Case Report, J Regen Med Vol: 8 Issue: 1
Chronic Superficial Achilles Bursitis Treated with Percutaneous Bursectomy and Platelet-Rich Plasma Injection: A Case Report
Colberg RE*, Umarvadia JS and Walsh KP
Andrews Sports Medicine & Orthopedic Center, Birmingham, AL, USA
*Corresponding Author : Ricardo E. Colberg
MD, American Sports Medicine Institute, Birmingham, AL, USA
Tel: (205) 918-0000
E-mail: ricardo.colberg@andrewssm.com
Received: November 20, 2018 Accepted: February 17, 2019 Published: February 25, 2019
Citation: Colberg RE, Umarvadia JS, Walsh KP (2019) Chronic Superficial Achilles Bursitis Treated with Percutaneous Bursectomy and Platelet-Rich Plasma Injection: A Case Report. J Regen Med 8:1. doi: 10.4172/2325-9620.1000148
Abstract
A 23-year old male presented with chronic right ankle pain intermittently over the past three years secondary to a chronic superficial Achilles bursitis. The patient had been seen by multiple physicians during this time and had tried various conservative treatment modalities, ranging from physical therapy and antiinflammatories to immobilization with a boot. He was then offered percutaneous bursectomy using a radiofrequency coblation wand under ultrasound guidance followed by a platelet-rich plasma injection. The patient, thereafter, was followed up for one year. At the eight week follow-up, the patient was very pleased to report full resolution of his symptoms. He returned to recreational sports without further reported pain and remained asymptomatic during follow-up at three months and one year after the procedure. This case highlights a novel procedure that has not been previously reported in the literature. It is minimally invasive, carries low risk for complication, requires minimal care on post-procedural follow-up, and does not restrict further surgical resolution if the procedure is unsuccessful.
Keywords: Chronic ankle pain; Bursitis; Achilles tendon; Haglund deformity; Platelet-rich plasma; Radiofrequency coblation; Ultrasonography
Introduction
The Achilles tendon is the largest tendon in the body, connecting the gastrocnemius and soleus muscles to the calcaneus. It contains both a retrocalcaneal bursa anterior to the tendon at its insertion and a larger, more superficial subcutaneous bursa posterior to the tendon. Although superficial Achilles bursitis is not related to a specific injury, it is typically due to repetitive stress over the tendon insertion onto the calcaneus. There are multiple causes for this, including sudden increase in exercise regimen, tight gastrocnemius muscles, and calcaneal bone spurs. Furthermore, it can be seen in middle-aged active individuals who play recreational sports or who have suddenly increased their intensity or duration of training. Treatments consist of physical therapy, strengthening exercises, anti-inflammatory medications, orthotics, heel lifts, and activity modification.
Case Summary
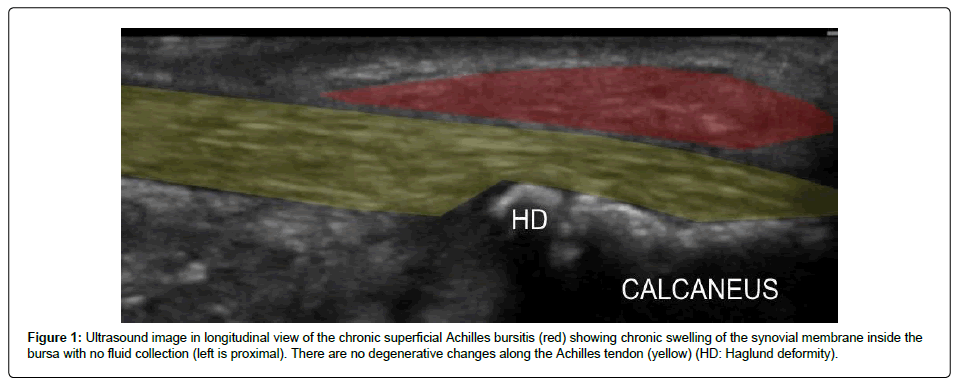
A 23-year old active male presented with complaints of chronic right ankle pain over a period of three years localized over the posterior aspect of the ankle and hindfoot. The patient described pain, swelling, and severe tenderness over the posterior calcaneus that had worsened over the last few months. He reported that the pain was exacerbated by playing recreational sports as well as wearing tight shoes. He denied any recent or acute injuries, although he admitted to recently spending more time studying in college and participating in sports sporadically. The patient described the pain on initial presentation as mild to moderate, and at times, severe, sharp and stabbing. Over the last few weeks, the pain had worsened with walking as well as going up and downstairs. The patient had seen multiple physicians for this pain that had previously been diagnosed with Achilles tendinitis. He had completed multiple months of physical therapy, oral anti-inflammatory medications, and using a boot and shoe insert with heel lift without much relief. Upon examination, the patient had severe tenderness to palpation throughout the whole superficial Achilles bursa, from medial to lateral and from proximal to distal. Under ultrasound imaging, his superficial Achilles bursa was noted to be chronically inflamed and there was no pathology in the actual tendon. The patient did have a Haglund deformity (Figure 1).
Figure 1: Ultrasound image in longitudinal view of the chronic superficial Achilles bursitis (red) showing chronic swelling of the synovial membrane inside the bursa with no fluid collection (left is proximal). There are no degenerative changes along the Achilles tendon (yellow) (HD: Haglund deformity).
Given the chronicity of his symptoms and failure of conservative measures, the patient was offered a surgical consult for an open bursectomy and Haglund resection; however, the patient indicated that he was not interested in surgery at this time due to concern of wound healing complications and wanted to exhaust minimally invasive options. The patient was educated on the possibility of injecting platelet-rich plasma (PRP) into the bursa to stimulate tissue healing versus performing percutaneous bursectomy using the Topaz EZ Microdebrider coblation wand (Smith & Nephew, London, UK) in order to remove the chronic degenerative tissue, versus combining the two treatment options. The patient was further educated on the fact that these treatments are novel and therefore considered experimental due to lack of undisputable evidence in the literature about their benefits. He was also educated on the risks associated with these treatment options, including bleeding, infection, tendon rupture, and the possibility of post-injection inflammatory reaction. The patient chose to proceed forward with an ultrasound guided right superficial Achilles percutaneous bursectomy and PRP injection into the bursa.
After written informed consent was obtained, 25 mL of whole blood was drawn from the antecubital fossa, mixed with 5 mL Acid Citrate Dextrose-A (ACD-A) and centrifuged (single spin) using the EmCyte System (EmCyte Corporation, Fort Myers, FL) to form 3 mL leukocyte rich PRP (no activator used). This was obtained by manually aspirating the buffy coat layer, following the manufacturer’s guidelines.
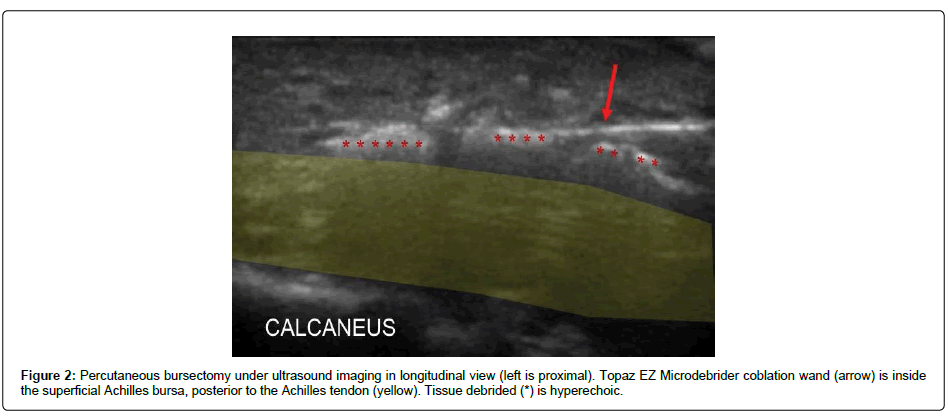
The patient’s skin and soft tissue surrounding the posterior aspect of the right ankle and hindfoot was prepped and cleansed in a sterile fashion with Betadine solution and isopropyl alcohol. Live ultrasound imaging using a portable sonographic imaging device was used with sterile ultrasound gel to avoid any surrounding neurovascular structures (Sonosite M-Turbo with HFL50X linear transducer, 15-6MHz by FUJIFILM SonoSite Inc., Washington, USA). A total of 2.5 ml of lidocaine 1% and 2.5 ml of Marcaine 0.25% were injected into the surrounding soft tissue for local anesthesia. An 18-guage 1 ½ inch needle was used to puncture the skin. Then, the coblation wand was advanced in plane with the ultrasound probe in a sagittal view towards the superficial Achilles bursa. A percutaneous superficial Achilles bursectomy was then completed over the posterior aspect of the tendon by activating the instrument approximately twenty times throughout the whole bursa, covering from proximal to distal, medial to lateral, and superficial to deep aspect of the bursa (Figure 2).
The patient then received the leukocyte-rich PRP injection into the treated site. Under live ultrasound imaging; a 22 gauge 1 ½ inch needle was used to inject a total of 3 ml of plasma concentrate into the soft tissue around the Achilles tendon and superficial Achilles bursa. At no time was the actual Achilles tendon neither punctured with the needles or instrument nor was it injected with PRP, confirmed with live ultrasound imaging. The medication was seen entering the correct tissue space. Hemostasis was achieved and the patient tolerated the procedure well with no complications noted.
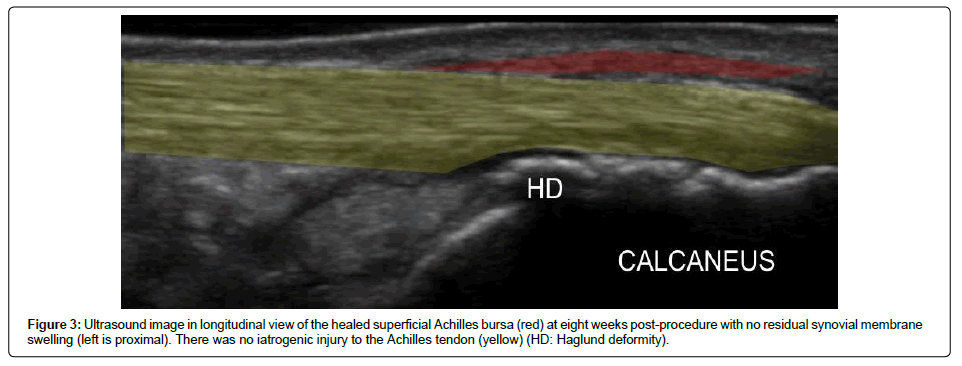
The patient was fitted with crutches and a walking boot in order to immobilize the ankle following completion of the procedure and was instructed to wear the boot at all times for the first week. After a week, he completed a 7 day boot wean protocol. A post-PRP physical therapy program was given to the patient and begun two weeks after the procedure. The patient was instructed not to take any anti-inflammatory medications for two weeks to avoid counteracting the effect of the PRP injection. At his four week follow-up, the patient reported mild intermittent pain with walking, but significantly improved pain at rest and when sitting down. At eight weeks post-procedure, his foot pain had completely resolved with the patient stating that it was “100% better.” Ultrasound imaging showed a healed superficial Achilles bursa (Figure 3). Overall, the patient’s visual analog scale (VAS) improved from 6/10 before the procedure, to 2/10 at both 4 and 8 weeks, and ultimately 0/10 at the 7 month mark with no residual tenderness to palpation over the superficial Achilles bursa. The patient was very satisfied with his interval improvement after three years of ankle pain.
Discussion
In this case, a 23-year old active male presented with a three year history of chronic superficial Achilles bursitis. This young patient had significant pain with simple ambulation that affected his activities of daily living. Conservative treatment is preferred and in many cases, surgery is not necessary. Non-operative measures include physical therapy, strengthening exercises, iontophoresis with dexamethasone, extracorporeal shock-wave therapy, and in some cases, localized steroid injection into the bursas. Eccentric training is the first line therapy for mid-portion Achilles tendinopathy. However, in randomized controlled trials that have been well cited, not all patients were pain-free following therapy with eccentric exercises [1]. No studies have looked specifically at eccentric exercises for superficial Achilles bursitis.
After continuing to report no pain reduction following six months of therapy, many of these patients received surgical consults. An open superficial Achilles bursectomy is indicated after six months of nonoperative treatment, but it carries a risk of wound complications. In fact, a pubmed serach for keywords “superficial achilles bursa”, “superficial achilles bursitis”, “retroachilles bursa” and “retroachilles bursitis” revealed no prior study describing the open surgical option for this condition. The studies that the pubmed search revealed were all on Achilles tendinopathy. Studies have shown that in patients with Achilles tendinitis treated surgically, non-athletic patients took longer and had more complications than athletic patients [2].
This is the first case report describing a procedure to treat chronic superficial Achilles bursitis. Based on this case report, a minimally invasive debridement of the bursa over the Achilles tendon using the Topaz Microdebrider may be considered for cases of recalcitrant superficial Achilles bursitis. The Topaz Microdebrider instrument creates a low energy plasma field at the tip of the instrument that coablates the surrounding soft tissue. In a study on coblation of chronic lateral epicondylitis, significant reduction in pain started 7-10 days after the procedure and lasted for 2 years, the entire duration of follow-up in the study [3].
Microtenotomy using radiofrequency has been used for chronic tendinopathies for years with promising results. It stimulates angiogenesis in the fibrotic and avascular tissue, which promotes secretion of fibroblastic growth factor, vascular endothelial growth factor, as well as vascular cells. Tendons that have been treated via radiofrequency microtenotomy show an early, controlled inflammatory response. There is evidence of extensive proliferation of vascular cells and new blood vessel formation at approximately 28 days [4]. The advantage of using co-ablation is that the low energy field treats only the tissue immediately adjacent to the instrument tip and it does not injure tissue more than 3 mm away.
A study looking at patients who had chronic isolated Achilles tendinopathy refractory to non-operative treatment rated their clinical outcome after radiofrequency microtenotomy as “good or excellent” with an average of 2.5 years follow-up [5]. Several case series have reported promising outcomes in recalcitrant plantar fasciitis treated with this instrument [6]. No study to date has been published on radiofrequency coblation technology used for performing percutaneous superficial Achilles bursectomy.
Meta-analysis of platelet injections for tendon-related pathology has also shown enhanced outcomes in contrast to placebo and other treatment approaches [7,8]. PRP is an autologous blood preparation with concentrations of platelets above baseline values. Similar to microtenotomy, this treatment modality contributes to injury healing by releasing growth factors and cytokines that modulate neovascularization in addition to promoting mitogenesis, boosting local collagen production and reorganization, and providing an anti-inflammatory effect [9]. Therefore, it remains uncertain if the patient’s successful outcome was a result of the procedure using the Topaz Microdebrider alone, the PRP alone, or the combination of the two treatments.
Conclusion
This case study presents a novel approach to treating superficial Achilles bursitis non-operatively. The combination of a percutaneous bursectomy followed by a PRP injection via ultrasound guidance yielded positive results of pain reduction and tendon healing visualized on ultrasound in this case study. It is unknown if the patient would have obtained similar outcomes if each of these procedures would have been performed individually or if it was a synergistic effect from combining the use of the Topaz Microdebrider to remove the degenerative tissue followed by the injection of PRP to stimulate appropriate tissue healing. Further studies are needed to determine the role of minimally invasive procedures such as the two described in this case report in the treatment of chronic superficial Achilles bursitis.
References
- Magnussen RA, Dunn WR, Thomson AB (2009) Nonoperative treatment of midportion Achilles tendinopathy: a systematic review. Clin J Sport Med 19: 54-64.
- Maffulli N, Testa V, Capasso G, Oliva F, Sulio A, et al. (2006) Surgery for chronic Achilles tendinopathy yields worse results in nonathletic patients. Clin J Sport Med 16: 123-128.
- Tasto JP, Cummings J, Medlock V, Hardesty R, Amiel D (2005) Microtenotomy using a radiofrequency probe to treat lateral epicondylitis. Arthroscopy 21: 851-860.
- Gerdesmeyer L, Frey C, Vester J, Maier M, Weil Jr L, et al. (2008) Radial extracorporeal shock wave therapy is safe and effective in the treatment of chronic recalcitrant plantar fasciitis: results of a confirmatory randomized placebo-controlled multicenter study. Am J Sports Med 36: 2100-2109.
- Sarimo J, Orava S (2011) Fascial incision and adhesiolysis combined with radiofrequency microtenotomy in treatment of chronic midportion Achilles tendinopathy. Scand J Surg 100: 125-128.
- Sean NY, Singh I, Wai CK (2010) Radiofrequency microtenotomy for the treatment of plantar fasciitis shows good early results. Foot Ankle Surg 16: 174-177.
- Fitzpatrick J, Bulsara M, Zheng MH (2017) Effectiveness of platelet-rich plasma in the treatment of tendinopathy: a meta-analysis of randomized controlled clinical trials. Am J Sports Med 45: 226-233.
- Filardo G, Di Matteo B, Kon E, Merli G, Marcacci M (2018) Platelet-rich plasma in tendon-related disorders: results and indications. Knee Surg Sports Traumatol Arthrosc 26: 1984-1999.
- Monto RR (2012) Platelet rich plasma treatment for chronic Achilles tendinosis. Foot Ankle Int 33: 379-385.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi