Case Report, Int J Ophthalmic Pathol Vol: 12 Issue: 4
Cataract Extraction on One Seeing Eye in Patient with Behcet’s Disease
Nurul Fitri Shabrina* and Randi Montana
Department of Infection and Immunology, Airlangga University, Surabaya, Indonesia
- *Corresponding Author:
- Nurul Fitri Shabrina
Department of Infection and Immunology,
Airlangga University,
Surabaya,
Indonesia;
Email: nurulfshabrina@yahoo.com
Received date: 18 May, 2020, Manuscript No. IOPJ-20-11056;
Editor assigned date: 21 May, 2020, PreQC No. IOPJ-20-11056 (PQ);
Reviewed date: 4 June, 2020, QC No. IOPJ-20-11056;
Revised date: 16 August, 2023, Manuscript No. IOPJ-20-11056 (R);
Published date: 13 September, 2023, DOI: 10.4172/2324-8599.12.3.031
Citation: Shabrina NF, Montana R (2023) Cataract Extraction on One Seeing Eye in Patient with Behcet’s Disease. Int J Ophthalmic Pathol 12:4.
Abstract
Introduction: Behcet’s disease is autoimmune relapsing systemic vasculitis of unknown that can cause uveitis and affect the anterior and posterior segment of the eye. Cataract is the most common complication of anterior segment caused by recurrent uveitis. This case was to report the outcomes and complications of cataract surgery in patients with Behcet's disease.
Case report: A of 35 years old man complained progressive visual loss since 6 months before admission with VA 1 meter finger counting and NLP. There was history of recurrent redness on both eyes accompanied by blurred vision and pain, oral aphtosis and genital aphtosis since three years before admission but didn’t seek help because of low access to healthcare in his previous home. From anterior segment examination there was posterior synechia, cloudy lens, pupil secclusion, rubeosis iridis, flare and cell suggesting chronic uveitis. There was elevated IOP of 43.4 mmHg on left eye. Retinal vasculitis was found on posterior segment examination.
Results: After combination of methylprednisolone and azathioprine for one year, there were improvement of quieter condition on both eyes and decreased left eye IOP of 37.2 mmHg. Lens extraction with iris retractor was done after three months of no inflammatory response. Despite uneventfull surgery and combination of immunosupresive medication, the visual acuity are not much improved and there was optic atrophy from the complication of chronic Behcet’s disease.
Conclusion: In patient with chronic Behcet’s disease, ocular involvement can affect both anterior and posterior segments with poor visual outcome regarding its complication
Keywords: Behcet’s disease; Cataract extraction; One-seeing
eye; Lens extraction
Introduction
Behcet's disease is an autoimmune, rare and severe chronic multisystemic inflammatory disease and characterized by recurrent oral aphthous ulcers, genital ulcers, skin lesions and both anterior and posterior uveitis. It is observed commonly among population in mediterrania, middle east and east Asia. The pathogenesis of Behcet’s disease is still unknown. Infection, HLA-B51 and environmental factor are some hypothesis that suspected to be the cause of Behcet’s disease [1].
Ocular manifestation of Behcet’s disease can be sight threatening because of relapsing uveitis that may involve anterior segment, posterior segment or both and may have several complication including optic atrophy, retinal detachment and secondary glaucoma which can all lead to blindness if treatment is delayed. The goal treatment of Behcet’s disease are to control chronic inflammation and decrease the number of relapse with corticosteroid and immunosuppressive theraphy. Azathioprine and corticosteroid are recommended as initial therapy for patient with ocular manifestation of Behcet’s disease [2].
Cataract is the most frequent complication in anterior segment in patient with Behcet’s disease because of recurrent attack of uveitis and corticosteroid use to control the disease. Like the other complicated cataract cause by uveitis, the surgical decision is based on etiology, duration and inflammation activity of the disease. Surgical removal in such cataract requires different approach in pre and post-operative period to prevent the risk of immediate severe inflammation after surgery. The surgery also requires additional manipulation such as dissection of synechias and iris retractors. The implantation of intraocular lens was also controversial in the complicated cataract [3].
Case Presentation
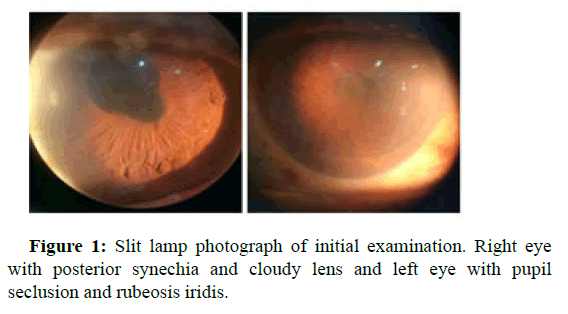
A 35 years old man complained progressive visual loss since 6 months before admission on both eyes with VA 1 meter finger counting and NLP. There was history of recurrent redness on both eyes accompanied by blurred vision and pain, oral aphtosis and genital aphtosis since three years before admission but didn’t seek help because of low access to healthcare in his previous home. From anterior segment examination there was posterior synechia, cloudy lens, flare and cell on the right eye and pupil secclusion, rubeosis iridis and elevated IOP of 43.4 mmHg on left eye suggesting chronic uveitis (Figure 1) [4].
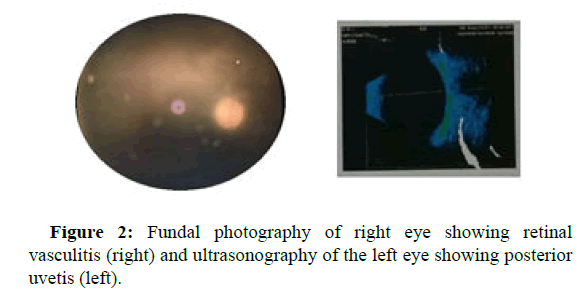
Retinal vasculitis was found on posterior segment examination on right eye and there was echogenic lession particle shaped with 20% echospike of RCS complex suggesting posterior uveitis found on USG on left eye (Figure 2) [5].
The patient was diagnosed with Behcet’s disease and was given the combination of corticosteroid and immunosuppressive of methylprednisolone 16 mg three times a day and azathioprine 50 mg three times a day. The patient also given topical corticosteroid, topical midryating and cyclopegic agent to prevent further synechia. Glaucoma medication was also given to control increased IOP. Despite all the medication, Behcet’s disease in this patient are hard to control because of the nature of recurrent uveitis in this disease. The patient also report side effect of prolonged corticosteroid use like weight gain and moon-face and there was also side effect of leucopenia and increased liver function that causing halt of the azathioprine use by several weeks [6].
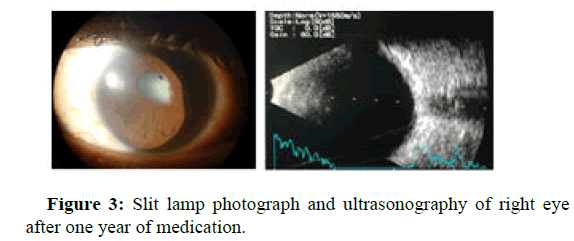
After one year of medication, the combination on immunosuppressive and corticosteroid are able to control the disease. There were improvement of quieter condition on both eyes and decreased left eye IOP of 37.2 mmHg. But there are worsening of cataract condition of right eye causing decrease visual acuity to become LP (+). Cataract condition are making the evaluation of posterior segment difficult to be done but the ultrasonography shows that there are no posterior uveitis. Lens extraction with iris retractor was discussed as an attempt to improve the visual acuity and evaluate the condition of posterior segment (Figure 3) [7].
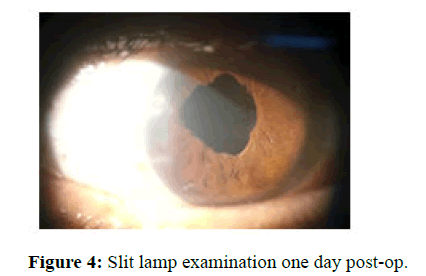
The surgery were being done after inflammation were controlled and the anterior chamber is free from cells for at least three months. The patient was given his usual regimen of immunosuppressive with additional IV methyl prednisolone 250 mg 4 times a day for 3 days before and after operation. The operation was done with phacoemulsification technique with synechia dissection and iris retractors. The surgery went uneventfull and there was no complication during surgery. One day after the operation, there was no flare and cell in sight and there was improvement of visual acuity of hand movement (Figure 4) [8].
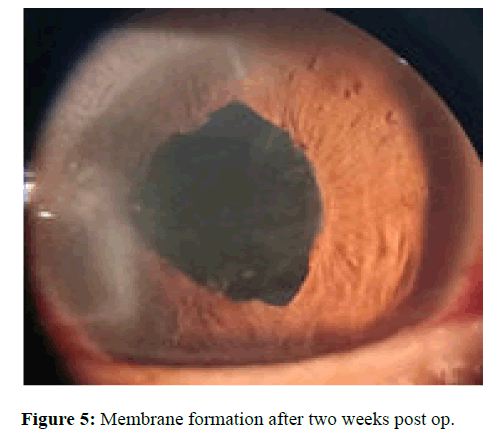
Patient then discharged after three days observation and inflammation control with no recurrence of uveitis during the admission in hospital. Two weeks after the operation, there was membrane formation in the IOL and cells in anterior chamber despite the immunosuppressive and corticosteroid therapy. Visual acuity is still at hand movement and upon examination there was optic atrophy that causing decreased vision (Figure 5) [9].
Results and Discussion
Behcet’s Disease (BD) is a chronic, relapsing, inflammatory vascular disease known to affect adult male younger than 40 years old. The etiology of Behcet’s disease is unknown, genetic and environmental factors are thought to be associated with the development and progression of the disease. Infectious agents, such as herpes simplex virus, hepatitis viruses, parvovirus and Streptococcus sanguis have been predicted as causes of Behcet’s disease [10].
Clinical features of Behcet’s disease include oral and genital ulcers, ocular inflammation, skin lesions and more rare condition such as articular, vascular, neurological, pulmonary, gastrointestinal, renal, vascular and genitourinary manifestations. The disease may start with one or more of the above symptoms but other symptoms may gradually appear over the years.
The ophthalmic manifestation of Behcet’s disease is seldom the initial manifestation and can occurs years after the first oral ulcers. Uveitis is the most common symptom and occurs in approximately two-thirds of patients with Behcet’s disease. The uveitis have feature of relapsing and can affect bilateral anterior and posterior segment of the eye and can be vision threatening if treatment is delayed. A single attack will usually heal spontaneously without producing any sequelae. However, because of the relapsing nature of it, it can lead to blindness if treatment is delayed. Most vision-threatening conditions were of posterior segment origin and were largely inversely correlated with the presence of genital ulcers and systemic vasculitis [11].
There are no gold standard criteria for the diagnosis of Behcet’s disease because there are no specific laboratory tests or pathognomonic findings. Two of the most commonly used classification criteria are the ICBD (International Criteria for Behcet’s Disease) and the ISG (International Study Group) criteria. The ISG criteria states that recurrent oral ulcer that occurs at least three times a year, is mandatory for the diagnosis. In addition, two of the four major symptoms, including eye lesion, recurrent genital ulcers, skin lesions and a positive pathergy test, are sufficient for the diagnosis of Behcet’s disease. Whereas ICBD states that there are four major and five minor criteria. The major criteria include recurrent aphthous ulcers, skin findings (similar of those erythema nodosum or acne and a pathergy test), genital ulcers and ocular involvement. The minor criteria include arthritis, intestinal ulcers, epididymitis, vascular disease and neuropsychiatric involvement. This diagnostic system requires only one major symptom in addition to typical ocular symptoms for the diagnosis of ocular Behcet’s disease.
In this case the patient present with recurrent genital and oral ulcer for over three years prior to admission and patient also have recurrent red eye that have mild pain for the course of three years. Suggesting that Behcet’s disease of this patient had happen long before patient seek help to hospital. In the initial examination, there are the signs of active uveitis of flare and cells in anterior chamber, posterior uveitis and vasculitis. There was also signs of chronic uveitis in forms of posterior synechia, cloudy lens and pupil seclusion. There was also elevated IOP on left eye with presence of rubeosis iridis suggesting that the glaucoma of the left eye is caused by neovascular or uveitic glaucoma from the complication of chronic relapsing uveitis. Because of recurrent aphthous ulcers, skin findings, genital ulcers and ocular involvement, this patient meet the classification criteria of Behcet’s disease in both ICBD and ISG [12].
The goal treatment of Behcet’s disease are to control chronic inflammation, reduce the frequency and severity of recurrences and decrease the number of relapse to minimize the involvement of posterior segment. To be effective, treatment must be started early. Corticosteroids is the most useful agent in the treatment of explosive inflammation of the anterior and posterior segments, prednisone doses of 1.5 mg/kg/day (with taper) are most beneficial for controlling acute inflammation as well as pulse dose steroids (1 g intravenous methylprednisolone infusions daily) are often used for 3 days if there are severe manifestation. Topically applied corticosteroid eye drops together with mydriatics or cycloplegic agents can often control the disease especially in mild anterior uveitis. Immunosuppressives can also be combined in those patients whose eye disease is refractory to treatment. Azathioprine and corticosteroid are recommended as the initial therapy for all patients with BD with inflammation of the posterior segment of the eye. A retrospective analysis of 157 consecutive patients with severe uveitis (active posterior uveitis or panuveitis) treated with corticosteroids (0.5 mg/kg/day-1 mg/kg/day) and azathioprine (2.5 mg/kg/day) revealed that posterior uveitis was controlled in 92.9% of patients, of whom 51.6% were complete responders and 41.4% were partial responders. In this case patient already got the combination of azathioprine 50 mg three times a day and methyl prednisolone 16 mg three times a day. Patient also got midryatic and cyclopegic drops for preventing further synechia and anti glaucoma medication for decreasing the IOP. Quiet condition of the eye and uveitic episode are controlled after one year of therapy, but visual acuity are decreased to light perception due to cataract. The posterior segment are difficult to evaluate but ultrasonography shows no posterior uveitis.
Cataract in uveitis may develop as a result of the intraocular inflammation and chronic corticosteroid usage or both. Surgery is indicated whenever visual improvement can be expected and the eye has been free of inflammation for a minimum of 3 months. For succcesfull surgery, the surgeon must ensure that uveitis should be inactive for at least 3 months preoperatively, systemic and topical steroids should be used prophylactically for 1 week preoperatively and continued postoperatively, immunosuppressive drugs should be continued. Additional step like synechiolysis, remove pupillary membranes, perform pupillary relaxing incisions or sphyncterotomies or using iris retractor hooks are sometimes needed to maintain adequate pupil size during surgery. The surgeon must ensure complete removal of cortical material should take place and one-piece PMMA posterior chamber intraocular lens should be used. The surgeon and patient must understand the special nature of this surgery, its risks and the prognosis for success. The cataract surgery in this patient are done with combination of corticosteroid and immunosuppressive agent as well as IV corticosteroid three days before and after operation. The surgery went uneventfull with phacoemulsification technique and IOL implantation with additional synechiolysis and iris retractors to maintain adequate pupil size.
The outcomes of visual acuity after cataract extraction are guarded in patient with Behcet’s disease. Patients with Behcet's disease related to intraocular inflammation appeared to have a higher risk for complications and therefore worse outcomes than patients with other clinical etiologies of uveitis. Berker et al., reported results of 72.5% improvement in vision after surgery of phacoemulsification and intraocular lens implantation in patients with Behcet’s disease However, the vision got worse in 17.5% of the eyes. Most frequent complication reported by them was posterior capsular opacification in 37.5% of eyes. Other complications were posterior seynchiae and severe inflammation. Posterior segment complications such as epiretinal membrane formation, cystoid macular edema and optic atrophy. In this patient despite the surgery being uneventfull and intense medication support of immunosuppressive and corticosteroid agent, the visual outcomes after surgery did not improved much from light perception to hand movement. There was membrane formation behind the intraocular lens as fast as two weeks after surgery suggesting the formation of posterior capsular opacity which is one of the postoperative complications after cataract surgery in eyes with uveitis. Upon examination of posterior segment there was also optic atrophy which is one of chronic manifestation of Behcet’s disease that causing irreversible visual loss.
Conclusion
In patient with chronic Behcet’s disease, ocular involvement can affect both anterior and posterior segments with poor visual outcome regarding its complication. Complications like retinal detachment, secondary glaucoma and optic atrophy often cause irreversible visual loss. It is thus very important for an ophthalmologist to be able to predict which case of Behcet’s disease will pursue a vision-threatening course and which case will not. To date, no enough data exists regarding the presence of general predictors for vision-threatening disease. If vision-threatening disease has certain predictors.
References
- Paovic J, Paovic P, Sredovic V (2013) Behcet’s disease: Systemic and ocular manifestations. Biomed Res Int 2013: 247345.
[Crossref] [Google Scholar] [PubMed]
- Leonardo NM, McNeil J (2015) Behcet’s disease: Is there geographical variation? A review far from the silk road. Int J Rheumatol 2015: 945262.
[Crossref] [Google Scholar] [PubMed]
- Hussein MA, Eissa IM, Dahab AA (2018) Vision-threatening Behcet’s disease: Severity of ocular involvement predictors. J Ophthalmol 2018: 9518065.
[Crossref] [Google Scholar] [PubMed]
- Saleh Z, Arayssi T (2014) Update on the therapy of Behcet disease. Ther Adv Chronic Dis 5: 112-134.
[Crossref] [Google Scholar] [PubMed]
- Kadayifcilar S, Gedik S, Eldem B, Irkec M (2002) Cataract surgery in patients with Behcet’s disease. J Cataract Refract Surg 28: 316-320.
[Crossref] [Google Scholar] [PubMed]
- Rokutanda R, Kishimoto M, Okada M (2014) Update on the diagnosis and management of Behcet’s disease. Open Access Rheumatol Res Rev 30: 1-8.
[Crossref] [Google Scholar] [PubMed]
- Alpsoy E (2012) New evidence-based treatment approach in Behcet's disease. Pathol Res Int 2012: 871019.
[Crossref] [Google Scholar] [PubMed]
- Saadoun D, Wechsler B, Terrada C, Hajage D, Le Thi Huong D, et al. (2010) Azathioprine in severe uveitis of Behcet's disease. Arthr Care Res 62: 1733-1738.
[Crossref] [Google Scholar] [PubMed]
- Agrawal R, Murthy S, Ganesh SK, Phaik CS, Sangwan V, et al. (2012) Cataract surgery in uveitis. Int J Inflamm 2012: 548453.
[Crossref] [Google Scholar] [PubMed]
- Berker N, Soykan E, Elgin U, Ozkan SS (2004) Phaco emulsification cataract extraction and intraocular lens implantation in patients with Behcet's disease. Ophthalmic Surg Lasers Imaging Retina 35: 215-218.
[Google Scholar] [PubMed]
- Shabrina NF, Hermawan D, Montana R (2020) Cataract extraction on one seeing eye in patient with Behcet’s disease. Ann Mech Inst 4: 83-87.
- Busbee BG, Brown MM, Brown GC, Sharma S (2003) Cost-utility analysis of cataract surgery in the second eye. Ophthalmol 110: 2310-2317.
[Crossref] [Google Scholar] [PubMed]
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi