Research Article, J Liver Disease Transplant Vol: 7 Issue: 2
Clinical Profile of Autoimmune Hepatitis Among Filipino patients
Ira I Inductivo-Yu1* and Emily Mae L Yap2
1Head, Section of Gastroenterology; Department of Internal Medicine; National Kidney and Transplant Institute; Philippines
2Department of Internal Medicine; National Kidney and Transplant Institute; Philippines
*Corresponding Author : Ira I Inductivo-Yu
Department of Internal Medicine, National Kidney and Transplant Institute; Room 3233, Diliman, Quezon City, Philippines
E-mail: irainductivo@gmail.com
Received: September 03, 2018 Accepted: October 10, 2018 Published: October 17, 2018
Citation: Inductivo Yu II, L Yap EM (2018) Clinical Profile of Autoimmune Hepatitis among Filipino patients. J Liver Disease Transplant 7:2. doi: 10.4172/2325-9612.1000165
Abstract
Significance: Autoimmune Hepatitis (AIH) has not been extensively described among Filipinos. This study was undertaken to determine the prevalence rate, demographic, clinical and laboratory findings of Filipinos diagnosed with AIH .
Methodology: This is a retrospective prevalence study of patients diagnosed with AIH from January 1, 2004 to December 31, 2014.
Results: The prevalence rate of AIH among those with liver diseases was 0.62% CI 95% [0.4%-0.95%] (20 cases/3,243). The average age was 38.55 years old + 17.62 with a female:male ratio of 1.85:1. The most common initial clinical presentation were jaundice (55%) and asymptomatic transaminitis (25%). The autoimmune markers were ASMA (80%), ANA (20%), Anti-LKM1 (20%), and Anti-mitochondrial antibody (AMA) (5%). Prednisone as monotherapy was given in 11 cases (55%). There was a decrease in mean pre- and post-treatment levels in the liver biochemistries: ALP from 144.33[87.72] to 102.85[28.86] IU/L, ALT from 192.32[311.97] to 97.12[121.4] IU/L, AST from 201.1[365.67] to 107.35[239.41] IU/L, total bilirubin levels from 11.77[14.37] to 5.2[7.67] mg/dL, and serum globulin levels from 3.75[0.64] to 3.36[0.62]. Seventeen patients (85%) were reported to be alive with good follow up.
Conclusion: AIH is rare among Filipinos. Jaundice was the most common initial presenting manifestation. Only a reduction in total bilirubin showed clinical significance. A majority were given Prednisone with good response.
Keywords: Autoimmune Hepatitis; Clinical profile; Filipinos; Prevalence
Introduction
Background
Autoimmune Hepatitis (AIH) is a chronic disease of unknown cause that is characterized by continuing hepatocellular inflammation and necrosis with a tendency to progress to cirrhosis. Because of its rarity, epidemiological studies are largely limited. The disease has female preponderance and a bimodal distribution has been described, with a first peak of incidence at 10 to 20 years and a second peak at 45 to 70 years [1].
AIH is rare. Among white adults, the prevalence is estimated to be 0.1 to 1.2 cases per 100,000 individuals [1]. The incidence of type 1 AIH in Europe and North America ranges from 0.1 to 1.9 per 100,000 cases/year. The relative proportion of AIH among cases with chronic hepatitis is low in regions with a high prevalence of viral hepatitis. Among the types of AIH, Type 2 is more frequent in southern Europe than in northern Europe, the United States, and Japan [2].
Type 1 AIH, the most common type worldwide, is the classic syndrome occurring in young women, associated with marked hyperglobulinemia, lupoid features, circulating anti-nuclear antibodies (ANA) and/or anti-smooth muscle antibodies (ASMA), Human Leukocyte Antigen (HLA)-DR3 or HLA-DR4, autoantibodies against actin and atypical perinuclear antineutrophilic cytoplasmic antibodies (pANCA). Conversely, Type II AIH is often seen in children, more common in Mediterranean populations, linked to HLA-DRB1 and HLA-DQB1 haplotypes. The latter is associated with anti-Liver Kidney Microsomal (LKM) antibodies, but not ANA [3]. Type 3 AIH is the least common type which is characterised by the presence of soluble liver antigen/liver-pancreas (SLA/LP) in serum [4].
Diagnosis requires determination of serum aminotransferases and gamma globulin levels; detection of ANA and/or SMA, or in their absence, anti-LKM1; and liver tissue examination. A diagnostic criteria has been recommended by the International Autoimmune Hepatitis Group (IAHG) which takes into account presence or absence of the following - genetic liver disease, active viral infection, toxic or alcohol injury, characteristic laboratory features, presence of autoantibodies and typical histologic findings. For patients suspected to have atypical autoimmune hepatitis, a diagnostic scoring system has been recommended by the same international group. With corticosteroid therapy, patients with AIH enter remission and frequently relapse after drug withdrawal. A definite diagnosis of AIH would constitute either a pre-treatment score of >15 and/or a post-treatment score of >17. A pre-treatment score of 10-15 and/or a post-treatment score of 12-17 would constitute a probable diagnosis of AIH. A sensitivity ranging from 97 to 100% and its specificity for excluding AIH in patients with chronic hepatitis C ranges from 66% to 92% has been described in the AASLD guidelines for AIH [5].
This criteria, however, is less applicable in routine clinical practice due to its complexity. Nonetheless, early diagnosis is important because immunosuppression is life-saving. A simplified diagnostic criteria was published by Hennes et al. for this purpose with the following variables - sex, age, autoantibodies, immunoglobulins, absence of viral hepatitis, and histology. The diagnosis of probable AIH would require a score > 6 points with 88% sensitivity and 97% specificity while definite AIH would necessitate a score of > 7 with 81% sensitivity and 99% specificity in the validation set [5].
Review of related literature
AIH is a chronic liver disease of unknown etiology. It affects any age, both sexes and all ethnic groups [6]. In a nationwide study done in Sweden, the overall incidence was 0.85/100,000 inhabitants and year, and the prevalence was 11/100,000 inhabitants [7]. In Alaska and New Zealand, prevalence rates of 42.9 cases per 100000 and 24.5 cases per 100000 inhabitants respectively have been described [8-9].
Studies among Southeast Asians are limited but are comparable to studies done among Caucasians. Jalihal et al. described 19 Bruneians seen in a hepatology clinic. The prevalence rate of the disease was 5.61/100,000 and was higher in the Chinese than in Malays and Indigenous people. The median age at diagnosis was 52 years (range 33-70) with a female to male ratio of 3.75:1 [10].
In a study in India, female predominance was described with a mean age of 36.2 was observed with type 1 as the most common type and advanced liver disease (chronic hepatitis and cirrhosis) being the most common clinical presentation. Most of these patients were ANA or SMA positive [11].
Clinical manifestations vary from asymptomatic to severe hepatitis according to race and ethnicity [6]. Commonly seen presentations described among the Bruneian population were abnormal liver function (52.6%), icteric hepatitis (36.8%), and decompensated liver disease (10.5%). Histologically advanced fibrosis was found in 47.4% and cirrhosis in 21.1% of the patients. During their follow-up period of 31 months (range 0.25-102), 3 patients died, 2 had progressive liver failure and 1 had lymphoma. Complete biochemical response was seen in 75% of the patients, partial response in 12.5%, and no response in 12.5% [10]. In one study, Hispanics were described to have the highest prevalence of cirrhosis while Asians were reported to have poorer survival outcomes [12]. Alaskan natives were observed to have a high frequency of acute icteric disease at the disease onset [8].
In a study in Pakistan, clinical presentation was variable, ranging from an asymptomatic clinical course to severe acute illness. Race was described to be a factor on its variability. Patients from Pakistan had high prevalence of advanced cirrhosis at time of presentation. Patients from Middle East and Japan had a cholestatic pattern on the liver function tests [13].
AIH remains a major diagnostic challenge worldwide. It should be considered in every case of acute or chronic hepatitis in the absence of viral, metabolic, genetic and toxic etiologies. Polyclonal hypergammaglobulinemia is characteristic in most cases, while histology and detection of autoantibodies are still the hallmark for timely diagnosis [6].
In hepatology, the term overlap syndrome describes variant forms of the major hepatobiliary autoimmune diseases, AIH, primary biliary cirrhosis (PBC), and primary sclerosing cholangitis (PSC). These patients present with both hepatitic and cholestatic biochemical and histological features of AIH, PBC, and/or PSC, and usually show a progressive course toward liver cirrhosis and liver failure without adequate treatment. AIH-PBC overlap syndromes have been reported in almost 10% of adults with AIH or PBC, whereas AIH-PSC overlap syndromes were found in 6 to 8% of children, adolescents, and young adults with AIH or PSC [14].
Potts and Verna published an article which described the prevalence of liver failure on five retrospective studies with a total population of 85 patients. This varied from 8.7% to 19.8%. The majority (>75%) were women in the third to the sixth decade with type 1 AIH. Almost all patients had either encephalopathy at admission and/or had significant coagulopathy. The outcome of these studies showed variable remission rates with immunosuppression from 8.3 to 50% [15]. The variability highlights the paucity of studies available, strengthening the need to generate more studies.
Significance of the study
AIH has not been extensively described in the Philippines. To date, there are no studies of this rare disease among Filipinos, despite the increasing number of patients with liver diseases coupled with the availability and accessibility of sophisticated diagnostic tests. This study is the first one to describe the clinical profile of Filipino AIH patients. This study is also aimed to increase awareness of this type of hepatitis and to prompt physicians to do further work-up among hepatitis cases with negative viral serologic results and with no readily identifiable etiologies.
Objectives
General objective
To determine the prevalence rate, demographic, clinical, and laboratory findings of Filipino patients with autoimmune hepatitis seen at the National Kidney and Transplant Institute from 2004 to 2014
Specific objectivess
To describe the demographic profile of patients with autoimmune hepatitis
To describe the initial clinical presentation of these patients during their first admission or consult
To describe the baseline laboratory findings of these patients
To describe the treatment modalities administered
To describe patient outcomes and treatment response
Methodology
Study design
This is a retrospective prevalence study.
Study setting
National Kidney and Transplant Institute, a tertiary referral center, located at East Avenue, Quezon City, Philippines.
Study population
Inclusion criteria: All new and old AIH patients at NKTI who were seen and referred to the Section of Gastroenterology, Department of Internal Medicine from January 1, 2004 to December 31, 2014 were included in this study.
Sampling procedure: Retrospective review of records of patients seen at NKTI who were diagnosed with autoimmune hepatitis from 2004 –2014. Purposive sampling was employed in this study.
Data collection procedure: Both in and out-patient charts were reviewed. Charts of admitted patients were viewed using the Document Viewer at the Medical Records section after approval was secured from the Research Ethics Committee. The actual out-patient charts were reviewed at the respective clinics of the physicians with patients with the disease. Confidentiality of patient information was upheld in accordance to the Declaration of Helsinki. Data were encoded in a password-protected Microsoft Excel spreadsheet. A code number was assigned to each patient to maintain anonymity. Only the primary investigator had access to the file.
Operational Definitions
Autoimmune hepatitis: A chronic disorder characterized by continuing hepatocellular necrosis and inflammation, usually with fibrosis, which can progress to cirrhosis and liver failure [8].
Liver diseases: Include the following: acute and chronic hepatitis regardless of etiology, alcoholic liver disease, liver cirrhosis regardless of etiology, liver failure regardless of etiology, hepatocellular cancer, non-alcoholic fatty liver disease, non-alcoholic steatohepatitis and genetic, metabolic and infiltrative diseases affecting the liver.
Cirrhosis: Defined histologically as a diffuse hepatic process characterized by fibrosis and the conversion of normal liver architecture into structurally abnormal nodules. The progression of liver injury to cirrhosis may occur over weeks to years [9].
Hepatitis B virus infection: Defined as HBsAg seropositivity or HBV-DNA detectable by PCR with or without liver parenchymal disease on ultrasonography.
Hepatitis C virus infection: Defined as presence of a reactive antibody to Hepatitis C virus (anti-HCV and detectable HCV-RNA on PCR.
Significant alcohol consumption: Daily intake of more than 60 g of alcohol in men and 20 g in women significantly increases the risk of cirrhosis [10].
Statistical Analysis
Data were encoded in Microsoft Excel 2013 Spreadsheet. The prevalence rate of autoimmune hepatitis with CI at 95% was computed. Descriptive statistics were used to measure central tendency (e.g. mean) and spread (e.g. SD) to describe the data in the clinical profile. Moreover, categorical data profiles were expressed using frequency and percentage distribution. In testing laboratory tests average values’ changes from baseline to post-treatment, Paired t-test was used. IBM SPSS version 21 was the statistical software used.
Results
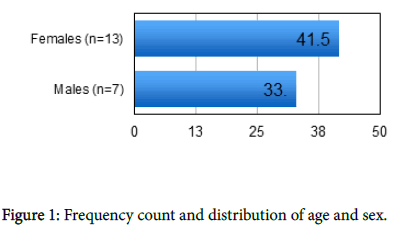
The prevalence rate of Autoimmune Hepatitis (AIH) seen among those with liver diseases at the National Kidney and Transplant Institute was 0.62% CI 95% [0.4%-0.95%] (20 cases / 3,243) from January 1, 2004 to December 31, 2014 . There were a total of 20 patients included in this study. The average age was 38.55 years old +/- 17.62. Thirteen (65%) were females with a female to male ratio of 1.85:1 (Figure 1). Moreover, these female patients were older (41.54 years old) as compared with the male group (33 years old).
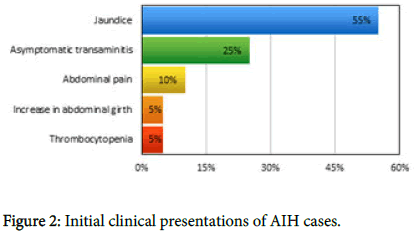
Jaundice (55%), asymptomatic transaminitis (25%) and abdominal pain (10%) were the most common initial clinical presentations in our study as shown in (Figure 2). Less common symptoms were an increase in abdominal girth and presence of thrombocytopenia.
The most common co-morbid illnesses were hypertension (15%) and cholelithiasis or cholecystolithiasis (15%). Three patients had coexisting autoimmune diseases - IgA Nephropathy (10%) and a case of hyperthyroidism (5%) that tested positive for anti-thyroglobulin (ATG)”. There were 2 patients (10%) with a family history of AIH (sisters). Another 2 (10%) had siblings with liver cirrhosis and there was 1 (5%) with a brother who had hepatocellular cancer. On review of their social history, there was only 1 (5%) who had a history of alcoholic beverage drinking and another 1 (5%) had history of food supplement (herbal drug) use.
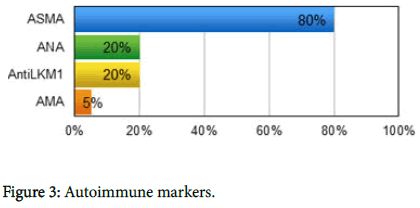
Among these patients, autoimmune markers supporting the diagnosis of AIH based on the international diagnostic criteria were tested and were found to be positive on the following: ASMA (80%), ANA (20%), Anti-LKM1 (20%), and Anti-mitochondrial antibody (AMA) (5%) (Figure 3).
Ultrasound results (Table 1) showed that 35% had chronic liver parenchymal disease, 25% had hepatomegaly, and 15% had fatty liver. Liver elastography was done in 8 cases and the results were as follows: F1 - 4 cases (20%), F2 - 1 case (5%), F3- 3 cases (15%), F4 – none. Patients who were clinically and by conventional ultrasound proved to be cirrhotic were no longer subjected to elastography. Only 3 patients had liver biopsy. Similarly, overtly cirrhotic patients were not biopsied.
| Ultrasound findings | Cases (%) |
|---|---|
| Normal liver and spleen | 4[20%] |
| Fatty Liver | |
| Fatty liver | 1[5%] |
| Moderate diffuse fatty liver | 1[5%] |
| Fatty liver with advanced fibrosis | 1[5%] |
| Hepatomegaly | |
| Hepatomegaly with signs of liver parenchymal disease | 2[10%] |
| Hepatomegaly with mild fatty changes | 3[15%] |
| Chronic liver parenchymal disease | |
| Chronic liver parenchymal disease | 2[10%] |
| Chronic liver parenchymal disease + portal hypertension | 3[15%] |
| Procedure not done | 3[15%] |
Table 1: Ultrasonography results of those with AIH.
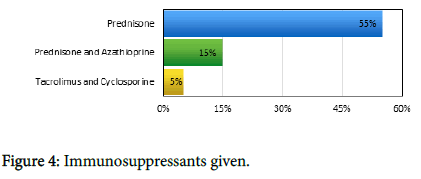
Furthermore, notable pre- and post-treatment laboratory test results (Table 2) of patients with AIH showed a reduction in the mean values of ALP from 144.33[87.72] to 102.85[28.86] IU/L, ALT from 192.32[311.97] to 97.12[121.4] IU/L, AST from 201.1[365.67] to 107.35[239.41] IU/L, total bilirubin levels from 11.77[14.37] to 5.2[7.67] mg/dL, and serum globulin levels from 3.75[0.64] to 3.36[0.62] g/L . Mean pre-treatment and post-treatment prothrombin time results (11.89[4.30] to 14.65[2.44]), as well as white blood cell counts (7.88[2.73] to 7.26[3.39]), platelet counts (273.33[124.01] to 241.19[107.17]) and hemoglobin levels (12.95[3.51] to 13.57[2.17]) were within the normal range. Among the laboratory tests monitored from baseline to 4-8 weeks post- treatment, total bilirubin levels (p=0.025) and platelet counts (p=0.039) showed statistically significant changes. As for the immunosuppressants given, 55% had been treated by Prednisone, 15% had Prednisone and Azathioprine, and 5% was given Tacrolimus and Cyclosporine as shown in Figure 4. The latter combination was no longer altered as this were the immunosuppressants given on a renal transplant patient.
| Pre-treatment | Post-treatment | ||||||
|---|---|---|---|---|---|---|---|
| Laboratory data of AIH patients | No. of cases | Abnormal (%) | Mean [SD] | No. of Cases | Abnormal (%) | Mean [SD] | p-value |
| ALP (NR 38-129) |
15 | 7[35%] | 144.33[87.72] | 13 | 3[15%] | 102.85[28.86] | 0.056 |
| ALT (NR 0-41 IU/L) |
19 | 13[65%] | 192.32[311.97] | 17 | 9[45%] | 97.12[121.4] | 0.058 |
| AST (NR 0-40 IU/L) |
16 | 10[50%] | 201.1[365.67] | 13 | 6[30%] | 107.35[239.41] | 0.131 |
| TBIL (NR 0-1 mg/dL) |
13 | 10[50%] | 11.77[14.37] | 15 | 11[55%] | 5.2[7.67] | 0.025 |
| Globulin (NR 3-3.5 g/dL) |
4 | 2[10%] | 3.75[0.64] | 5 | 2[10%] | 3.36[0.62] | 0.341 |
| WBC count (NR 4.5-11) |
18 | 2[10%] | 7.88[2.73] | 16 | 6[30%] | 7.26[3.39] | 0.294 |
| Platelet count (NR 150-400) |
18 | 3[15%] | 273.33[124.01] | 16 | 2[10%] | 241.19[107.17] | 0.039 |
| Hemoglobin (NR 12-16 g/dl) |
15 | 9[45%] | 12.95[3.51] | 13 | 4[20%] | 13.57[2.17] | 0.102 |
| Prothrombin time (NR 8.6-12.8) |
12 | 5[25%] | 11.89[4.30] | 6 | 4[20%] | 14.65[2.44] | 0.349 |
Table 2: Pre- and post-treatment laboratory results of AIH patients.
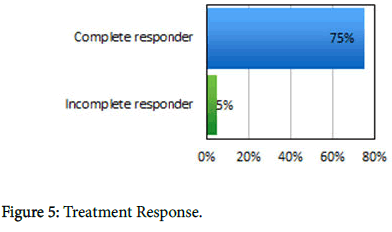
Other ancillary medications given to the patients were Propranolol (10%) for those with liver cirrhosis, Ursodeoxycholic acid (25%), Silymarin (15%), Zinc (10%), branched chain amino acids (5%) and Phospholipids (5%). Among the patients who were given immunosuppressants (75%), all responded completely except for one incomplete responder as shown in Figure 5. Two among those who completely responded had overlap syndrome. Lastly, 17 patients (85%) were reported to be alive and had good follow up as of this writing while 3 patients (15%) lost to follow up.
Discussion
From 2004 to 2014, the prevalence rate of Autoimmune Hepatitis (AIH) seen among those with liver diseases at the National Kidney and Transplant Institute was 0.62% CI 95% [0.4%-0.95%] (20 cases per 3,243) (Table 1). More cases of AIH were made in the past 3 years as a result of better and more available diagnostic tests and increase in awareness of the disease.The prevalence rate in our study is almost consistent with the findings in Europe and North America wherein AIH rate ranges from 0.1 to 1.9/100,000/year. Studies among Southeast Asians were limited but were comparable to studies done among Caucasians. In Southeast Asia, Jalihal et al. described 19 Bruneians seen in a hepatology clinic. The prevalence rate of the disease was 5.61/100 000 and this was higher in the Chinese than in Malays and Indigenous people [10].
As for the AIH patients’ demographics , their average age was 38.55 years old +/- 17.62, while 13(65%) were females with female to male ratio 1.85:1. Moreover, females were older (41.54 years old) as compared to males (33 years old). Females were also mostly at risk with AIH (14– 72 years old).
In Singapore and Thailand, the ratio between male:females are 1∶11 and 1∶6.1, respectively [16,17]. The ratio of 1:3.75 in our series is lower but comparable to those reported from Taiwan of China (1:3.4) and India (1:2.3 to 3) [4,11,12]. The reported age of diagnosis varies. In our series, the median age at diagnosis was 52 years. Studies from Thailand and Singapore reported older median ages (62 and 63 years, respectively) while Indian studies reported younger ages ranging from 31 to 43.6 years [11,18,19]. In Western countries, these have been reported to be around 40. Overall, the median age of patients with AIH in Southeast Asian seems to be older.
Furthermore, the most common presentations were jaundice (55%), asymptomatic transaminitis (25%), and abdominal pain (10%). This is similar to a study done by Choudhuri et al in India wherein the most common presentations were jaundice (55.2%) and abdominal pain (23.6%) [11]. Similarly, in Turkey, Kansu et al also reported jaundice to be present in all their patients with AIH [20]. As for the most common comorbid illnesses, 15% had hypertension, 15% had cholelithiasis/ cholecystolithiasis, and 10% had IgA Nephropathy. Concurrent immunological disorders are reported in some patients with diabetes, thyroiditis, even ulcerative colitis. Two patients in our study had IgA Nephropathy, one had DM, and another one patient had hyperthyroidism. Moreover, 10% had family history of AIH, hepatocellular cancer, and 10% liver cirrhosis. Whether the etiology of the liver cancer and cirrhosis in the other family members was also AIH was never ascertained as these information were just data recall and no serologic tests for AIH were apparently done.
The classification of AIH into different types is based on serum autoantibody profiles. Type I AIH is characterized by the presence of antinuclear antibody (ANA), anti-smooth muscle antibody (SMA), or both and constitutes 80% of AIH cases. Type 2 AIH is characterized by the presence of anti-liver kidney microsomal (LKM) 1 and/or anti- LKM3 and/or anti-liver cytosol 1 (LC1) antibodies. In our study, the autoimmune markers supporting the diagnosis of AIH based on the international diagnostic criteria that were positive include ASMA (80%), ANA (20%), AntiLKM1 (20%), and AMA (5%). These findings are similar to AIH patients from previous studies wherein Type I AIH is the predominant type.
In our study, ultrasonography showed that 35% had chronic liver parenchymal disease, with portal hypertension in 3 cases (15%), 25% with hepatomegaly, and 15% with fatty liver cases. In a study done by Kansu et al, cirrhosis with portal hypertension is an established associated condition of AIH patients [20]. Lok-Beng Koayet al in his study also reported 37% of AIH patients with liver cirrhosis [21]. In Singapore, India, and Thailand, approximately 40% also had cirrhosis at diagnosis [11,16,17]. Transient elastography is an alternative means of diagnosing liver fibrosis. Although no validated study has yet arise with regard to the use of liver elastography among AIH patients, there were 8 patients who underwent this test with the following results: F1 - 4 cases (20%), F2 - 1 case (5%), F3- 3 cases (15%), F4 - none. Furthermore, only 3 of the 20 patients in this study had undergone liver biopsy. No elastography and biopsies were no longer done on the cirrhotic patients. Steroid monotherapy or combination therapy with prednisone and azathioprine are the standard initial treatment of AIH. Combination therapy is best suited for elderly, osteoporotic patients, those with diabetes, hyper- tension, obesity and psychiatric disorders. Monotherapy with steroids is preferred in patients with hematological abnormalities and in young patients with fertility concerns.
Lok-Beng Koayet al also reported that, among patients with AIH, a substantial proportion of patients presented with poor liver function at entry similar to our study [21]. Although mean values of ALP, ALT, AST, total bilirubin and serum globulin levels were observed to reduce post-treatment, only reduction in the total bilirubin values showed significant reduction (p=0.025). Yet these post-treatment results are encouraging, although, due to such rare conditions, the sample sizes are not that large to yield statistically significant changes. In relation to treatment outcomes, Jalihal et al revealed that most of their patients achieved a biochemical response similar to our study [10].
With regards to patients outcomes, 85% were reported to have good response and with good compliance to follow-up while 15% were lost to follow up. Similar to a published report, 10% of patients in our study had AIH-PSC overlap syndrome [14]. Kansu et al highlighted that autoimmune hepatitis carries a high mortality if left untreated but has a favorable outcome when treatment is initiated early in the course of the disease [20].
Conclusion
The prevalence rate of Autoimmune Hepatitis (AIH) seen among those with liver diseases at National Kidney and Transplant Institute was 0.62% CI 95% [0.4%-0.95%]. Their average age was 38.55 +/- 17.62years old with a female:male ratio of 1.85:1. The most commonly presenting symptoms of patients with AIH were asymptomatic transaminitis, jaundice and abdominal pain. Family history was notable for AIH and liver cirrhosis in siblings. A majority of these patients has positive ASMA (80%). Ultrasonography results done among our study population showed chronic liver parenchymal disease +/- portal hypertension hepatomegaly, and fatty liver cases. Although that the mean values of the patients’ ALP, ALT, AST, total bilirubin and globulin levels have reduced post-treatment, only total bilirubin values reduction showed significant reduction. Although platelet counts were also observed to decrease significantly, pre- and post-treatment values remained to be within the normal range. A majority were given Prednisone as monotherapy with good response. There were 85% were reported to be alive while 15% lost to follow up.
Limitations
Since this study was done retrospectively, there were biochemical tests that were not done on some patients. Biopsy was also not done in a majority of patients. However even in the absence of biopsies, treatment was not withheld especially among patients who are clearly in need of therapy.
Recommendation
A multi-center prospective study is recommended by the authors to be able to describe the course of this rare Filipino liver disease in detail.
References
- Mittal MK (2007) Severe hypercalcemia as a harbinger of acute lymphoblastic leukemia. Pediatr Emerg Care 23: 397-400.
- Hye-Jin P, Eun-Jin C, Jin-Kyung K (2016) A successful treatment of hypercalcemia with zoledronic acid in a 15-year-old boy with acute lymphoblastic leukemia. Ann Pediatr Endocrinol Metab 21: 99-104.
- Bahoush G, Miri-Aliabad G (2014) Severe hypercalcemia: A rare and unusual presentation of childhood acute lymphoblastic leukemia. Int J Hematol Oncol Stem Cell Res 8: 38-40.
- Yang J, Zhou X, Wang B, Gao C, Zhang RD, et al. (2009) Severe hypercalcemia complicated in acute lymphoblastic leukemia (ALL) with E2A-HLF fusion gene: Report of two cases and literature review. Chin J Hematol 30: 615.
- Sato A, Imaizumi M, Chikaoka S, Niizuma H, Hoshi Y, et al. (2004) Acute renal failure due to leukemic cell infiltration followed by relapse at multiple extramedullary sites in a child with acute lymphoblastic leukemia. Leuk Lymphoma 45: 825-828.
- Buonuomo PS, Ruggiero A, Piastra M, Riccardi R, Polidori G, et al. (2004) A case of acute lymphoblastic leukemia presenting as severe Hypercalcemia. Pediatr Hemat Oncol 21: 475-479.
- Sultan I, Kraveka JM, Lazarchick J (2004) CD19 negative precursor B acute lymphoblastic leukemia presenting with hypercalcemia. Pediatr Blood Cancer 43: 66-69.
- Lokadasan R, Prem S, Koshy SM, Jayasudha AV (2015) Hypercalcaemia with disseminated osteolytic lesions: A rare presentation of childhood acute lymphoblastic leukaemia. Ecancermedicalscience 9: 553–561.
- Oloomi Z (2012) Acute lymphoblastic leukemia without circulating blasts presenting as severe hypercalcemia. Acta Med Iran 45: 76-78.
- Hooman N (2013) Bisphosphonates for treatment of severe idiopathic infantile hypercalcemia. Iran J Kidney Dis 7: 79-81.
- Lassaletta A, Perez A, Díaz MA, Sevilla J, González-Vicent M, et al. (2004) Successful treatment of invasive aspergillosis with oral voriconazole following intravenous liposomal amphotericin in a child with acute lymphoblastic leukemia. J Pediatr Hematol Oncol 26: 117-119.
- Mathur M, Sykes JA, Saxena VR, Rao SP, Goldman GM (2003) Treatment of acute lymphoblastic leukemia-induced extreme hypercalcemia with pamidronate and calcitonin. Pediatr Crit Care Med 4: 252-255.
- Kumar C G, Biswal N, Kayal S (2016) A typical presentation of acute lymphoblastic leukemia in a 7 year old child. Indian J Hematol Blood Transfus 32: 8-10.
- Marwah A, Kumar R, Dasan J B, Choudhury S, Bandopadhyaya, G et al. (2002) Soft tissue uptake of Tc99m-MDP in acute lymphoblastic leukemia. Clin Imaging 26: 206-208.
- Ganesan P, Thulkar S, Gupta R, Bakhshi (2009) Childhood aleukemic leukemia with hypercalcemia and bone lesions mimicking metabolic bone disease. J Pediatr Endocrinol Metab 22: 463-467.
- Junior J, Armelin Benites EC, Santos Fernandes GSD, Freddi N A, Koga W, et al. (2015) Case Report: Pulmonary alveolar calcification as a result of severe hypercalcemia due to acute lymphoblatic leukemia. F1000 Res 4: 111.
- Soni P N (1993) Hypercalcaemia and multiple osteolytic lesions in childhood acute lymphoblastic leukaemia. Postgrad Med J 69: 483-485.
- Laffan MA, Talavera JG, Catovsky D (1986) Hypercalcaemia in t cell acute lymphoblastic leukaemia: Report of two cases. J Clin Pathol 39: 1143-1146.
- Perez-Alonso P, Salinas S (2000) Pathologic quiz case – The importance of the autopsy in a pediatric case with atypical features – Acute lymphoblastic leukemia. Arch Pathol Lab Med 124: 1846-1848.
- Niizuma H, Fujii K, Sato A, Fujiwara I, Takeyama J, et al. (2008) PTHrP-independent hypercalcemia with increased proinflammatory cytokines and bone resorption in two children with CD19-negative precursor B acute lymphoblastic leukemia. Pediatr Blood Cancer 49(7): 990-993.
- Tagiyev A, Demirbilek H, Tavil B, Buyukyilmaz G, Gumruk F, et al. (2016) Severe hypercalcemia in a child with acute lymphoblasticleukemia relapse: Successful management with combination of calcitonin and bisphosphonate. J Pediatr Hematol Oncol 38: 232-234.
- Kolyva S, Efthymiadou A, Gkentzi D, Karana-Ginopoulou A, Varvarigou A (2014) Hypercalcemia and osteolytic lesions as presenting symptoms of acute lymphoblastic leukemia in childhood. The use of zoledronic acid and review of the literature. J Pediatr Endocrinol Metab 27: 349-354.
- Sherief LM, Azab SF, Zakaria MM, Kamal NM, Elbasset Aly MA, et al. (2015) Renal presentation in pediatric acute leukemia: Report of 2 cases. Medicine 94: 1461.
- Moayeri H, Oloomi Z, Sambo SA (2011) A cross-sectional study to determine the prevalence of calcium metabolic disorder in malignant childhood cancers in patients admitted to the pediatric ward of Vali-Asr Hospital. Acta Med Iran 49: 818-823.
- Liu MN, Luo XQ, Lu YY, Hong-shan C, Zhen-yu S (2007) One case report and review of literatures of acute lymphoblastic leukemia presenting with hypercalcemia at initial. J Appl Clln Pediatr 22: 1160-1161.
- Rajagopal R, Su HL, Jalaludin MY, Krishnan S, Abdullah WA, et al. (2013) Hypercalcaemia: An unusual presenting feature of childhood acute lymphoblastic leukaemia. Br J Haematol 163: 147-147.
- Trehan A, Cheetham T, Bailey S (2009) Hypercalcemia in acute lymphoblastic leukemia: An overview. J Pediatr Hematol Oncol 31: 424-427.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi