Research Article, J Vet Sci Med Diagn Vol: 5 Issue: 6
Canine Filamentous Dermatitis Associated with Borrelia Infection
| Marianne J Middelveen1, Gheorghe M Rotaru2, Jody L McMurray2, Katherine R Filush3, Eva Sapi3, Jennie Burke4, Agustin Franco4, Lorenzo Malquori4, Melissa C McElroy1 and Raphael B Stricker1* | |
| 1International Lyme and Associated Diseases Society, Bethesda, Maryland, USA | |
| 2Heartland Veterinary Clinic, Airdrie, Alberta, Canada | |
| 3Department of Biology and Environmental Science, University of New Haven, West Haven, Connecticut, USA | |
| 4Australian Biologics, Sydney, New South Wales, Australia | |
| Corresponding author : Raphael B Stricker, M.D, International Lyme and Associated Diseases Society, Bethesda, Maryland, USA Tel: +(415) 399- 1035 Fax: (415) 399-1057 E-mail: rstricker@usmamed.com |
|
| Received: September 12, 2016 Accepted: September 28, 2016 Published: October 03, 2016 | |
| Citation: Middelveen MJ, Rotaru GM, McMurray JL, Filush KR, Sapi E, et al. (2016) Canine Filamentous Dermatitis Associated with Borrelia Infection. J Vet Sci Med Diagn 5:6. doi: 10.4172/2325-9590.1000212 |
Abstract
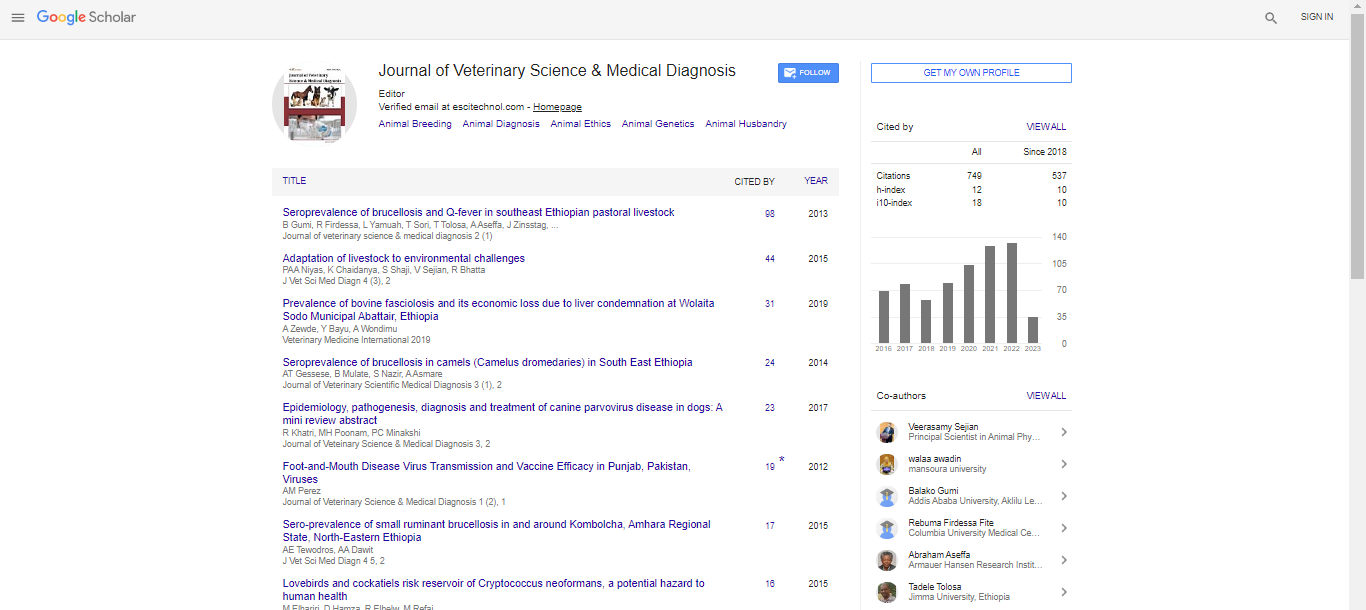
Canine Filamentous Dermatitis Associated with Borrelia Infection
Background: Although canine clinical manifestations of Lyme disease vary widely, cutaneous manifestations are not well documented in dogs. In contrast, a variety of cutaneous manifestations are reported in human Lyme disease caused by the spirochete Borrelia burgdorferi. A recently recognized dermopathy associated with tickborne illness known as Morgellons disease is characterized by brightly-colored filamentous inclusions and projections detected in ulcerative lesions and under unbroken skin. Recent studies have demonstrated that the dermal filaments are collagen and keratin biofibers produced by epithelial cells in response to spirochetal infection. We now describe a similar filamentous dermatitis in canine Lyme disease. Methods and Results: Nine dogs were found to have cutaneous ulcerative lesions containing embedded or projecting dermal filaments. Spirochetes characterized as Borrelia spp. were detected in skin tissue by culture, histology, immunohistochemistry, polymerase chain reaction (PCR) and gene sequencing performed at five independent laboratories. Borrelia DNA was detected either directly from skin specimens or from cultures inoculated with skin specimens taken from the nine canine study subjects. Amplicon sequences from two canine samples matched gene sequences for Borrelia burgdorferi sensu stricto. PCR amplification failed to detect spirochetes in dermatological specimens from four healthy asymptomatic dogs. Conclusions: Our study provides evidence that a filamentous dermatitis analogous to Morgellons disease may be a manifestation of Lyme disease in domestic dogs.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi