Review Article, Jrgm Vol: 12 Issue: 6
Bone Marrow Aspirate and Injectable Platelet Rich Fibrin for Achilles tendon Rupture
Joao vitor Bizinotto Lana1*, Napoliane Santos2,3, Gregory Melo1, Gabriel Silva Santos2,3, Palmerindo Mendonca2,3, Luyddy Pires2,3, Francisco Honorio2,3, Lucas Furtado da Fonseca2,3,4, Raffael Marum Bachir3,5, Rafael Barnabe Domingues2,3,6, Jose Fabio Lana1,2,3,6
1Medical Specialties School Center, Max Planck University Center (UniMAX), Indaiatuba, SP, Brazil
2Department of Orthopedics, Brazilian Institute of Regenerative Medicine (BIRM), Indaiatuba, SP, Brazil
3Regenerative Medicine, Orthoregen International Course, Indaiatuba, SP, Brazil
4Department of Orthopedics Federal University of São Paulo (UNIFESP), São Paulo, SP, Brazil
5Hospital IFOR, São Bernardo do Campo, SP, Brazil
6Clinical Research, Instituto Anna Vitória Lana (IAVL)
*Corresponding Author: Joao vitor Bizinotto Lana
Medical Specialties School Center, Max Planck University Center (UniMAX), Indaiatuba, SP, Brazil
E-mail: jvblana@gmail.com
Received: 08-Nov-2023, Manuscript No. JRGM-23-119678;
Editor assigned: 10-Nov-2023, PreQC No. JRGM-23-119678 (PQ);
Reviewed: 24-Nov-2023, QC No. JRGM-23-119678;
Revised: 27- Nov-2023, Manuscript No. JRGM-23-119678 (R);
Published: 04-Dec- 2023, DOI:10.4172/2325-9620.1000275
Citation: Lana JVB, Santos GS, Santos N, Melo G, Mendonca P, et al. (2023) Bone Marrow Aspirate and Injectable Platelet Rich Fibrin for Achilles tendon Rupture. J Regen Med 12:6.
Copyright: © 2023 Lana JVB. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Achilles tendon rupture is a frequent ailment tied to overuse injuries of the ankle and foot. Given the tendon's limited vascularization, which depends on diffusion from synovial fluid for nutrient intake, managing this condition poses challenges. The weakened state post-rupture can predispose one to further injuries. Although surgical interventions often lead the way in treatment, challenges can arise during recovery. Meanwhile, the use of orthobiologics for non-invasive treatment has shown promising outcomes in various regenerative medicine applications. Notably, autologous treatments like bone marrow aspirate (BMA) and injectable platelet-rich fibrin (i-PRF) have gained traction in clinical scenarios.
BMA is a reservoir of diverse cell populations and molecules pivotal for tissue regeneration. PRF, on the other hand, is a dense concoction of platelets, growth factors, cytokines, leukocytes, and a sturdy fibrin matrix conducive to cellular functions.
Utilizing a combination of these two orthobiologic entities could amplify their individual effects, optimizing the healing process by fostering tissue growth, fostering new blood vessel formation, and modulating immune responses.
With this understanding, we advocate for the joint use of BMA and i-PRF as a potent orthobiologic solution, aiming to improve the healing trajectory of Achilles tendon ruptures within the sphere of regenerative orthopedics.
Keywords: Achilles tendon rupture; Bone marrow aspirate; Platelet-rich fibrin; Orthobiologics; Regenerative medicine.
Introduction
Achilles tendon rupture is a relatively common injury that occurs when the tendon, located at the back of the ankle, tears or ruptures. This injury can have a significant impact on mobility and athletic performance. Epidemiologically, Achilles tendon ruptures are most commonly seen in middle-aged individuals, particularly males, who participate in physical activities that involve repetitive jumping or sudden changes in direction. The prevalence of Achilles tendon ruptures is estimated to be around 18 to 37 cases per 100,000 people per year, with an increasing incidence noted in recent years [1,2].
The Achilles tendon is the thickest and strongest tendon in the human body. It originates in the calf region, specifically from the fusion of the gastrocnemius muscle and the soleus muscle. The gastrocnemius muscle has two heads, medial and lateral, which cross the knee joint. Deep to the gastrocnemius lies the soleus muscle. Together, these muscles form the triceps surae, and their conjoint tendon is known as the Achilles tendon [1,3]. The Achilles tendon has three main vascular areas: the peroneal artery supplies the midsection of the tendon, while the posterior tibial artery supplies the proximal and distal sections. The mid-substance of the tendon has relatively poor vascularization, which may contribute to a higher incidence of pathology in that region [1,3].
The length of the Achilles tendon averages about 15 cm, with variations ranging from 11 to 26 cm. Its width changes along its course: it measures around 6.8 cm (4.5–8.6 cm) at its origin and narrows to approximately 1.8 cm (range 1.2–2.6 cm) in the midsection. As it approaches the calcaneus (heel bone), the Achilles tendon becomes more rounded and has a width of about 3.4 cm (2.0–4.8 cm) at its insertion site on the posterior surface of the calcaneus. [1,3]. The Achilles tendon is connected to both the soleus and gastrocnemius muscles. The exact proportion of these insertions varies among individuals. Studies on cadavers have shown that in approximately 52% of cases, 52% of the tendon fibers originate from the soleus muscle, while 48% come from the gastrocnemius muscle. In 35% of cases, an equal contribution is observed, and in 13% of cadavers, more than 60% of the contribution arises from the gastrocnemius muscle [1,3].
The main motivation for the development of this study is based on the favorable results that researchers have obtained with the use of autologous products derived from bone marrow aspirate (BMA) and platelet concentrates such as platelet-rich fibrin (PRF) in accelerating the healing process and improving degenerative conditions. We believe that the association of the rich cellular and molecular components from BMA and PRF might establish an effective therapeutic methodology for the treatment of patients with Achilles tendon rupture.
Etiopathogenesis
Symptoms of an Achilles tendon rupture can vary, but one common and distinctive symptom reported by many individuals is a sudden and audible “popping” or “snapping” sound at the time of injury. This sound is often accompanied by a sharp pain in the back of the leg or ankle. The popping sensation occurs when the Achilles tendon tears or ruptures, and it is caused by the sudden release of tension within the tendon fibers [2].
Degeneration of the Achilles tendon, known as Achilles tendinopathy, can increase the risk of rupture. Tendinopathy is a condition characterized by chronic degeneration and structural changes within the tendon. It is often caused by repetitive overuse, poor biomechanics, or inadequate healing of a previous injury. [2] When the Achilles tendon undergoes degeneration, the tendon fibers become weaker, less organized, and more prone to injury. The tendon may develop small tears or areas of focal thickening. These degenerative changes compromise the structural integrity of the tendon, making it less capable of withstanding the forces placed upon it during physical activity [2].
The weakened tendon is more susceptible to rupture, particularly when sudden and forceful movements or excessive strain are applied. Activities that involve explosive movements, such as sprinting, jumping, or sudden changes in direction, can put immense stress on the Achilles tendon. In individuals with degenerated tendons, these forces can exceed the tendon’s capacity, leading to a rupture [2].
Additionally, certain risk factors can contribute to tendon degeneration and increase the likelihood of rupture. These include advanced age, obesity, smoking, systemic diseases such as diabetes or rheumatoid arthritis, and the use of certain medications, such as corticosteroids. These factors may impair the tendon’s ability to heal and repair itself, further predisposing it to degeneration and subsequent rupture [2]. It’s important to note that while degeneration increases the risk of Achilles tendon rupture, not all individuals with tendon degeneration will experience a rupture. However, the presence of degeneration should be taken seriously, as it indicates an underlying weakness in the tendon that may require intervention or modification of activities to prevent further injury [2].
The most common cause of Achilles tendon ruptures is a sudden and forceful contraction of the calf muscles, typically during activities that involve explosive movements or intense strain on the tendon. This can occur while running, jumping, or participating in sports such as basketball or soccer. Chronic Achilles tendinopathy, a condition characterized by degeneration of the tendon, can also increase the risk of rupture [2].
Metabolic health
It is important to emphasize that in order to maximize treatment potential, the patient’s overall metabolic status must be adequately balanced in terms of inflammation. Metabolic disorders, such as obesity, diabetes, and insulin resistance, are characterized by dysregulation of metabolic processes in the body [4]. They often involve chronic low-grade systemic inflammation, which is a state of prolonged, mild inflammation that persists in the absence of overt symptoms [5]. This type of inflammation is typically associated with increased levels of inflammatory markers, such as C-reactive protein (CRP) and interleukin-6 (IL-6), in the bloodstream [6]. Low-grade systemic inflammation is believed to arise from several factors related to metabolic disorders. These include increased adipose tissue mass, particularly in the abdominal region, which is metabolically active and releases pro-inflammatory substances called adipokines [4]. Adipokines, such as leptin and adiponectin, can influence the immune system and contribute to chronic inflammation [4]. In addition, metabolic disorders often involve dysregulation of glucose and lipid metabolism. High blood glucose levels, as seen in diabetes or insulin resistance, can activate inflammatory pathways and promote the release of pro-inflammatory molecules [7]. Dyslipidemia, characterized by abnormal levels of cholesterol and triglycerides, can also contribute to systemic inflammation through mechanisms such as oxidative stress and the activation of immune cells [8].
The inflammatory molecules circulating in the bloodstream can directly affect the tendon’s structure and integrity [9]. They can stimulate the production of matrix metalloproteinases (MMPs), enzymes that break down the extracellular matrix of the tendon [9]. Excessive MMP activity can lead to collagen degradation, weakening the tendon’s mechanical properties and making it more susceptible to injury [9].
Chronic inflammation can impair the tendon’s blood supply. Inflammatory molecules can disrupt the delicate balance between the production of new blood vessels (angiogenesis) and their regression (remodeling) [10]. This disturbance in angiogenesis can compromise the tendon’s ability to receive sufficient oxygen and nutrients, impairing its healing capacity [11]. Moreover, it can also interfere with the controlled inflammatory response necessary for tendon healing [10]. Inflammation is a normal part of the tissue repair process and involves the activation of immune cells, release of growth factors, and recruitment of reparative cells. However, in the presence of chronic inflammation, this healing response can become dysregulated. The prolonged inflammatory state can disrupt the balance between pro- inflammatory and anti-inflammatory signals, leading to an impaired healing environment within the tendon [10]. It is important to note that other elements of a patient’s lifestyle may also contribute to metabolic dysregulation, making them more susceptible to chronic inflammation and the risk of Achilles tendon rupture. These elements include sleep patterns, diet, the intestinal microbiome, and the use of certain drugs or medications [12].
Therefore, the combination of a weakened tendon structure, compromised blood supply, and impaired healing response increases the risk of Achilles tendon rupture [13]. Even relatively minor stresses or movements that would typically be well-tolerated by a healthy tendon can lead to a rupture when the tendon’s integrity has been compromised by chronic inflammation.
Treatment approach
Once an Achilles tendon rupture is suspected, it is crucial to seek immediate medical attention. A physician will typically perform a physical examination, which may involve squeezing the calf muscles to check for a gap or deformity in the tendon. Imaging tests, such as an ultrasound or MRI, can confirm the diagnosis and determine the extent of the injury [2].
The treatment of Achilles tendon ruptures can be either surgical or non-surgical, depending on various factors, including the severity of the rupture, the patient’s age, activity level, and overall health. Non-surgical treatment typically involves immobilizing the ankle in a cast or walking boot and utilizing crutches to reduce stress on the injured leg. Physical therapy and rehabilitation exercises are crucial for strengthening the tendon and restoring flexibility and function [2,14]. Surgical intervention may be recommended for more severe ruptures or for individuals who are physically active and require a quicker recovery. Surgery involves reattaching the torn ends of the tendon using sutures or other surgical techniques. Following surgery, a period of immobilization is required, followed by a gradual rehabilitation program [2,14]. Regardless of the chosen treatment approach, recovery from an Achilles tendon rupture is a gradual process. It can take several months before individuals can return to their pre-injury level of activity. Rehabilitation plays a vital role in rebuilding strength, flexibility, and coordination of the affected leg [2,14].
Surgical intervention
Surgical intervention for Achilles tendon rupture has long been considered the gold standard, particularly for athletes and active individuals who require a speedy recovery. Many studies support the efficacy of surgery in terms of restoring the tendon’s strength and function. The utilization of techniques such as percutaneous or open repair, with or without reinforcement, has demonstrated favorable outcomes in terms of tendon healing and patient satisfaction [14,15].
However, it is worth noting that surgical management does not come without potential drawbacks. There are risks associated with surgical complications, such as infection, wound healing problems, and nerve damage. Additionally, the recovery process following surgery can be demanding, involving an extended period of immobilization and rehabilitation. Despite these considerations, surgery remains a viable option for those seeking an accelerated recovery and a quicker return to physical activities [14,15].
Conservative approach
On the other hand, conservative (non-surgical) treatment approaches have also been explored for Achilles tendon rupture, particularly for individuals with lower functional demands or those who prefer to avoid surgery. Functional bracing, early mobilization, and physical therapy can yield satisfactory outcomes in some cases [14,15]. Conservative management aims to facilitate natural healing processes and gradual tendon remodeling without surgical intervention. It typically involves a combination of immobilization in a cast or boot followed by a progressive rehabilitation program. This strategy can lead to good functional outcomes, reduced complication rates, and improved patient satisfaction, particularly for individuals with a lower activity level [14,15]. However, conservative treatment does come with its own limitations. The healing process may be slower compared to surgery, and there is a risk of re-rupture or elongation of the tendon during the non-operative phase. It is crucial to carefully select appropriate candidates for conservative treatment, considering factors such as patient age, activity level, and the extent of the tendon rupture [15,16].
Orthobiologics
These hurdles led medical experts to seek alternative methods that are able to address tendon healing without increasing the risk of additional problems. Such alternatives are widely known as orthobiologics and have been the topic of extensive debate and contention in the scientific literature, particularly concerning their use in musculoskeletal regenerative medicine. Essentially, orthobiologics are biologically sourced products derived from substances inherent to the body, and they possess the capability to augment the healing response to orthopedic injuries [17]. Notable examples widely cited in the scientific literature include PRF and bone marrow products, particularly BMA [18, 19]. Such products are renowned for their abundance in cytokines and progenitor cell groups. They have showcased the ability to regulate the inflammatory responses seen in various orthopedic ailments that impact bone, cartilage, muscle, and tendons. This gives rise to significant hope and anticipation in the realm of regenerative medicine [20].
Bone Marrow Aspirate (BMA)
The bone marrow possesses a highly enriched molecular composition, abundant with cytokines and growth factors (Table 1) released by mesenchymal stem cells (MSCs). These components assist in attracting, modulating, and promoting anabolic activities within the microenvironment, thus aiding the regenerative process [17,21,22]. It’s important to note that the specific composition and concentration of growth factors in BMA may vary among individuals and depend on various factors, including age, health status, and the specific method used for BMA extraction and processing. These growth factors collectively contribute to the regenerative potential of BMA and its ability to enhance wound healing outcomes [23,24].
| Growth factor | Biological role |
|---|---|
| Platelet-Derived Growth Factor (PDGF) | PDGF plays a crucial role in promoting cell proliferation, angiogenesis, and extracellular matrix formation. It stimulates the migration and proliferation of various cell types involved in wound healing, including fibroblasts, endothelial cells, and smooth muscle cells. |
| Transforming Growth Factor-Beta (TGF-β) | TGF-β is a multifunctional growth factor that regulates cell growth, differentiation, and matrix production. It promotes the synthesis of collagen and other components of the extracellular matrix, thereby contributing to tissue remodeling and wound closure. TGF-β also modulates the immune response and has anti-inflammatory properties. |
| Vascular Endothelial Growth Factor (VEGF) | VEGF is a potent inducer of angiogenesis, the formation of new blood vessels. It stimulates the proliferation and migration of endothelial cells, leading to the formation of new capillaries in the wound bed. |
| Fibroblast Growth Factor (FGF) | FGFs are a family of growth factors that play a critical role in wound healing. They promote fibroblast proliferation and migration, which are essential for collagen synthesis and tissue remodeling. FGFs also stimulate angiogenesis, epithelial cell migration, and the production of extracellular matrix components. |
| Insulin-like Growth Factors (IGFs) | IGFs are involved in cell proliferation, differentiation, and tissue repair. They stimulate the synthesis of collagen and other matrix proteins, promote cell survival, and have anti-apoptotic effects. IGFs work in coordination with other growth factors to support the healing process. |
Table 1. Growth factors released by MSCs.
In addition to the important growth factors, BMA also holds a diverse range of cell populations. These can be categorized into non-hematopoietic cells - which consist of pericytes, endothelial cells, osteoblasts, adipocytes, and Schwann cells; and hematopoietic cells, which include neutrophils, lymphocytes, megakaryocytes, monocytes, and osteoclasts [25]. BMA extraction entails drawing bone marrow from an appropriate site, often the posterior iliac crest, with a specialized needle. The cells obtained from this process bolster the regenerative capabilities of BMA by encouraging angiogenesis, adjusting the immune response, and spurring tissue restructuring [23].
Moreover, MSCs can manipulate their immediate microenvironment and modulate the wound-healing cascade, reducing apoptosis and fibrosis, dampening inflammation and stimulating cell proliferation and differentiation via paracrine and autocrine pathways [26]. Additionally, they can downregulate synthesis of major pro-inflammatory cytokines, including interleukin
1 (IL-1), IL-6, interferon-γ (IFN-γ) and tumor necrosis factor-α (TNF-α) [27-29]. MSCs also exert an immune regulatory function as they are able to impede the activation of type 1 macrophage (MΦ1), natural killer (NK) cells, as well as B and T lymphocytes [30].
For these reasons, specifically, the application of this autologous orthobiologic material can work to the patient’s advantage and control the state of exacerbated inflammation in the extracellular environment of the injured area. The abundance of bioactive molecules and the diverse cell populations found in BMA provide indispensable support in the extracellular environment after tendon injuries.
Platelet-Rich Fibrin (PRF)
Fibrin, an integral component present in platelet-rich hemoderivatives, often doesn’t get the recognition it deserves despite its significant role in tissue repair. PRF, which is a notable source of fibrin, is recognized as a second-generation platelet concentrate. While it bears similarities to other platelet-rich products, PRF boasts certain advantages over the traditional platelet-rich plasma (PRP). For instance, PRP has some minor limitations related to blood handling and the necessity of adding anticoagulants, which PRF has effectively addressed [31]. This alternative biomaterial, in the form of a natural fibrin matrix, not only exhibits immunological and stimulatory characteristics but also encompasses all the hematological components intrinsically engaged in the healing process [31]. PRF mimics an autologous scar-forming matrix, derived purely from centrifuging peripheral blood without incorporating any external substances [32]. Indeed, this bio graft manifests as a fibrin-matrix polymer with a tetra molecular structure, encompassing platelets, leukocytes, cytokines, and even circulating stem cells within its makeup [33]. The inherent adhesive qualities of PRF present notable benefits. Due to its resilience, this material has the potential to remain in the targeted joints for an extended period. This duration facilitates a longer release of growth factors and maintains consistent cell adhesion and proliferation, enhancing the healing and regenerative process [34].
Studies suggest that, when compared to PRP, PRF might aid the healing process without inciting significant “flare-ups” which can sometimes occur following PRP injections, particularly when utilizing leukocyte-rich PRP [35]. PRF is versatile in its applications. It can be conveniently modified and utilized as a membrane, aiding in healing chronic wounds. Furthermore, it can be employed as a platelet gel in tandem with other biomaterials, like bone grafts, to enhance tissue regeneration and repair [36-39].
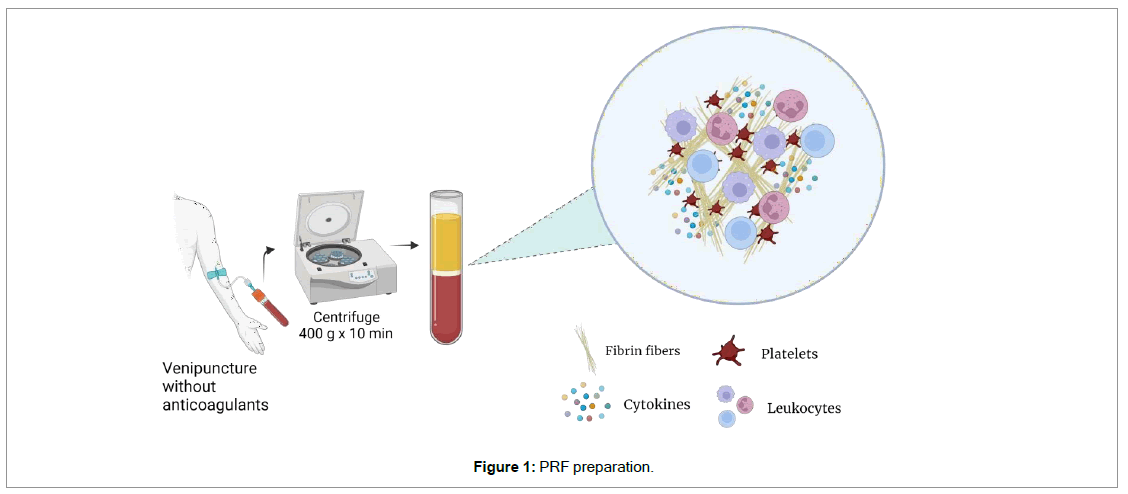
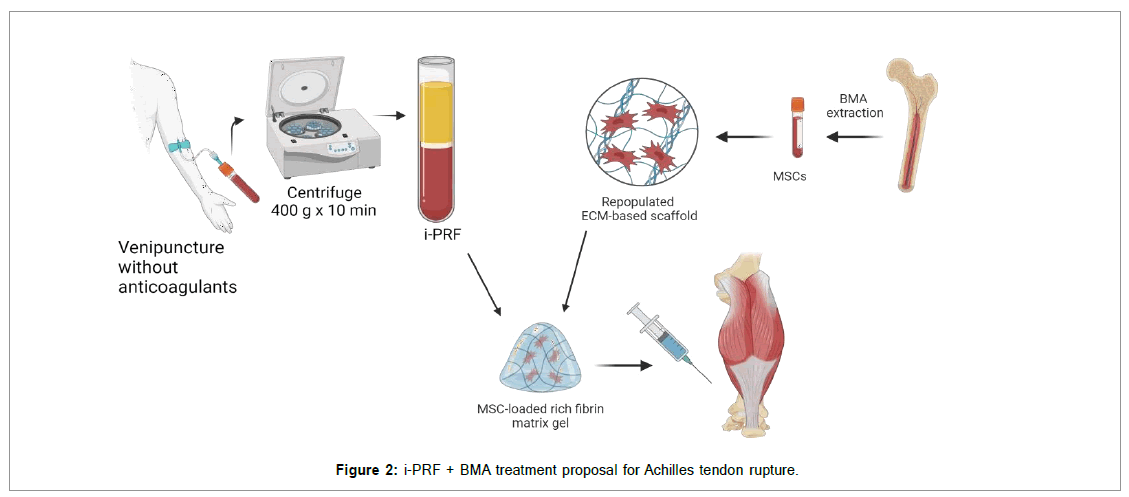
While numerous protocols outline the preparation of platelet concentrates, the process to create PRF is straightforward with only slight variations. Notably, the preparation of PRF begins with the omission of anticoagulants, which are recognized inhibitors of tissue regeneration [40]. To put it simply: a venipuncture is conducted, and blood is gathered into plastic tubes. These tubes might be coated with a clot activator (like glass, silica, or thrombin) to speed up the clotting process, but it’s not mandatory. After collection, the tubes are quickly put into a centrifuge, and they undergo a single centrifugation cycle, typically at 400 g for 10 minutes [41]. Following the centrifugation process, a layered mixture is obtained. The erythrocytes, being the heaviest particles, settle at the bottom of the suspension. Meanwhile, the platelet-poor plasma (PPP) is found in the uppermost portion of the tube (Figure 1). The fibrin clot, which materializes between the PPP and the erythrocyte layer, is the distinctive feature that accentuates PRF as a remarkable orthobiologic instrument. This clot captures platelets, leukocytes, and growth factors and components from BMA, transforming it into a natural and autologous bio scaffold (as illustrated in Figure 2).This makes it a dense depot of bioactive molecules essential for tissue repair and regeneration [41-45]. PRF can subsequently be effortlessly extracted from the tube using forceps, readying it for various applications.
There’s also an injectable variant of PRF, known as i-PRF, which provides greater flexibility in treatment options [40]. Injectable PRF is commonly prepared in vacuum tubes devoid of any additives, aiming to postpone the coagulation process. This delay grants practitioners ample time to handle the orthobiologic sample appropriately and administer an intra-articular injection. It’s important to highlight that PRP by itself is known to disperse quickly, which can occasionally diminish its therapeutic efficacy based on the injection site [46]. On the other hand, fibrin possesses the ability to maintain the contour of a joint for approximately 5 minutes post-injection, for example, ensuring that the product remains at the designated injection sites for longer periods [47]. This means that the robust fibrin matrix can hold the cells from BMA in the tendon target tissue and effectively modulate the healing cascade.
Conclusion
In conclusion, the management of Achilles tendon rupture involves a consideration of both surgical and conservative options. Surgery provides the potential for a quicker recovery and restoration of tendon function, especially for active individuals. On the other hand, conservative treatment can be a viable option for individuals with lower functional demands or those who prefer to avoid surgery, with satisfactory outcomes reported in selected cases. BMA and PRF are regenerative therapies used in wound healing. BMA contains various cell populations involved in tissue repair, while PRF provides a concentrated mixture of platelets, growth factors, and a robust fibrin matrix that supports cell activity. The combination of these two orthobiologic products may prove to be useful as it yields synergistic effects that can enhance wound healing outcomes by stabilizing tissue regeneration, angiogenesis and immune modulation processes.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi