Research Article, Int J Ophthalmic Pathol Vol: 11 Issue: 5
Changes in Intraocular Pressure after Cataract Surgery in Yaounde
G. Kagmeni1,2 , C. Nanfack Ngoune*1,3, A.F. Nomo1,3, G. Nsangou1, D. Sina1, MG Nguepi1, CD Noche4
1Department of Ophthalmology, Faculty of medicine and biomedical sciences, University of Yaounde I
2University teaching hospital of Yaounde, Yaounde, Cameroon
3Ophthalmology unit, Gyneco-obstetric and pediatric hospital of Yaounde, Yaounde, Cameroon
4Higher Institute of Health Sciences, Université des Montagnes, Bangangte, Cameroon
*Corresponding Author: Chantal Nanfack Ngoune, Department of Ophthalmology, Faculty of medicine and biomedical sciences, University of Yaounde, Yaounde, Cameroon; Email: cngoune2001@yahoo.fr
Received date: 07 May, 2022, Manuscript No. IOPJ-22-65499;
Editor assigned date: 09 May, 2022, Pre QC No. IOPJ-22-65499 (PQ);
Reviewed date: 23 May, 2022, QC No IOPJ-22-65499;
Revised date: 28 May, 2022, Manuscript No. IOPJ-22-65499 (R);
Published date: 07 June, 2022, DOI: 10.4172/2324-8599.11.5.21
Citation: Kagmeni G, Ngoune CN, Nomo AF, Nsangou G, Sina D, Nguepi MG, Noche CD (2022) Changes in Intraocular Pressure after Cataract Surgery in Yaounde. Int J Ophthalmic Pathol 11:5.
Abstract
Introduction:Changes in Intraocular Pressure (IOP) have been reported following cataract surgery. This study sought to examine changes in IOP following Manual Small-Incision Cataract Surgery (MSICS) in a Cameroonian population.
Methods:In this prospective non-comparative case series, the IOP values of all consecutive patients who underwent MSICS at the University Teaching Hospital were recorded preoperatively and at day 3, day 14 and day 60 postoperatively.
Results: This study included 53 patients who underwent MSICS. The patients had a mean age of 59.9 years (range: 7– 85 years). The preoperative mean IOP was 18.6 ± 4.3 mm Hg (range: 10.2–33.4 mm Hg). An IOP greater than 20 mm Hg was observed in 18.34% of the patients before surgery. The mean amount of cohesive viscoelastic substance used for implantation was 0.6 ml (range: 0.5–0.8 ml). An artificial lens was implanted in the posterior chamber in 94.3% of patients and the sulcus in 5.7% of patients. The IOP decreased gradually and significantly from 18.6 ± 4.3 preoperatively to 15.9 ± 3.6 mm Hg at day 3 (P=0.002) and 13.0 ± 2.2 mm Hg at day 60 (P=0.001) postoperatively.
Conclusion:Uncomplicated cataract surgery led to a significant decrease in IOP in most patients. Cataract surgery should be considered first in cases of glaucoma-cataract association.
Keywords: Intraocular pressure; Manual small-incision cataract surgery
Introduction
A cataract is an opacification of the crystalline lens that results in a decrease in visual acuity. Age-related cataract is the leading cause of blindness in the world, and accounts for 48% of avoidable blindness [1,2]. Cataract surgery is the most commonly performed operative procedure worldwide. The main goal of cataract surgery is to replace the clouded lens with an implant to restore vision and improve the patient’s quality of life. Many studies have described changes in Intraocular Pressure (IOP) (both increases and decreases from the normal IOP level) following cataract surgery [2,3]. Coh et al. [4] reported a significant decrease in IOP, ranging from 14.2% to 21%, after a one-month follow-up period. Coh et al. also found that after cataract removal, the number of hypotonising drugs was reduced in glaucoma patients. Previous studies have reported a decrease in IOP following phacoemulsification [5,6]. The present study sought to examine IOP variations following cataract surgery in a Cameroonian population.
Methods
In this prospective study, we included all consecutive patients aged 40 years and above who underwent cataract surgery at the CHU of Yaoundé. The study was conducted in full compliance with the Helsinki declaration. The institutional Ethical review board of the faculty of medicine and biomedical sciences (FMSB) of the University of Yaounde i approved the study (Number 313/UYI/FMSB/RDRC/ DAASB/CSD). A written informed consent was obtained from each patient or their legal guardian. Before surgery, all patients underwent a comprehensive ophthalmological examination to determine their visual acuity and IOP (using a Topcon non-contact tonometer) and a slit-lamp fundoscopy. The peribulbar anaesthesia was a mixture of 2% xylocaine in adrenaline (2.5 ml) and bupivacaine (2.5 ml). A fornixbased conjunctival flap was made from 10 to 12 o’clock. A 7.5 mm self-sealing sclero-corneal tunnel incision was made 1 mm into the clear cornea and 1.5–2.0 mm behind the limbus. A continuous curvilinear capsulorhexis was completed. A posterior-chamber Intraocular Lens (IOL) implant was placed in the capsular bag under a cohesive viscoelastic material. After the IOL implant, at least 10cc of BSS was exchanged with the Simcoe cannula for the aspiration of viscoelastic substance out of the anterior chamber. At the end of the procedure, an antibiotic-corticosteroid mixture was injected subconjunctivally. Postoperative care comprised the topical application of a steroidal of anti-inflammatory and antibiotic medication for 6 to 8 weeks. The analysed parameters included the adjusted IOP, the anterior chamber depth, the type of anaesthesia, the type of surgery, the viscous volume used for the implantation, the implantation site (e.g., sac, sulcus and CA), the volume of solute exchanged for washing after the implantation, the type of corticosteroid used in the sub-conjunctival injection, the duration of the procedure and the adjusted IOP during the postoperative period at day 3, day 14, and day 60.
Statistical analysis
The data obtained were analyzed using SPSS software (version 1.6). The preoperative IOP and the postoperative IOP at various time points after surgery are reported as the mean and standard deviation. The IOP changes were compared using an analysis of variance. A p value <0.05 was considered statistically significant.
Results
This study comprised 53 patients who had been operated on and followed up with at the University Teaching Hospital, Yaounde. The patients had a mean age of 59.9 years (range: 7–85 years), and 56.6% of the patients were female. The mean anterior chamber depth was 3.23 ± 0.6 mm (range: 2.11–4.62 mm). Details of the IOP variations are summarized in Table 1.
| Pre operative IOP | Day 3 post operative IOP | Day 14 post operative IOP | Day 60 post operative IOP | |
|---|---|---|---|---|
| Mean | 18,6 ± 4,3 | 15,9 ± 3,6 | 14,2 ± 3,3 | 13,0 ± 2,2 |
| Range | 10,2-33,4 | 8,3-24 | 9,6-20 | Nov-18 |
| PIO (> 20 mmHg) (%) |
18.34% | 7,5 | 9 | 7,5 |
| Difference between baseline and post- operative IOP | 2,7 ± 0,7 | 4.4 ± 0,13 | 5,6 ± 2,2 | |
| Compariso n baseline and post- operative IOP |
P=0,002 | P=0,001 |
Table1: Comparison between preoperative IOP and IOP at D3, D14, D60 after surgery
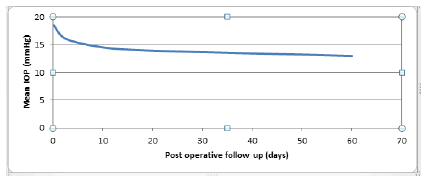
The preoperative mean IOP was 18.6 ± 4.3 mm Hg (range: 10.2– 33.4 mm Hg). An IOP greater than 20 mm Hg was observed in 18.34% of the patients before surgery. All patients underwent manual small-incision cataract surgery (MSICS). The mean amount of a cohesive viscoelastic substance used for the implantation was 0.6 ml (range: 0.5–0.8 ml). An artificial lens was implanted in the posterior chamber in 94.3% of patients and in the sulcus in 5.7% of patients. After implantation, the average volume of BSS used to wash out the viscoelastic material was 10 ml (range: 5–18 ml). The average duration of the procedure was 14 minutes (range: 7–32 minutes). Data’s on IOP variation are summarized in table1. IOP decreased gradually and significantly from 18.6 ± 4.3 mm Hg preoperatively to 15.9 ± 3.6 mm Hg at day 3 (P=0.002) and 13.0 ± 2.2 mm Hg at day 60 (P = 0.001) postoperatively (Figure 1).
Discussion
The patients in our study had a mean age of 59 ± 18.9 years (range: 7–85 years), which explains the predominance of senile cataracts. This type of cataract is thought to result from a change in the chemical composition of the crystalline fibres by a normal aging process or the strengthening and clouding of the lens secondary to other mechanisms [7].
The mean preoperative adjusted IOP in our study was 18.6 ± 4.3 mm Hg. This figure was higher than that reported by Oluwatoyin et al. of 13,5 mm Hg in Nigeria in 2020 [8]. This may be explained by the difference between the two methodologies adopted by the studies. Notably, Oluwatoyin et al. excluded patients presenting with ocular hypertension, glaucoma, pseudo-exfoliation, pre-existing trauma, complicated cataracts and surgical complications, such as posterior capsule rupture, vitreous loss and hyphema, from their study.
In this study, patients had a mean anterior chamber depth of 3.03 ± 0.6 mm. In an Ivory Coast study, Fanny et al. [9] reported a mean anterior chamber depth of 2.98 ± 0.53 mm. Lens opacification is accompanied by a change in its density and an increase in its thickness, which places pressure on the posterior surface of the iris and leads to a decrease in the depth of the anterior chamber. SICS was the most common surgical technique used, as it is a standard technique in the poor countries of Africa and Asia [3,10,11] This technique may be selected because of the type of cataract presented by patients or because it is comparable in the long term to phacoemulsificassion [12]; however, due to its high costs, it was only performed in 11% of our patients. Sabyasachi et al. found that the decrease in IOP was significant and comparable 6 months after cataract surgery using either of the techniques and that both surgeries produced similar changes in anterior chamber and angle parameters [13]. In the present study, the IOL implant was mainly placed in the posterior chamber (in 94.3% of cases), which is the ideal site for implantation during cataract surgery, as it provides stability for the implant [14].
A posterior capsule tear was the most common operative complication in our study. This complication was the reason for three implantations in the sulcus in our series. A posterior capsule tear is an important risk factor for postoperative hypertonia [15]. A significant decrease in the mean IOP was noted in the early postoperative period (P=0.002); however, 7.5% of the patients had an IOP greater than 20 mm Hg. This increase in IOP persisted on day 3 postoperatively and may be explained by several factors, including early postoperative inflammation, retained viscoelastic substance and the use of topical medication (e.g., antibiotics, mydriatics and steroids).
The use of a dispersive viscoelastic substance has been incriminating in the genesis of increase in IOP in some studies [16]. Some authors have reported an increase in the mean IOP from the baseline value, while others have described a significant increase in IOP in the early post-phacoemulsification period [17]. However, these authors concluded that both phacoemulsification and MSICS led to significant and similar IOP reductions 6 months after surgery.
In the late postoperative period, a decrease in mean IOP of about 5.6 mm Hg compared to the mean preoperative IOP was noted. It is thought that this decrease in IOP is secondary to structural modifications of the anterior chamber; that is, a deepening of the anterior chamber and a widening of the iridocorneal angle. This would allow an opening of the trabecular meshwork and lead to an increase in the flow of aqueous humour [18]. Similarly, changes in the anterior chamber and angle parameters have been found in both phacoemulsification and SICS [17]. In the present study, we did not find a statistically significant correlation between the operative parameters (i.e., the amount of viscoelastic substance used for implantation, the volume of BSS used to wash out the viscoelastic substance and the duration of the procedure) and the decrease in IOP observed after cataract surgery.
Conclusion
Based on the findings of this study and many others, cataract surgery appears to modify the parameters of the anterior chamber, which results in a sustainable decrease in IOP. Cataract surgery should be considered first in cases of glaucoma-cataract association.
References
- He M, Wang W, Huang W (2017) Variations and Trends in Health Burden of Visual Impairment Due to Cataract: A Global Invest Ophthalmol Vis Sci 58: 4299-4306.
- Li T, He T, Tan X, Yang S, Li J et al. (2009) Prevalence of age- related cataract in high-selenium areas of China. Biol Trace Elem Res 128: 1-7.
- Grinbaum A, Blumenthal M, Assia E (2003) Comparison of intraocular pressure profiles during cataract surgery by phacoemulsification and extracapsular cataract extraction. Ophthalmic Surg Lasers Imaging 34: 182-6.
- Coh P, Moghimi S, Chen RI, Hsu CH, Masís Solano M et al. (2016) Lens Position Parameters as Predictors of Intraocular Pressure Reduction After Cataract Surgery in Glaucomatous Versus Nonglaucomatous Eyes. Invest Ophthalmol Vis Sci 57: 2593-9.
- Athanasiov PA, Edussuriya K, Senaratne T, Sennanayake S, Sullivan T et al. (2010) Cataract in central Sri Lanka: prevalence and risk factors from the Kandy Eye Ophthalmic Epidemiol 17: 34-40.
- Cheng CY, Liu JH, Chen SJ, Lee FL (2000) Population-based study on prevalence and risk factors of age-related cataracts in Peitou, Taiwan. Zhonghua Yi Xue Za Zhi (Taipei) 63: 641-648.
- Rigal-Sastourné JC, Delbarre M (2012) Semiologie et formes cliniques de la cataracte chez l’adulte. EMC Ophtalmologie 9: 1-10.
- Onakpoya OH, Adeoye AO, Adegbehingbe BO, Badmus SA, Adewara BA et al. (2020) Intraocular pressure variation after conventional extracapsular cataract extraction, manual small incision cataract surgery and phacoemulsification in anindigenous black population. Pan Afr Med J 36: 119.
- Fanny A, Ouattara A, Aka J, Coulibaly F, Gbé K et al. (2007) Valeurs biometriques de l'oeil du sujet africain de race noire et hypothèse du role dans certaines pathologies: A propos de 325 J Fr Ophtalmol 30: 68-72.
- Djiguimde PW, Diomande IA, Ahnoux-Zabsonre A, Koffi KV, Meda TA et al. (2015) Résultats de la chirurgie avancee de la cataracte par tunnelisation: A propos de 262 cas réalisés au CHR de Banfora (Burkina Faso). Pan Afr Med J 22:
- Nganga Ngabou CGF, Makita C, Ndalla SS, Nkokolo F, Madzou M (2017) Baisse de la pression intraoculaire après chirurgie manuelle de la cataracte par petite incision Intraocular pressure decrease after manual small incision cataract surgery]. J Fr Ophtalmol 40: 397-402.
- Yasutani H, Hayashi K, Hayashi H, Hayashi F (2004) Intraocular pressure rise after phacoemulsification surgery in glaucoma J Cataract Refract Surg 30: 1219-24.
- Shingleton BJ, Wadhwani RA, O'Donoghue MW, Baylus S, Hoey H (2001) Evaluation of intraocular pressure in the immediate period after phacoemulsification. J Cataract Refract Surg 27: 524-7.
- Kohnen T, Baumeister M, Kook D, Klaproth OK, Ohrloff C (2009) Cataract surgery with implantation of an artificial lens. Dtsch Arztebl Int 106: 695-702.
- Ionides A, Minassian D, Tuft S (2001) Visual outcome following posterior capsule rupture during cataract Br J Ophthalmol 85: 222-224.
- Rainer G, Menapace R, Findl O, Georgopoulos M, Kiss B et al. (2000) Intraocular pressure after small incision cataract surgery with Healon5 and Viscoat. J Cataract Refract Surg. 26: 271-276.
- Sengupta S, Venkatesh R, Krishnamurthy P, Nath M, Mashruwala A et al. (2016) Intraocular Pressure Reduction after phacoemulsification versus Manual small-incision cataract surgery: a randomized controlled trial. Ophthalmology 123: 1695-1703.
- Kim JW (1996) Comparative study of intraocular pressure change after cataract surgery: Phacoemulsification and extracapsular cataract extraction. Korean J Ophthalmo 10: 104-108.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi