Case Report, J Regen Med Vol: 9 Issue: 1
Case Report: Psoriatic Arthritis and Stem Cell Therapy
Paul A Dreschnack1* and Marvell Scott2
1Saint Joseph’s Medical Center, New York, United States
2Boonshoft School of Medicine, Sports Medicine, Wright State University, United States
*Corresponding Author: Paul A Dreschnack
Plastic surgeon, Saint Joseph’s Medical Center, New York, NY 10036, United States
Tel: 2129831938
E-mail: drpaul@microsurgery.com
Received: December 10, 2019 Accepted: February 03, 2020 Published: February 10, 2020
Citation: Dreschnack PA, Scott M (2020) Case Report: Psoriatic Arthritis and Stem Cell Therapy. J Regen Med 9:1. doi: 10.37532/jrgm.2020.9(1).153
Abstract
We report a case of a 63-year-old patient with a 20-year history of psoriatic arthritis that covered 80% of her body. After failed methotrexate therapy, her symptomology was well controlled with topical clobetasol. After treatment with adipose-derived stem cells for a painful knee, her skin pathology disappeared for 7 months without any further treatment. When lesions did return, they were of less severity then usually seen.
Keywords: Methotrexate therapy; Psoriatic arthritis; Stem cell therapy
Introduction
Psoriatic arthritis (PsA) is a progressive autoimmune inflammatory disease that is often difficult to differentiate from rheumatoid arthritis. Investigations into classification and diagnostic criteria have been intensively investigated [1].
Often it begins as eczema in the teenage years, progresses to psoriasis at middle age, and evolves into bone and joint arthropathy. Joint erosion causes pain, which causes patients to seek medical assistance. Multiple internal organ systems may become involved with the debilitation that can be expected with chronic inflammatory diseases.
Treatment historically involves topical steroids, oral prednisone, methotrexate, and non-steroidal anti-inflammatory medications. Biologic anti-inflammatory medications are becoming popular with excellent television marketing programs. These newer medications function to control joint inflammation and reduce skin manifestations by interfering with tumor necrosis factor α.
Here we discuss a woman who presented with unilateral knee pain. She controlled her skin outbreaks with topical clobetasol after failed methotrexate therapy. Immune modulation is a new field of study for stem call therapy and exosome therapy. PsA patients often fail one therapy or another. Undesirable side effects of medications and loss of efficaciousness of medications frequently cause these patients to attempt different regimens for treatment. Many patients become frustrated at the insidious progression of the disease, the side effects and failed therapy. This presentation is significant in that it offers another viable alternative that limits side effects and still produces satisfactory results.
Case Report
A 63-year-old female medical office employee had a 20-year history of psoriatic arthritis. She sought medical attention because she had progressive left knee pain that limited her ability to ambulate, particularly ascending stairs. Her dermatopathology initially appeared as eczema in her teen years, involving all extremities and her thorax anteriorly and posteriorly. Over time, the eczema progressed to psoriasis at about age 40 years, and the psoriasis progressed to psoriatic arthritis at approximately age 60. In the past two years, 80% of her skin body surface area was affected with the disease. Methotrexate usage controlled her skin lesions initially, but as the disease progressed, it lost its efficaciousness after four years (July 2008 to February 2012), and was discontinued by her physician. Attempts to control her skin lesions were abandoned due to her allergies to NSAIDS, and lack of continued responsivity to methotrexate. At times of symptomology, topical clobetasol cream was her medication of choice, and gave her the most relief. Clobetasol usually successfully reduced her lesions to erythema on her thorax; however, the extremity symptomology was more difficult to control. She had been on topical clobetasol for a week prior to her first office visit.
Orthopedically, there was a history of pes planus and genu varum. A former Jazzercise and Zumba student in 2009, she began to develop left knee pain, and changed to Yoga, which she felt would be less stressful on her joints. In 2015, she felt a pop in her left knee in Yoga class, and wore a brace on her left knee for 2 years. An MRI was obtained on consultation which showed a torn medial meniscus.
A diagnosis of iritis had been previously established, and scleritis developed in 2008, which was treated with prednisone eye drops. Oral prednisone was added for 4 months in 2008 at a dosage of 20 mg twice a day. There were no further issues of ophthalmological pathology. She generally felt that she fared better in summer months with her skin lesions, but had a flare up three days prior to appearing in the office for a consultation in November of 2017. On this occasion she was applying clobetasol cream to her legs. She was not a good candidate for usage of hydroxychloroquine, as she had a history of ophthalmological problems (iritis and scleritis) in the past. Tumor necrosis factor blocking medications such as etanercept (Enbrel®), infliximab (Remicade®), adalimumab (Humira®), golimumab (Simponi®), and certolizumab pegol (Cimzia®) are newer medications that she has not attempted treatment with, as most did not exist at the time of her treatment. Her physician entertained the idea of starting her on Enbrel® (etanercept), however she had a family history of lung cancer, so it was determined not to be a viable possibility. Ustekinumab (Stelara®), which block interleukins, also was not attempted. Neither were Apremilast (Otezla®) or Secukinumab (Cosentyx®) seemingly due to failed therapy with methotrexate in the past.
Medically, there was a history of hypertension, occasional benign preventricular contractions, and hypercholesterolemia. Medication at the time of examination included lisinopril, hydrochlorothiazide and rosuvastatin. Allergies included non-steroidal anti-inflammatory drugs, and penicillin, both of which produced wheezing and urticaria. A moderate cigarette smoker, she quit in 1995 after smoking for many years. There was no history of alcohol consumption.
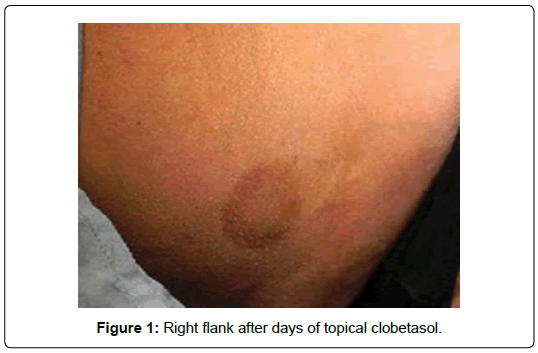
On examination, she was five feet seven inches tall, and weighed 205 pounds, with a pyknic habitus. Psoriatic plaques were limited to the extremities. The thorax anteriorly and posteriorly did not have plaques, but rather erythema in the flanks at the time of examination (Figure 1).
Lesions of the extremities had an erythematous base around the plaque. The left knee showed mild pain on palpation of the joint medially and laterally, and on range of motion with full knee flexion and extension. There was a click on knee extension - a positive McMurray test, and a negative drawer sign. Her hands exhibited mild joint soreness, but overt joint deformities were absent. Clubbing was absent. Joint deformities were likewise absent on all extremities.
Mesenchymal stem cell (MSC) harvest was performed with IV sedation utilizing a super-wet technique and the Tulip aspiration system. 120 mL of adipocyte lipoaspirate was sent to the laboratory for cell isolation. This was achieved via ultrasound separation at Advanced Therapeutics Labs in New York City. An intra-articular left knee injection was performed under 1% Lidocaine local anesthesia, and a drip of intravenous mesenchymal stem cells was administered. Cell counts determined by Advanced Therapeutics Lab were 336,000,000. Twenty-four hours later, the patient returned to work. Her discomfort rapidly improved, and reported that she could ascend steps with mild residual discomfort.
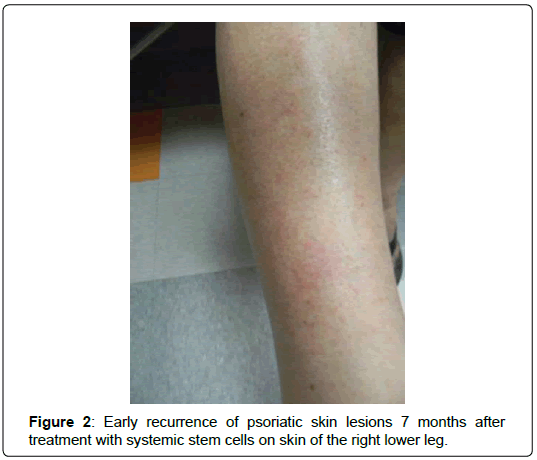
One-week postoperatively, she noticed that her skin lesions had markedly improved. By four weeks, all skin lesions had disappeared completely, although she still had mild left knee pain. Skin lesions were absent completely for seven months postoperatively. After this period of time, they began to return on the thorax and extremities (Figure 2). She did receive two additional interarticular injections into the left knee with “some improvement” in her discomfort, but did not receive any additional systemic intravenous therapy (other than the single treatment at the time of cell harvest). When the skin lesions returned, they were not as severe as her usual outbreaks that occurred prior to stem cell treatment. After one year, they were limited to clusters on the lower extremities, elbows and thorax (Figure 3).
Discussion
Obviously psoriatic arthritis is a disease characterized by chronic inflammation, and significant frustration for the patient who has it. We expect to find low immunomodulatory cytokines, and high interferon-gamma (INF- Ɣ) levels. The chronic inflammation prevents the skin manifestations from healing. Mesenchymal stem cells contribution to embryogenesis has a long history from its theoretical bone marrow derived fibroblasts by Cohnheim 1867, to the in-utero repair of cleft lips, and the identification of surface antigens [2-4]. There are innumerable papers on the trophic properties, antiinflammatory, immunomodulatory and anti-apoptotic properties of MSCs [5,6]. The inflammatory properties of chronic psoriatic lesions impede the healing process of normal mature cells. Interleukin-1 (IL-1), interlukin-2 (IL-2) and IL-12 are elevated, as is interferon-gamma (INF- Ɣ). MSC’s respond by increasing IL-4 and IL-10. The increase of IL-4, 5 and 13, and decrease of INF-Ɣ shift macrophages from the pro-inflammatory state (M1) to the anti-inflammatory state (M2). The increased IL-4 and IL-10 fortify the Helper T cells-2 (TH2), thus increasing rapidly to counter the pro-inflammatory Helper T cells-1 (TH1), and thus reduce the chronic inflammation [7].
Margaret Coutts in her recent article presented a patient that failed all standard treatment modalities, but did respond to treatment with stem cells with an excellent outcome [8]. A C Woods presented a review of PsA patients treated with stem cells that had a remission of at least one year, with reports of varying lengths of known patients at that time [9].
Conclusion
This particular patient sought medical attention not for dermatopathological resolution, but for relief of joint pain. Antiinflammatory proteins make a sizable contribution to the relief that this patient is experiencing. The immunomodulatory cytokines, macrophage shift and T-Helper cell shift together relieved the dermatological symptomatology completely for seven months. After seven months, the lesions gradually began to return as punctate dermal lesions on the thorax and extremities. However, with significantly less virulence then she had exhibited prior to treatment. The returning lesions averaged 1.2 cm x 0.4 cm. The large plaques present prior to treatment did not return at the time of this submission, 21 months after surgery. After a lengthy history of skin pathology, the overall presentation of the skin manifestations is significantly improved. Most importantly, she finds satisfaction with the final outcome.
References
- Helliwell PS, Taylor WJ (2005) Classification and diagnostic criteria for psoriatic arthritis. Ann Rheum Dis 64: ii3-ii8
- Cohnheim J (1867) About inflammation and suppuration. Arch für Pathologische Anatomie und Physiologie und für Klinische Medicin 40: 1-79.
- Longaker, M, Whitby D, Adzick N, Crombleholme T, Langer J, et al. (1990) Fetal wound healing, IV. Second and early third trimester fetal wounds demonstrate rapid collagen deposition without scar formation. J Pediatr Surg 25: 63-69.
- Haynesworth S, Baber M, Caplan A (1992)Cell surface antigens on human marrow-derived mesenchymal cells are detected by monoclonal antibodies. Bone 13: 69-80.
- Iyer S, Rojas M (2008) Anti-inflammatory effects of mesenchymal stem cells: novel concept for future therapies. Expert Opin Biol Ther 8: 569-582.
- Uccelli, Moretta L, Pistoia V (2008) Mesenchymal stem cells in health and disease Nat Rev Immunol 8: 726-736.
- Aggarwal S, Pittenger M (2005) Human mesenchymal stem cells modulate allogenic immune cell responses Transplantation. Blood 105:1815-1822.
- Coutts M, Soriano R, Naidoo R, TorfH (2017) Umbilical cord blood stem cell treatment for a patient with psoriatic arthritis. World J Stem Cells 9: 235-240.
- Woods AC, Mant MJ (2006) Amelioration of severe psoriasis with psoriatic arthritis for 20 years after allogeneic haematopoietic stem cell transplantation. Ann Rheum Dis 65: 697.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi