Her mum shouted at him to stop. Eventually he let go and she ran upstairs where she locked herself in her bedroom. The SUDS level for this memory was 10/10. As she remembered being in her bedroom she felt safe and a sense of calm as the assault was at least over for another day.
I asked my patient to connect to that memory of her as a 9-yearold girl. I asked her to visualize saying to that image of herself as a 9 year old what she needed to hear to feel secure and safe. This technique is from ego state therapy as taught by Fran Waters [22] LCSW in the US. My patient was able to reprocess multiple thoughts, feelings and sensations associated with this episode. In particular she now realized that it wasn’t her fault. She was the victim of physical and psychological abuse from her father, which should have been reported to the police. My patient reported that previously thinking of her dad made her feel angry upset and unable to speak about the traumatic events. Now that she had worked through her feelings she felt immensely relieved and the SUDS level was now 0/10.
The third traumatic memory SUDS 10/10 to the third traumatic memory with a SUDS score of 10/10. My patient witnessed him assault her mother who was pushed up against a doorframe. She was almost strangled and thought she was going to die. His hands were around mum’s throat and his facial expression was enraged and his eyes were described as almost black.
Dad was told to leave and my patient was woken at 3 a.m by mum who said they were to leave immediately to stay with relatives in the midlands. Family of my patient her 2 younger siblings to the family of my patient, her 2 younger siblings. They stayed there for 1 week before returning to their previous neighbourhood initially in a holiday let. This proved too expensive and they were forced to return home where the locks were changed.
In defending herself from his vicious assault mum had kicked out automatically in self-defence. This had bruised her husband’s leg and he threatened to inform police and social services that in fact he had been assaulted and her allegations were made up. These events were overwhelming for my patient and she took an overdose.
Comments on reprocessing by patient during the session: Using a modified version of Elan Shapiro’s Recent Traumatic Event Protocol [23]. I invited my patient to get in touch with the most distressing feelings, thoughts, memories, emotions, sensations or movement impulses from the moment of the flight to the midlands culminating with her impulsive overdose which was an attempt to deal with the intolerability of being outside her window of tolerance.
My patient was able to get in touch with a range of feelings especially anger which was felt to be active at a gut-brain level. I encouraged her to tap on her abdomen bilaterally with each hand. She was also able to relax her arms and let go of all her anger. She reflected, “I am a bigger and better person for being able to do this. Final She felt a weight lifted from her shoulders. She moved the zappers or buzzers to each shoulder. I hypothesized that as she activated the neural networks at a shoulder level this would connect via the brainstem to her right and then left hemisphere. This would allow her to reflect and learn from this experience. In particular we discussed coping strategies as a future template was he to attempt to annoy, humiliate or frustrate her in the future. This is due to be tested experimentally using fMRI once appropriate research funding has been approved.
The holy grail of trauma therapy is to examine several interrelated brain networks before and after therapy. These networks become stuck at a developmental level of 7-9 years in adults or adolescents who have suffered childhood abuse. The default mode, salience and central executive networks are all adversely affected. My hypothesis is that following 12 hours of trauma-focused therapy using BART psychotherapy these networks will display a greater level of developmental integrity.
My patient related how she had pushed her dad away by not seeing him for several years after this assault. Her 2 younger sisters went to live with him. It appeared they couldn’t recall the abusive incidents and may have coped by dissociating at the time. According to my patient he bought their affections via bribery while she lived with her mother and didn’t receive any of the gifts given to her sisters.
It was suggested that my patient join her sister at a movie. My patient brought her boyfriend along for protection from any verbal attacks by her dad. To get some income she took up an admin post in the shop where her dad worked. She would occasionally get a lift from him. As a police car went by he joked,” If you and your mother were here you would probably call for the police to come and take me away in their car”.
My patient realized this was just the sort of comment designed to get her angry and annoyed. We reprocessed this memory so she felt insulated from these comments. I showed her how to stretch out her interlocked hands in front of her and move them up and down. This could act as a convex reflective shield deflecting his words back onto himself. This would give my patient extra protection in these situations.
My patient came to realize that not reacting to any insulting comments would disorient and confuse him. She would be victorious, as he would not know how to react. I used the magic remote to imagine scenarios in a future template to increase her confidence to put this strategy into practice.
Towards the end of the session my patient stifled a yawn. I explained that in my clinical experience this is a sign of engagement in BART psychotherapy and an indication of reprocessing at the level of the corpus callosum. The continuous bilateral auditory clicking at the level of the mastoid process just behind the ears helps to keep the prefrontal cortex tuned into bodily sensations, feelings and emotions.
It is my hypothesis that this continuous bilateral stimulation dampens brainstem activity. It is likely that pontine geniculate occipital [24] or (PGO) brainwaves are generated. This sets up transfer of information from the right to left cerebral hemispheres via the fibres of the corpus callosum. The PGO waves induce tiredness as witnessed by patient’s yawning. Further reprocessing generates the movements characteristic of Rapid Eye Movement Sleep. My patient ended the 120min session pleasantly tired and relaxed.
Final session: This appointment was the next day. My patient reported being able to discuss the details of the previous session without getting distressed upset or angry as they drove home. In this session my patient was able to recall an incident with a SUDS score of 10. This was not in her conscious awareness on initial assessment. It is common that unconscious memories emerge for reprocessing once a therapeutic relationship has developed. She described sitting in the college library when she suddenly developed an acute level of anxiety. She had to walk out of the building and sat on a wall until collected by her dad, as mum was unavailable at the time. Previously when my patient got a panic attack in secondary school, she was allowed out of the class until the symptoms subsided when she would return to the classroom. This time sitting on a wall outside college, she reluctantly rang dad. He collected her and brought her back to his place of work until my patient’s mum was able to collect her. He sarcastically said to my patient, “Now you know how I feel”, in an effort to shift attention to him. My patient remembers trying not to react to this provocation at the time. Using the magic remote I asked her to replay the scene in the car in her mind and allow any distress to surface. She became aware of a knot and tightness in her stomach, which was released by zapping the gut or enteric plexus by placing the handheld buzzers adjacent to this area.
This is the site where our earliest memories and physical sensations are located. My hypothesis is that these feelings are transmitted along the umbilical cord from conception and throughout pregnancy. Any prenatal or postnatal distress can be transmitted in uteri or directly to the infant. Thus the baby may become predisposed to chronic stress and anxiety
My patient was invited to rewind in time to the point of onset of the anxiety attack and explore any significant life events that might be related. She realized that she had been going out with her boyfriend around that time. He had broken his arm and she missed many classes to accompany him to hospital appointments. When she had sought support from him he was not emotionally available. She wanted to end the relationship but he begged her not too. A short time later he broke off the relationship. She felt betrayed and confused. These feelings were zapped at a chest level, using the buzzers until they were resolved and moved to the level of the left and right prefrontal cortices. I mentioned how the fog of confusion would lift and be reprocessed to the back of her mind. We now revisited the episode of panic in the library. My patient reported that she experienced the anxiety at a SUDS level of 0/10. We now tapped into all previous feelings of anxiety from the abusive memories associated with dad until they also reached a SUDS level of zero.
I now wanted to explore if there were any unresolved traumatic issues. My patient remembered having to look after her younger sisters when her mum was hospitalized with depression. Her stepdad Joe had occupied the role left by her dad who she accepted would come to play a small role in her life. The main unresolved issue was a feeling of resentment that no one protected her from the physical assaults and emotional abuse she experienced from her dad. This contrasted with the immediate action taken by mum to leave in the middle of the night when she was assaulted. We explored possible reasons for his behaviour. My patient described an incident when he was playing with setting fires. He ignited a gas canister and his friend’s clothes caught fire. The friend was rushed to hospital with severe burns. He required extensive surgery and skin grafts and her dad never spoke to his friend after the incident. As well her dad had a history of mental health problems.
Discussion
My patient gave feedback that before these sessions she would become emotionally overwhelmed and react without thinking. She would become anxious or develop panic attacks. She now reported that she could work through these instinctive or gut reactions. She was also able to recognize that they had been reprocessed at the level of the cardiac nervous system i.e. sympathetic and parasympathetic.
We discussed the default mode network (DMN). I explained that its development was likely to have stalled at age 7-9. This has been discussed in detail by Phillips [25] and Lanius [26]. Now that we had potentially freed up the DMN to continue its development, she would be able to access reason and rationalize her thoughts rather than revert to feelings of panic and anxiety.
Essentially her implicit unconscious memories are now part of explicit conscious awareness. My patient is aware of the previously unconscious drives to her behaviour and can choose to react in a manner integrating sensations feelings, emotions, movement, impulses and thoughts.
A. Intrusive thoughts (Table 5)
| Question No. on Revised Impact of Events Scale | Question on Revised Impact of Events Scale | Initial Score | Post-treatment score |
|---|---|---|---|
| 1 | Any reminders brought back feelings about them | 3 | 1 |
| 2 | I had trouble staying asleep | 3 | 0 |
| 3 | Other things kept making me think about | 3 | 1 |
| 6 | I thought about them when I didn’t mean to | 0 | 2 |
| 9 | Pictures about them popped into my mind | 3 | 2 |
| 16 | I had waves of strong feeling about them | 2 | 1 |
| 20 | I had dreams or nightmares about them | 3 | 0 |
| Subtotal | 17 | 7 | |
Table 5: Intrusive thoughts
B. Avoidance Behaviour (Table 6)
| Question No. on Revised Impact of Events Scale | Question on Revised Impact of Events Scale | Initial score | Post-treatment score |
|---|---|---|---|
| 5 | I avoided letting myself get upset when I thought about them or was reminded of them | 3 | 1 |
| 8 | I stayed away from reminders of them | 2 | 3 |
| 11 | I tried not to think of them | 3 | 3 |
| 12 | I was aware that I still had a lot of feelings about these events but I did not deal with them | 2 | 0 |
| 13 | My feelings about them were kind of numb | 1 | 1 |
| 22 | I tried not to talk about them | 4 | 2 |
| Subtotal | 15 | 10 | |
Table 6: Avoidance Behaviour.
C. Symptoms of Hyperarousal (Tables 7 and 8)
| Question No. on Revised Impact of Events Scale | Question on Revised Impact of Events Scale | Initial score | Post-treatment score |
|---|---|---|---|
| 4 | I felt irritable and angry | 2 | 0 |
| 10 | I was jumpy and easily startled | 3 | 1 |
| 14 | I found myself acting or feeling like I was back at that time | 3 | 1 |
| 15 | I had trouble falling asleep | 3 | 0 |
| 18 | I had trouble concentrating | 3 | 0 |
| 19 | Reminders of them caused me to have physical reactions, such as sweating, nausea (sickly feeling), a pounding heart or trouble breathing | 4 | 2 |
| 21 | I felt watchful or on guard | 3 | 0 |
| Subtotal | 21 | 4 | |
Table 7: Symptoms of Hyperarousal.
| Total Score (53/88) | Before treatment | After treatment (21/88) |
|---|---|---|
| Diagnosis | Moderate PTSD | No symptoms of PTSD |
Table 8: Diagnosis.
In looking at the scores after 6 hours of BART psychotherapy the pathological scores are for questions numbered 8 and 11 (Table 6). This refers to a reflex, which is present when she walks up stairs and a desire not to think about her dad. These show that her recovery has been adaptive to her current situation and we agreed to end therapy. She was interested in revisiting her unwillingness to forgive her parents for not protecting her.
Thus my patient is a good example of a client who was able to stop taking antidepressants and her symptoms of traumatic stress disappeared. This was completed using a course of 6 hours BART psychotherapy delivered over a period of approximately 3 weeks.
Areas for further development into the theory and practice of BART psychotherapy:
1. As an integrative treatment for physical and mental health problems.
The meninges of the central nervous system or head-brain have been shown to contain endothelial cells from the lymphatic system [27]. These endothelial cells transport fluid and immune cells from the cerebrospinal fluid (CSF) to deep cervical nodes. This provides a connection to the lymph nodes, thymus, spleen and bone marrow of the lymphatic system. Maiken Nedergaard [28] named the glymphatic system as a waste clearance system for the CNS. It involves glia cells. Glia is derived from the Greek word for glue and exists in the gutbrain as enteric glial cells (EGC’s). They interact with circulatory, sensorimotor, peripheral nervous, central nervous, endocrine and immune systems. EGC’s regulate permeability of gut mucosa and the neural activity of Meissner’s and Auerbach’s plexi. Knowledge of these interactions has the potential to improve disease states such as inflammatory bowel disease, irritable bowel syndrome and other conditions with reduced gut motility and a reactive EGC phenotype.
2. As a means of activating immune system connections between gut, heart and head, BART may lessen inflammation associated with neuropsychiatric disorders such as depression.
Interferon gamma has been shown to have a role in regulating neuronal connectivity and social behaviour [29]. It appears to mediate an adaptive immune response and promotes prosocial behaviour. Gaba amino butyric acid (GABA) comes from inhibitory neurons and reacts with interferon gamma to recruit neural circuits that promote social behaviour. Confirmation of this link between meningeal immune system and social behaviour at a molecular level represents a paradigm shift in our understanding. BART psychotherapists have the potential to apply this knowledge in the many neurological and psychiatric disorders that show disturbance in social behaviour. This includes ASD, ADHD, OCD, dementia and psychotic disorders such as BAD and schizophrenia.
3. As a specific treatment for autism spectrum disorders.
Patients with autism show hyper connectivity between the PFC and insular cortex in the frontal lobe. The inhibitory neurotransmitter GABA activates inhibitory interneurons designed to prevent hyper excitability and connectivity in the PFC. It is possible that abnormal immune responses may be a significant aetiological factor in autism spectrum disorders. The activation of imagination via guided visualization during BART may not only stimulate mirror neuron activity but also improve immune-neural communication at the level of multiple body systems. The author has treated a number of patients with autism to good effect. This will be commented on in a future paper.
4. As a means of treating immature neurological networks. These include the default mode and salience networks, (DMN and SN).
During resting state fMRI scanning patients with PTSD showed increased connectivity associated with the SN. This is because the SN is associated with threat sensitivity, impaired attentional control and hyperarousal. As seen in the case example all these symptoms are found in PTSD. The DMN regions include posterior cingulate cortex, ventromedial prefrontal cortex and bilateral anterior insula. During resting state scanning of the DMN using fMRI, patients with PTSD showed reduced coupling within the DMN, greater coupling within the SN and increased coupling between DMN and SN [30]. The key goal for future research into BART psychotherapy in patients with PTSD will be to show that clinical improvement is correlated with a relative reduction of threat sensitive circuitry and normalization of the DMN and SN networks in fMRI scans pre and post treatment.
Conclusion
According to Prof Kevin Tracey [31] the diverse fields of neuroscience and immunology have a new aetiological paradigm. This means that specific neurological circuits change some steps in cellular and humoral immunity, which in turn transmits signals through newly defined molecular mechanisms such as GABA inhibitory interneurons. Recent discoveries by Prof Coffey [13] on the structure and function of the mesentery shed new light on the links between the gut-brain and all the other information processing systems in the body. This paper has shown links between the gut heart and brain at a neurological and endocrinological level of organization. Latest research showing newly discovered links between the lymphatic immune and meningeal system have been described. BART psychotherapy is ideally placed to take advantage of these important new medical discoveries.
Acknowledgements
I would like to thank Pat Scully from Rédacteurs Ltd for reviewing an early version of this manuscript, Cliodhna and Sorcha O’Malley for help with the diagrams and Sorcha O’Malley for producing the unattributed figures.
References
- NHS North West (2011) Improving outcomes and ensuring quality: Guide for commissioners and Providers of Perinatal and infant mental health services. Manchester.
- Buckler R L (2013) The cerebellum and cognitive function: 25 years of insight from anatomy and Neuroimaging. Neuron 80: 807-815.
- Schmahmann JD, Pandya DN (1991) Projections to the basis pontis from the superior temporal sulcus and superior temporal region in the rhesus monkey. J Comp Neurol 308: 224-248.
- Deleuze G, Guattari F, Massumi B, Gilles Deleuze, Felix Guattari (2004) A thousand plateaus: Capitalism and schizophrenia. London: Continuum International Publishing Group. United Kingdom
- Ananthaswamy A (2013) Like clockwork: The cogs and wheels that drive our thoughts. New Scientist 219: 32-35.
- O’Malley AG (2015) The art of BART: Bilateral Affective Reprocessing of thoughts as a dynamic model for psychotherapy. Oxford, United Kingdom: Karnac Books, London.
- O’Malley AG (2016) Beyond the Art of BART: Bilateral Affective Reprocessing of Thoughts as a Dynamic model for Psychotherapy across the Lifespan. Int J Psychol Behav Anal 118.
- Cryan JF, Dinan TG (2012) Mind-altering microorganisms: The impact of the gut microbiota on brain and behaviour. Nature Reviews Neuroscience 13: 701-712.
- Robinson A (2016) Health and Wellbeing Is your gut making you sick?
- Sarkar A, Lehto SM, Harty S, Dinan TG, Cryan JF, et al. (2016) Psychobiotics and the manipulation of Bacteria–Gut–Brain signals. Trends in Neurosciences 39: 763-781.
- Coffey JC, O’Leary DP (2016) The mesentery: Structure, function, and role in disease. Lancet Gastroenterol Hepatol 1: 238-247.
- Toldt C (1879) Vereinsangelegenheiten. Deutsche Entomologische Zeitschrift. 1879: 7-8.
- Coffey JC, Culligan K, Walsh LG, Sehgal R, Dunne C, et al. (2016) An appraisal of the computed axial tomographic appearance of the human mesentery based on mesenteric contiguity from the duodenojejunal flexure to the mesorectal level. European Radiology 26: 714-721.
- Kennedy PJ, Clarke G, Quigley EMM, Groeger JA, Dinan TG, et al. (2012) Gut memories: Towards a cognitive neurobiology of irritable bowel syndrome. Neurosci Biobehav Rev 36: 310-340.
- Davidson RJ (2004) Well-being and affective style: Neural substrates and biobehavioural correlates. Philos Trans R Soc Lond B Biol Sci 359: 1395-1411.
- Schachter S, Singer J (1962) Cognitive, social, and physiological determinants of emotional state. Psychol Rev 69: 379-399.
- Rusbridger A (2014) alanrusbridger.com/playitagain/interviews/interview-professor-ray-dolan-frs.
- The Brain Prize (2017)
- Childre D, Martin H, Beech D, Howard Martin, Donna Beech (1999) The Heart Math solution. Harper San Francisco, San Francisco, USA.
- Childre D, Rozman R (2002) Overcoming emotional chaos: eliminate anxiety, Lift depression and create security in your life.
- Mc Craty R, Atkinson M, Tomasino D. Science of the heart: Exploring the role of the heart in human performance.
- Waters F (2016) Healing the fractured child: Diagnosis and treatment of youth with dissociation. First ed. Springer publishing company: 1-73.
- Shapiro E, Laub B (2008) Early EMDR intervention (EEI): A summary, a theoretical model, and the recent traumatic episode protocol (R-TEP). J EMDR Prac Res 2: 79-96.
- Stickgold R (2001) EMDR: A putative neurobiological mechanism of action. J Clin Psychol 58: 61-75.
- Philip NS, Carpenter SL, Sweet LH (2014) Developing Neuroimaging Phenotypes of the default mode network in PTSD: Integrating the resting state, working memory, and structural Connectivity. J Vis Exp 89: 51651.
- Lanius RA, Bluhm RL, Coupland NJ, Hegadoren KM, Rowe B, et al. (2010) Default mode network connectivity as a predictor of post-traumatic stress disorder symptom severity in acutely traumatized subjects. Acta Psychiatr Scand 121: 33-40.
- Louveau A, Smirnov I, Keyes TJ, Eccles JD, Rouhani SJ, et al. (2015) Structural and functional features of central nervous system lymphatic vessels. Nature 523: 337-341.
- Jessen NA, Munk ASF, Lundgaard I, Nedergaard M (2015) The Glymphatic system: A beginner’s guide. Neurocheml Res 40: 2583-2599.
- Filiano AJ, Xu Y, Tustison NJ, Marsh RL, Baker W, et al. (2016) Unexpected role of interferon-γ in regulating neuronal connectivity and social behaviour. Nature 535: 425-429.
- Sripada RK, King AP, Welsh RC, Garfinkel SN, Wang X, et al. (2012) Neural Dysregulation in Posttraumatic stress disorder. Psychosom Med 74: 904-911.
- Tracey KJ (2002) The inflammatory reflex. Nature 420: 853-859
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi