Research Article, J Spine Neurosurg Vol: 6 Issue: 5
Cranio-Cervical Trauma Eidemiology, Classification, Diagnosis And Management
Amar Saxena*
Department of Neurosurgery, University Hospitals of Coventry and Warwickshire, United Kingdom, Regional Specialty Professional Advisor in Neurosurgery for West Midlands, UK
*Corresponding Author : Dr. Amar Saxena MCh, FRCS (Eng), FRCS (SN)
Department of Neurosurgery, University Hospitals of Coventry and Warwickshire, Clifford Bridge Road, Coventry, CV2 2DX, United Kingdom
Tel: +44 7771852449
Fax: +442476965210
E-mail: saxenaamar7@yahoo.co.uk, amar.saxena@uhcw.nhs.uk
Received: October 26, 2017 Accepted: November 17, 2017 Published: November 25, 2017
Citation: Saxena A (2017) Cranio-Cervical Trauma Eidemiology, Classification, Diagnosis and Management. J Spine Neurosurg 6:5. doi: 10.4172/2325-9701.1000284
Abstract
Objective: To provide an overview of current knowledge of the management of Cranio-Cervical (Occipito-cervical) injuries.
Method: Literature search for new trends in the management of Cranio-cervical injuries. The article is divided into subheadings of Introduction, Epidemiology, pre-disposing factors and Anatomy of the Cranio-cervical junction including relevant surgical anatomy. NICE guidelines for management of cervical spine injuries and its recommendations are mentioned. This is followed by description of individual fractures, including their classification, clinical presentation and management. Recent advances in the management of individual fractures are mentioned with reference. The fractures covered are Occipital Condylar fractures (including Traumatic Atlanto-Occipital Dislocation), C1 Fractures (including Jefferson Fracture) and Odontoid fractures (including Hangman’s fracture) with brief description of surgical techniques to stabilize these fractures. Results: Cranio-cervical junction is a very tough construct and it requires very strong forces to result in occipito-cervical bony or ligamentous injuries. Cranio-cervical injuries must be suspected in high velocity injuries like RTAs and also in the elderly with neck pain and stiffness following a fall. Since Conventional cervical spine plain films can miss injuries in this region, there is need for a high index of suspicion as elaborated by NICE guidelines. There are new trends in the surgical management of Jefferson’s fractures (Posterior osteosynthesis) and Hangman’s fractures of C2 (Anterior approach better)
Conclusion: Cranio-cervical injuries constitute a significant proportion of high velocity trauma and can be missed. There is a need for high index of suspicion in such patients. Recent trends seem to favour surgical management of these injuries even in the elderly. Aim should be early surgical fixation wherever possible even in elderly patients, if there is no significant co-morbidity or contraindication for surgery.
Keywords: Cervical spine; Cranio-cervical junction; Neuro-trauma; High velocity injury; Occipital condyle; Jefferson’s Fracture; Hangman’s fracture; Harms technique; Anterior lag screw
Introduction
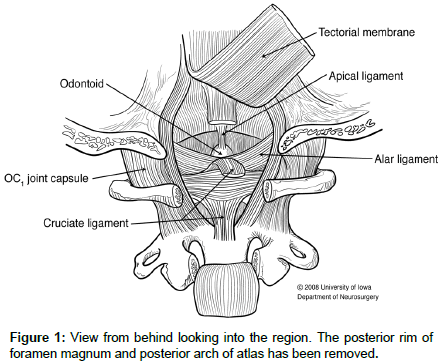
Civilian trauma is the leading cause of death in people aged 5–44 years in developed countries accounting for 10% of deaths [1,2]. The overall mortality for patients with spinal injuries has remained relatively unchanged at 17% over the last 20 years [3]. The reported annual incidence for spinal fractures varies from 19 to 88 per 100,000 persons and for spinal cord injuries between 14 to 53 per million [3-9]. About half of severe spine injuries are reportedly not suspected in the pre-hospital setting [10]. Identification of spinal injuries during initial trauma evaluation is challenging, as patients often have a reduced level of consciousness due to other injuries or are under the influence of sedative and/or analgesic medication. This is particularly true in cranio-cervical junction injuries. 20% of all fatal victims of RTA have an associated severe cervical spinal cord injury. 80% of these involve C1, C2 or occiput. Early detection of spinal injuries in the Emergency Department is important in order to initiate further diagnostic testing and treatment and to avoid additional spinal injury. NICE (National Institute of Clinical Excellence) has developed guidelines for such an evaluation. This article is a review of the anatomy of cranio-cervical junction epidemiology of the spinal injuries (including those of the cranio-cervical junction). This article includes the classification and management (including updated surgical management) of injuries of the cranio-cervical junction (Figure 1).
Epidemiology of cervical spine (including Occipito-cervical junction) injuries
The data obtained from a European cohort study on predictors of spinal injury in adult (≥16 years) major trauma patients, using prospectively collected data of the Trauma Audit and Research Network (TARN Registry) from 1988 to 2009 showed the incidence as follows. This probably is the largest study published on spinal injuries [11]. 250,584 patients were analysed. 9.6% had sustained spinal fractures/dislocations alone and1.8% had sustained spinal cord injury with or without fractures/dislocations. Spinal injury patients had a median age of 44.5 years and majority (64.9%) were males. 45% of patients suffered associated injuries to other body regions. Age <45 years, Glasgow Coma Score (GCS) 3–8, falls >2 m, sports injuries and road traffic collisions (RTCs) were predictors for spinal fractures/dislocations [11]. Age <45 years, male gender, GCS <15, associated chest injury, sports injuries, falls >2 m, RTCs and shooting were predictors for spinal cord injury. Multilevel injury was found in 10.4% of fractures/dislocations and in 1.3% of cord injury patients. As spinal trauma occurred in >10% of major trauma patients, aggressive evaluation of the spine is warranted, especially, in males, patients <45 years, with a GCS <15, concomitant chest injury and/or dangerous injury mechanisms (falls >2 m, sports injuries, RTCs and shooting). Diagnostic imaging of the whole spine and a diligent search for associated injuries are substantial [11] (Figure 2).
Mode of injury
Majority of injuries are due to RTA (50%), followed by falls (21%) injuries are due to falls (mainly in older population), Sports related injuries account for14% and Gunshot injuries in 14% [12]. 60% of spinal cord injuries occur under 30 years of age, although occurrence in childhood and adolescence is uncommon. 20% of all fatal victims of Road Traffic Accidents have an associated severe cervical spinal cord injury. 80% of these involve C1, C2 or occiput. Studies have shown that in auto injuries which require towing from the scene of the accident, cervical spine injuries occur with a frequency of 1 in 300 victims. If an occupant is ejected from the vehicle, the frequency increases to 1 in 9 [13] (Figure 3).
Predisposing factors
Most important factor is associated serious head or trunk injury. Other factors include alcohol intoxication. A number of underlying medical diseases may also predispose to the development of spinal or spinal cord injury. These include 1) Generalised seizure disorder, 2) unrecognised metastatic spinal disease 3) Advanced degenerative disease in the elderly and 4) existence of underlying congenital or developmental cervical spine disease. These include a) Ankylosing spondylitis. b) Degenerative spondylosis c) Congenital fusion of cervical vertebrae.
Anatomy of the occipito cervical junction
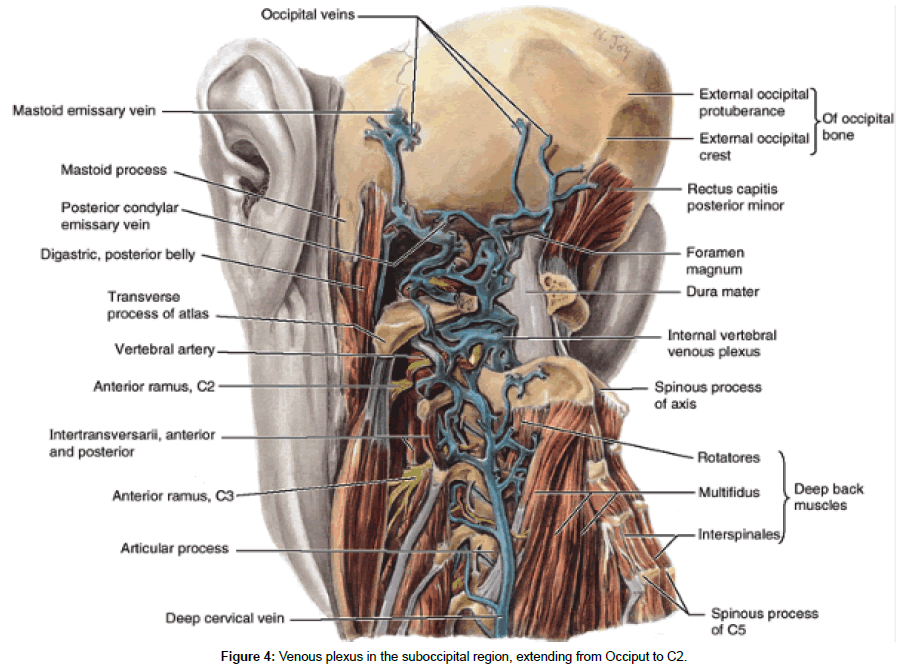
The cranio-cervical (cranio-vertebral) junction represents the complex transitional zone between the cranium and the spine. It should be considered anatomically and radiologically distinct from cranium as well as the cervical spine. It is composed of bony structures articulating with synovial joints, strong intrinsic ligaments, membranes and muscles. It not only protects the brain stem, the spinal cord and cranial nerves, but the critical vasculature supplying the brain and the cervical spinal cord lies in its close vicinity. Injury to the cranio-cervical junction carries the potential for devastating morbidity and significant mortality. The requirements placed on the cranio-cervical junction are onerous—not only must it house, protect and support structures critical for function (and ultimately survival), it must also simultaneously provide significant mobility and stability to the region (Figure 4).
Anatomy of Cranio-vertebral junction (Ligamentous)
The cranio-cervical articulation contains two groups of ligaments. 1) First set of ligaments connect the Occiput to the first cervical vertebra C1 by the anterior capsule ligaments, the anterior and posterior atlanto-occipital membrane ligaments and the two lateral atlanto–occipital ligaments. The cruciate ligament (a longitudinally oriented structure (associated with the transverse ligament of the atlas) provides additional stability to the articulation. Principal stabilizing ligaments of the Atlas are 1) Transverse ligament of the Atlas and 2) Alar ligaments.
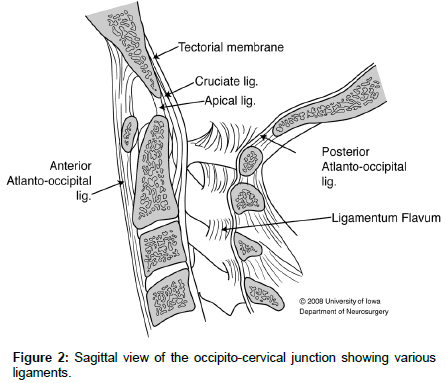
Secondary stabilizing ligaments of Cranio-cervical junction include: 1) Anterior Atlantooccipital membrane. 2) Posterior Atlanto- Occipital membranes. 3) Apical ligament. 4)Tectorial membrane. 5) Ligamentum flavum. 6) Anterior & Posterior Longitudinal Ligaments and 7) Capsular ligaments. These ligaments are more elastic & weaker than the primary ligaments (Figure 5).
Atlanto-occipital ligaments
A) Anterior Atlanto-occipital Membrane: Ligament is continuous caudally with the anterior Atlanto-axial ligament & through it to the Anterior Longitudinal Ligament of the spinal column. It acts as a tension band that stretches during extension, serving as a secondary stabilizer against this motion. B) Posterior Atlanto-Occipital Membrane: This is a weaker ligament containing no significant elastic tissue. Ligament is firmly attached to the dura anteriorly. It is loose between the bones & does not limit their motion. Ligament invests itself on either side to form a canal through which the vertebral artery, accompanying veins, & the first cranial nerve pass. C) Lateral Atlanto-Occiptal Ligaments: Ascending ligament, which reinforces the Atlanto-Occipital joint capsules.
Atlantoaxial ligaments
These connect the atlas with the Axis (C2 vertebra) and include:
1) Anterior Atlanto-axial ligament,
2) Posterior Atlanto-axial ligament
3) Transverse ligament of the atlas: This is a thick and strong ligament and is about 6mm in height. This ligament presents a fibrocartilagenous surface ventrally allowing a free gliding motion to occur over the posterior facet of the dens. Transverse Ligament effectively limits anterior translation and flexion of the atlanto-axial joint. Caudal crus & Rostral crus fibres joined with transverse ligament on its dorsal aspect to form Cruciate ligament of atlas. An accessory band ventral to the ascending crus attaching to the apex of the odontoid process is termed Gerber’s ligament. The force required to rupture the transverse ligament ranged from 12 to 180 kp (mean 84kp) under slow loading & about 111 kp under rapid loading (Figure 6).
2) The second set of ligaments coursing from the occiput to the second cervical vertebra C2 provides the major structural support for the cranio-cervical junction. These ligaments include apical dental ligament, the paired alar ligaments and the tectorial membrane. These also provide major structural support for the cranio-cervical junction.
A) Apical Ligament: slender band of fibres about 2-5mm wide & 2-8mm long containing small amount of collagen & elastic fibres. It has no mechanical significance.
B) Alar Ligaments: These are two strong cords that attach to the dorsal lateral body of the dens. They are ventral & cranial to the transverse ligament. Alar ligaments allow an anterior shift of C1 from 3 to 5 mm. They strengthen the Atlanto-Occipital capsule
C) Tectorial Membrane: It is a strong band of longitudinally oriented fibres attached to the dorsal surface of the C3 vertebra, axis body & to the body of dens. It is the rostral extension of the PLL of the vertebral column. Tectorial membrane is essential for limiting flexion and hyperextension.
Muscles: Muscles have only a minor role related to CVJ stabilization & do not limit the movements of the joints.
An important anatomical feature is the presence of a large plexus of veins between the Occipital bone and atlas an between atlas and the Axis. This could cause troublesome bleeding during instrumentation between C1 and C2 (Figure 7).
Contents
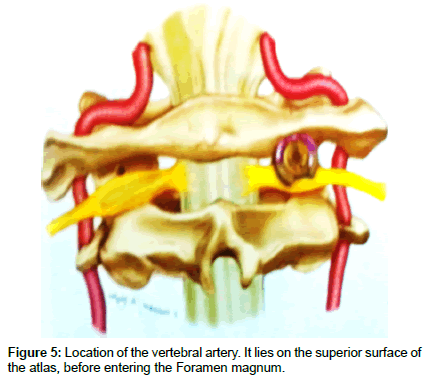
Neural structures related to Cranio-cervical junction are 1) Caudal brainstem (Medulla Oblongata) 2) Cerebellum (tonsils and vermis), 3) fourth ventricle 4) Rostral part of spinal cord 5) Lower cranial nerves & 6) Upper cervical nerves. The only cranial nerve that crosses the cranio-cervical junction by passing through the Foramen Magnum is the spinal accessary nerve. Major Vascular structures related to the cranio-cervical junction are: 1) The vertebral arteries 2) Postero-inferior cerebellar arteries (PICA), 3) Internal carotid arteries and 4) External carotid arteries. It is important to understand that the vertebral artery lies horizontally in a groove on the superior surface of the Atlas about 10mm on either side of the midline, before entering the foramen magnum. One has to be very careful while dissecting in the region of the atlas to avoid injury to the vertebral artery. It also lies (unprotected and exposed) close to the emerging C2 nerve root between the transverse processes of the C1 and C2.
Motion at Cranio-cervical junction
Joints at the Cranio-vertebral junction are unique in that they bear weight through synovial joints (rather than through discs as in the rest of the spine). This allows significantly more movement than at any other spinal level 14. A). ROTATION occurs when movement occurs about an axis. B). TRANSLATION occurs when movement occurs along an axis. The C1 lateral masses contain the occipital condyles in a cup-like fashion, facilitating flexion and extension (Figure 8).
Atlanto-occipital joints
The C1 lateral masses contain the occipital condyles in a cuplike fashion, facilitating flexion and extension. The condyles of these paired joints in sagittal direction are arcuate & thus due to this anatomy, motion about the vertical axis is not possible. Thus, this joint has movement only around the transverse & A-P axes. These joints allow forward or backward bending (nodding of head) & a slight lateral tilting motion to either side. They do not permit rotation.
Atlanto-axial joints
Rotation of atlas occurs around the odontoid process like a wheel around an axle & its axis passes centrally through the annulus osteofibrosis. The superior facet of the axis is convex & the inferior facet of the atlas is either horizontal or slightly convex with horizontal orientation of the articulation. Because of this, these facets slide forward & backward on each other with rotation. The Atlanto-axial joints allow less flexion and extension motion than rotation [14].
Movements at the Cranio-cervical junction
Flexion and extension at the Atlanto-occipital joints are more than the Atlanto-axial joints (flexion 10 degrees and extension is 25 degrees). Total rotation of the entire cervical spine is up to 90 degree and approximately half of this rotation occurs at the atlanto-axial joint. Rotation with accompanying lateral flexion in the cervical spine occurs below the axis (C2) [14] (Figure 9).
Prevention of excessive motion at the Cranio-cervical junction
The ligaments at the cranio-cervical junction restrict extreme motion. Hyperextension is limited by tectorial membrane and lateral flexion and Rotation by alar ligaments. Excessive flexion is limited by Anterior arch C1 contacting the basion and Anterior translation is limited by transverse ligament. Normal Atlanto-axial motion: Approximately 47.5 degrees of rotation and 10 degrees of Flexion and extension occur at the C1-C2 junction.
NICE (National Institute of Clinical Excellence, UK) Guidelines for suspected C-Spine Fractures has recommended [15]:
1. Trauma patients who are alert, awake with no mental status changes, no neck pain and no deficit may be considered to be stable and no radiological studies are needed.
Sequential approach to assessment for spinal injury in the emergency department (same rules apply in the Pre-Hospital setting):
On arrival at the emergency department, use a prioritizing sequence to assess people with suspected trauma, for example ABCDE:
i) Catastrophic hemorrhage
ii) Airway with in-line spinal immobilization (see airway management)
iii) Breathing
iv) Circulation
v) Disability (neurological)
vi) Exposure and environment.
At all stages of the assessment:
i) Protect the person’s cervical spine with manual in-line spinal immobilization, particularly during any airway intervention, and avoid moving the remainder of the spine or maintain full in-line spinal immobilization. ii) Make eye contact and be in the patient’s eye line to ensure you are visible when communicating with this person to avoid them moving their head (Figure 10).
Initial factors to take into consideration in hospital assess the person for spinal injury, initially taking into account the factors listed below.
Check if the person is
i) Under the influence of drugs or alcohol ii) Confused or uncooperative
Check if the person has
i) Any significant distracting injuries ii) Reduced level of consciousness iii) Spinal pain iv) Any hand and/or foot weakness (motor assessment). v) Altered or absent sensation in the hands or feet (sensory assessment) vi) Priapism (unconscious or exposed male) vii) A history of past spinal problems, including previous spinal surgery or conditions that predispose to instability of the spine i.e., Ankylosing spondylitis (Figure 11).
Figure 11: Dickman Classification. Clockwise from top left picture. Picture A (top left)= Disruption of the transverse ligament in the mid-portion. B (top right) = Bony evulsion. C (Bottom left)= Disruption of the transverse ligament at the insertion of medial tubercle. D (bottom right) = Bony evulsion.
A&C= Dickman type I B&D = Dickman type II
Assess whether the person is at high, low or no risk for cervical spine injury using the Canadian C‑spine rule as follows:
1. The person is at high risk if they have at least one of the following high‑risk factors
1. Age: 65 years or older
2. Dangerous mechanism of injury: Fall from a height of greater than 1 metre or 5 steps, Axial load to the head – for example diving, High‑speed motor vehicle collision, Rollover motor accident, Ejection from a motor vehicle, Accident involving motorised recreational vehicles, Bicycle collision, Horse riding accidents.
2. Paraesthesia in the upper or lower limbs
2. The person is at low risk if they have at least one of the following low‑risk factors:
a) Involved in a minor rear‑end motor vehicle collision. b) Comfortable in a sitting position
c) Ambulatory at any time since the injury. d) No midline cervical spine tenderness. e) Delayed onset of neck pain.
3. The person remains at low risk if they are
Unable to actively rotate their neck 45 degrees to the left and right (the range of the neck can only be assessed safely if the person is at low risk and there are no high‑risk factors).
4. The person has no risk if they
Have one of the above low‑risk factors and Are able to actively rotate their neck 45 degrees to the left and right.
Assessment of the person with suspected thoracic or lumbosacral spine injury using these factors:
a. Age 65 years or older and reported pain in the thoracic or lumbosacral spine
b. Dangerous mechanism of injury (fall from a height of greater than 3 metres, axial load to the head or base of the spine – for example falls landing on feet or buttocks, high‑speed motor vehicle collision, rollover motor accident, lap belt restraint only, ejection from a motor vehicle, accident involving motorised recreational vehicles, bicycle collision, horse riding accidents)
c. Pre-existing spinal pathology, or known or at risk of osteoporosis – for example steroid use
d. Suspected spinal fracture in another region of the spine
e. Abnormal neurological symptoms (paraesthesia or weakness or numbness)
On examination:
a) Abnormal neurological signs (motor or sensory deficit). b) New deformity or bony midline tenderness (on palpation) c) Bony midline tenderness (on percussion) d) Midline or spinal pain (on coughing) e) On mobilisation (sit, stand, step, assess walking): pain or abnormal neurological symptoms (stop if this occurs) (Figure 12).
When to carry out or maintain full in‑line spinal immobilisation Carry out or maintain full in‑line spinal immobilisation if: A highrisk factor for cervical spine injury is identified and indicated by the Canadian C‑spine rule A low-risk factor for cervical spine injury is identified and indicated by the Canadian C‑spine rule and the person is unable to actively rotate their neck 45 degrees left and right Indicated by one or more of the factors listed in recommendation Do not carry out or maintain full in‑line spinal immobilisation in people if: They have low‑risk factors for cervical spine injury as identified and indicated by the Canadian C‑spine rule, are pain free and are able to actively rotate their neck 45 degrees left and right. They do not have any of the factors listed in recommendation How to carry out full in‑line spinal immobilisation When immobilising the spine tailor the approach to the person’s specific circumstances (see Recommendations The use of spinal immobilisation devices may be difficult (for example in people with short or wide necks, or people with a pre‑existing deformity) and could be counterproductive (for example increasing pain, worsening neurological signs and symptoms). In uncooperative, agitated or distressed people, including children, think about letting them find a position where they are comfortable with manual in‑line spinal immobilisation.
When carrying out full in‑line spinal immobilisation in adults, manually stabilise the head with the spine in‑line using the following stepwise approach:
1. Fit an appropriately sized semi‑rigid collar unless contraindicated by:
a) A compromised airway
b) Known spinal deformities, such as ankylosing spondylitis (in these cases keep the spine in the person’s current position).
2. Reassess the airway after applying the collar.
3. Place and secure the person on a scoop stretcher.
4. Secure the person with head blocks and tape, ideally in a vacuum mattress.
Diagnostic imaging- RECOMMENDATIONS
1. CT SCAN
CT should be used as the primary imaging modality for excluding cervical spine injury in adults following blunt trauma if any of the following criteria are met (level two evidence):
a) GCS below 13 on initial assessment b) Intubated patients. c) Inadequate plain film series
d) Suspicion or certainty of abnormality on plain film series* e) Patient’s being scanned for head injury or multi-region trauma
*As a minimum CT should cover the area from the cranio-cervical junction to the thoraco-cervical junction since selective scanning has been shown to miss injuries (NICE guidelines, 2007) It is also recommended that CT be used as the primary imaging modality in the following settings:
a) Patient has dementia (or a chronic disability precluding accurate clinical assessment)
b) Patient has neurological signs and symptoms referable to the cervical spine c) Patient has severe neck pain ( ≥ 7/10 severity)
d) Patient has a significantly reduced range of neck movement (i.e. unable to actively rotate the neck 45 degrees in both directions)
e) Patients with known vertebral disease (e.g. ankylosing spondylitis, rheumatoid arthritis, spinal stenosis, or previous cervical surgery)
PLAIN RADIOGRAPHS: lain radiographs: In the absence of an indication for CT, 3-view plain radiographs should be used as the primary imaging modality for excluding cervical spine injury Imaging for spinal injury should be performed urgently, and the images should be interpreted immediately by a healthcare professional with training and skills in this area.
Timing of the Imaging
Imaging of the cervical spine should be performed within 1 hour of a request having been received by the radiology department or when the patient is sufficiently stable (level five evidence). If the patient is having an urgent CT head performed then the neck should be scanned at the same time (Figure 13).
A radiologist (or clinician specifically trained to perform this task) should formally report the CT cervical spine scan images promptly.
2. MRI SCAN
MRI should be used to exclude cervical spine injury* in adults following blunt trauma if any of the following criteria are met:
a) Neurological signs and symptoms referable to the cervical spine
b) Suspicion of vertebral artery injury (e.g., spinal column displacement, foramen transversarium or lateral process fracture, posterior circulation syndromes).
*MRI should always be used in conjunction with another modality, preferably CT, in order not to miss bony injuries.
c) Further imaging is advised for adults with severely restricted neck movement or severe pain (≥ 7/10) despite a normal CT following blunt cervical spine injury (level four evidence). d) Further imaging is advised for adults with severely restricted neck movement or severe pain (≥ 7/10) despite a normal CT following blunt cervical spine injury (level four evidence). Flexion-extension views cannot reliably exclude unstable cervical spine injuries in the acute setting (level three evidence).
e) In author’s opinion, if the CT demonstrates fracture dislocation, an MRI scan of the cervical spine should be done to rule out breach of PLL and disc disruption before subjecting the patient to cervical traction prior to fixation. In the acute phase MRI is the imaging modality of choice (level 2 evidence). When indicated, MRI should be performed as soon as possible as its sensitivity for injury identification may fall after 48 hours (level four evidence). Patients with injuries identified on MRI should be discussed with spinal surgeons (level five evidence). Patients without fracture or neurological deficit can be discharged following a negative MRI scan (level two evidence).
Before removing the cervical spine immobilization devices, all radiographs should be read by an experienced ED physician, neurosurgeon, orthopedic surgeon, radiologist or other physician with expertise in interpreting these studies.
3. Trauma patients who have an altered level of conscious due to a traumatic brain injury or due to other causes which are likely to leave the patient unable to complain of neck pain or neurological deficits for 24 hours after their injury: may be considered to have a stable spine if after adequate three view plain X-rays (CT supplement as necessary) and thin cut axial CT images through C1 and C2 are read as normal by an experienced physician. If the patient has abnormalities of the C-spine discovered on any radiographic or MRI images as recommended above, the surgical sub-specialty responsible for spine trauma should be consulted.
Individual fractures
Occipital Condylar fracture OCF
Occipital condylar fractures were first described by Bell in 1817 and occipital condylar fractures and severe head trauma was initially drawn in autopsy series with an incidence as high as 4% in fatal head injuries [16,17].
Conventional cervical spine plain films miss between 50-93% of occipital condyle fractures which are the most common cervical spine fracture missed by radiology residents [18-20]. With routine CT scan in high energy trauma the spectrum of this disease has become much better elucidated. Occipital condyle fractures should be suspected in trauma patients with lower cranial nerve palsies, upper cervical spine mobility restriction or persistent neck pain. This kind of injury may be associated with Injuries to the vertebral artery, Brain stem, cervical cord, nerve roots, lower cranial nerves etc. Most common cranial nerve involved is the hypoglossal nerve. Full clinical assessment is often difficult because many patients have concomitant traumatic brain injury and altered level of consciousness.
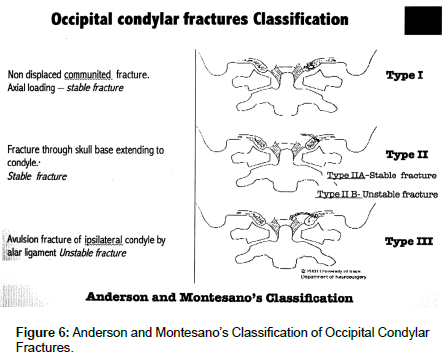
Classification of condylar fractures
Anderson and Montesano Classification: The most commonly used classification for Condylar fractures is that of Anderson and Montesano from 1988 based on the description of only six cases [21].
Type I: Non-displaced communited condylar fracture. This is a communited impaction fracture resulting from axial loading. These are stable injuries and the treatment is immobilisation in a Semirigid Cervical collar. Type II: It is a fracture of the condyl extending through skull base extending to condyle. Usually this is a stable injury and treated in a Cervical Collar. Type III: This fracture involves Avulsion fracture of the ipsilateral condyle by alar ligament. According to Anderson and Montesano only type III fracture would be considered to be unstable. Treatment is immobilisation in a Halo/Minerva jacket or Surgical fixation.
Tuli Classification: Tuli et al proposed a new system of classification [22]. This system takes into account ligamentous injury as seen on MRI scan to define the stability of the fracture.
Type I fractures are undisplaced and stable (Figure 14).
Type II fractures are divided into two subtypes A and B. Type IIA is a displaced fracture of the occipital condyl with stability at the occiput-C-C2 levels. The treatment is Immobilisation in semi-rigid cervical collar. In Type IIB fractures there is instability at the occiput- C-C2 levels as demonstrated by imaging [23]. Treatment is either immobilisation in a Halo or internal fixation Traumatic Atlanto- Occipital Dislocation
Mechanism of injury A) Hyperextension Atlanto occipital dislocations are high velocity, high force injuries. Typically AO dislocations results from distraction with extreme hyperextension and rupture of the tectorial membrane (the cranial extension of the posterior longitudinal ligament. Other mechanisms are B) Extreme lateral flexion resulting in Injury to alar ligament and C) Hyperflexion leading to the separation of posterior elements. This injury has the highest incidence in paediatric age group but can occur in adults following high velocity injuries. Death from AO dislocation results most commonly from respiratory depression secondary to neurogenic shock. Classically, AO dislocation was considered fatal. Survival is now common perhaps due to increased sensitivity of detection during trauma survey. The diagnosis of AO dislocation is frequently delayed or missed in patients who present neurologically intact or incomplete neurology [24] (Figure 15).
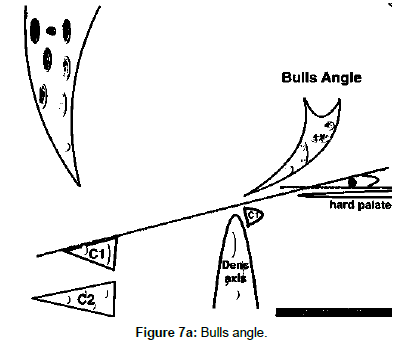
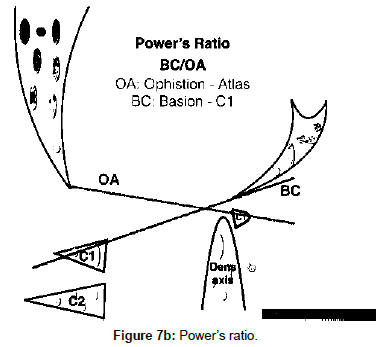
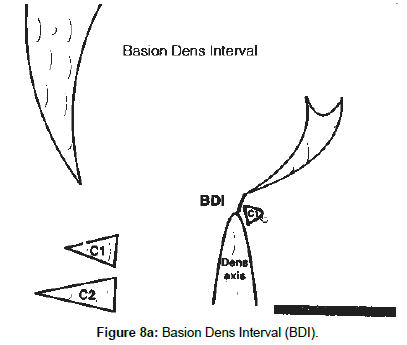
There are many methods for radiographic evaluation of AO dislocation involving calculation of various angles, lines and ratios as below [25,26]
Bulls Angle: Draw a line between posterior and anterior arch of C1à⋄angle between this line and the hard palate. Pathological: >13 degrees
Power’s ratio: is the distance from the tip of the basion to the posterior arch of C1 (B-C) divided by the distance from tip of the opisthion to tip of the ododntoid (anterior arch of atlas) (O-O). Ratios greater than 1 suggest anterior AO dislocation.
Pathological ratio: >1
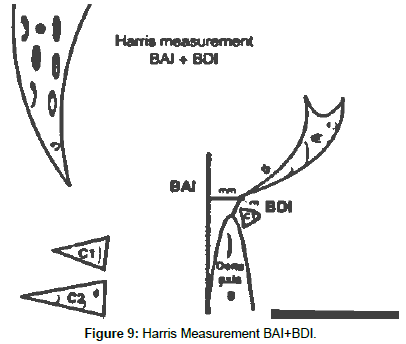
Harris’s method or the rule of 12s:
a) Basion dens interval (BDI)
Distance between inferior and posterior tip of basion and tips of dens.
Pathological:>12 mm
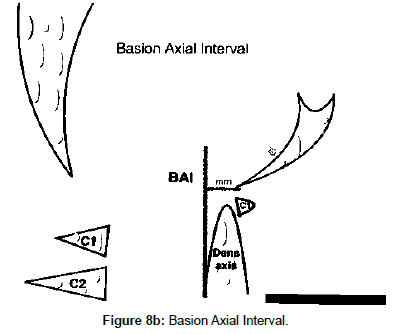
b) Basion axial Interval (BAI)
A vertical line is drawn along the posterior aspect of the odontoid, extending above the level of the foramen magnum (posterior axial line). A perpendicular line is drawn from this posterior axial line to the inferior and posterior tip of the basion and the distance is measured.
Pathological:>12 mm
c) BDI +BAI
For both the BDI and BAI, a value greater than 12mm is indicative of an anterior atanto-occipital dislocation. Pathological:>12 mm
d) Additional, the BAI should be measured in flexion and extension. If the value varies more than 1-2 mm then it means that the head is sliding backwards or forward on cervical spine. Thin slice CT and 3D reconstruction of spine is more reliable for such measurements. Spontaneous reduction of AO dislocation can occur such that any of the above measurement techniques no longer detect it. An increased distance between the posterior elements of C1and C2 may be the only clue on CT (Figure 16).
MRI evaluation reveals ligamentous injury at cranio-cervical junction. Retropharyngeal haematomas can occur in AO dislocation and if these are seen on CT, an MRI scan must be carried out.
X-line method of Lee’s lines: involve assessment of relationship of bony elements at craniocervical junction. Two intersecting lines are drawn, one from tip of basion to anterior aspect of posterior ring of C2 and a second from tip of opisthion to the posterior aspect of C2 body. The first line should pass across the superior -posterior aspect of the odontoid process and the second line should pass just anterio to the posterior portion of the ring of C1 [25,26].
Measuring brain stem compression
Grabb Oaks Line: To diagnose brain stem compression, draw a line on mid sagittal MRI scan from lowest point of the clivus to the lowest posterior point of the axis corpus. Measure a right angle from this line to the beginning of the spinal canal.
Pathological :>8 mm.
Clivo Axial Angle (CXA): Draw a line along the clivus and a second one down on the posterior side of the axis.
Normal angle is between 1500 in flexion and 1800 in extension.
Pathological: <1500 is typical of basi-occipital hypoplasia with a risk of brain stem compression Wackenheim Line: Angle between clivus line and dural canal. This line should go through the dens or be tangential to it [25,26].
Traynelis AO Dislocation classification: Three types of dislocations can occur:
Type I when there is an Anterior displacement of occiput with respect to C1anterior arch. Type II dislocation means a Longitudinal distraction of occiput from C1 and Type III dislocation occurs when dislocates posteriorly with respect to C1. Patients with AO dislocation should be treated to avoid progression of neurological deficit as these are highly unstable fractures. Halo is an alternative in those not fit for surgery. For type II traction is not indicated as it may cause further neurological deficit. For type I or III (with anterior or posterior dislocation respectively), gentle traction to realign the spine may be helpful with no weights. In most just changing the head position the alignment can be normalised. This kind of injury may be associated with Injuries to the vertebral artery, Brain stem, Cervical cord, nerve roots, lower cranial nerves etc. It is usually a fatal injury. Management includes Airway and ventilation. Most patients require internal fixation.
C1 fractures: Jefferson’s fracture
This is relatively common injury constituting approximately 10% of cervical spine injuries. In 50% cases C1 fracture appears in combination with C2 injuries. Isolated C1 fractures rarely cause neurological deficit.
Three most common types are a) Anterior or Posterior arch fractures (31-45%) b) lateral mass fractures (13-37%) and c) Burst fractures involving anterior and posterior ring fractures (also called Jefferson fracture) (37-51%). The integrity of the transverse ligament is crucial in the stability of atlanto –axial complex. This may be assessed on plain x-ray AP view or open mouth view or coronal CT reconstruction by measuring the lateral mass displacement. If the cumulative displacement of the lateral masses is equal or more than 7 mm then the transverse ligament is considered to be incompetent (rule of Spence) [27]. Panjabi’s group 28 found that ADI (atlanto – dens interval) of more than 3.5mm on flexion radiograph is the most reliable predictor of transverse ligament disruption. It can also be diagnosed on MRI scan (Figure 17).
Mechanism: Axial load applied to vertex driving the occipital condyles into lateral masses of C1.
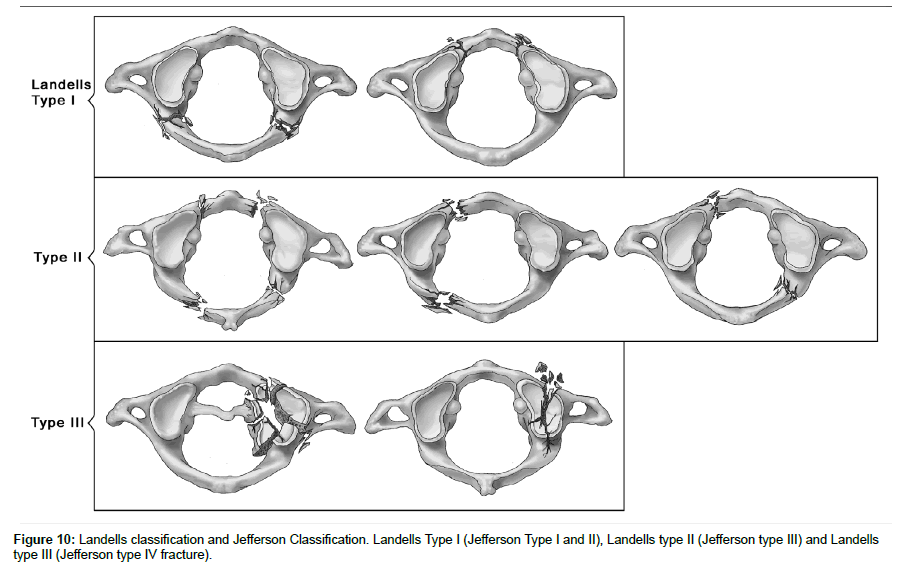
There are many classifications. a) Jefferson Classification b) Landells Classification c) Dickman Classification Jefferson (and Landells) classification
a) Jefferson type I and II fracture (Landells type I fracture): Fracture of the posterior arch at two places and anterior arch at two places respectively.
b) Jefferson Type III fracture (Landells Type II): Burst fracture. This is the classic Jefferson fracture involving fracture of the ring at four places or fracture involving each arch at one place.
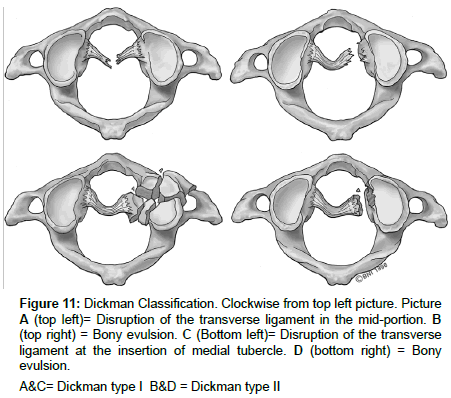
c) Jefferson Type IV fracture (Landells type III): Dickman Classification: This is based on disruption of transverse ligament.
A= Disruption of the transverse ligament in the mid-portion. B = Bony evulsion. C = Disruption of the transverse ligament at the insertion of medial tubercle and D (bottom right) = Bony evulsion. A&C (essentially disruption of the transverse ligament) are classified as Dickman type I fracture whereas B & D involving bony avulsion are classified as Dickman type II fracture.
Diagnosis: Thin slice CT with cuts parallel to C1 arch would demonstrate the type of fracture. X-ray cervical spine Open mouth view Lateral view with flexion and extension should be done to demonstrate or rule out instability (Figure 18).
Treatment: 1) Fractures of the lateral mass with intact transverse ligament should be treated with rigid external immobilisation i.e halo for 8-12 weeks. 2) Communited lateral mass fractures may be better treated in a Halo. This should be followed by dynamic flexion and extension views. If instability demonstrated on flexion extension dynamic views then Occipito-C2 fixation is needed.
3) Fractures of the anterior or posterior arch are also treated according to the integrity of the transverse ligament. ADI of more than 3.5.mm or Lateral mass displacement of more than 7 mm. They can be treated in a rigid cervical collar, SOMI brace or Halo for 3 months.
4) Treatment of Jefferson’s fracture (C1 burst fracture) also depends on integrity of the Transverse ligament. ADI of more than 3.5 mm or lateral mass displacement of over 7 mm on CT or disruption of transverse ligament on MRI indicate instability. a) A Jefferson’s fracture with intact Transverse ligament can be treated in a halo for upto 3 months. b) Jeffersons’ fracture with breached transverse ligament broken can be treated either in a Halo or by internal fixation by any of the techniques described for C1-C2 fixation. (see odontoid fractures) [28] (Figure 19).
Recent publications advocating posterior osteosynthesis of nonunited Jefferson’s fractures have been published. Direct posterior C1 lateral mass screws compression reduction and osteosynthesis is a valid technique, avoiding fusion of upper cervical spine [29,30]. It is suggested that the ideal treatment of unstable Jefferson fractures is expected to preserve the function of C0–C1–C2. Unstable Jefferson fractures involve the concomitant failure of the vertical ligamentous tension because of the loss of C0– C2 height. Reduction of the displaced lateral masses to restore the C0–C2 height and maintain the ligamentous tension is the key to the surgery [29,30]. Dickman Type I injuries need surgical fixation whereas Dickman type II would heal in a halo
Odontoid fractures
Odontoid fractures constitute about 8-18% of all cervical spine injuries with neurological injuries occurring in 10-20%. The incidence of neurological deficit in surviving patients is low, likely due to large diameter of the cervical canal at this level [31]
Due to its special anatomy, the axis (C2) is exceptionally vulnerable at two points, the Odontoid process and the isthmus.
a) The odontoid process (dens) is the only vertebral body type (cancellous) structure in the spine, which must resist forces other than compression. This explains the high incidence of these fractures in osteoporotic spine. Because the C1-C2 connection lacks a real facet joint, the C2 body is connected to the facet of C3 through an elongated pedicle called the isthmus (Figure 20).
b) The motion planes of the proximal and distal joints of C2 also make a sharp angle and have a considerable offset between them. The motion plane of C1-C2 joint is ventral, whereas the C2-C3 joint is dorsal to the spinal canal.
c) This connection is further weakened by the vertebral artery penetrating the axis just at the base of the pedicles. This explains the common occurrence of the traumatic spondylolisthesis of the C2, which is also (erroneously) called the hangman’s fracture [21].
There are two peaks of incidence with distinctive patterns; one in childhood injuries usually as result of hyper-flexion and the other in elderly with hyperextension [32]. C2 fractures are common in elderly and carry a significant in hospital mortality rate probably as high as 25% [33,34].
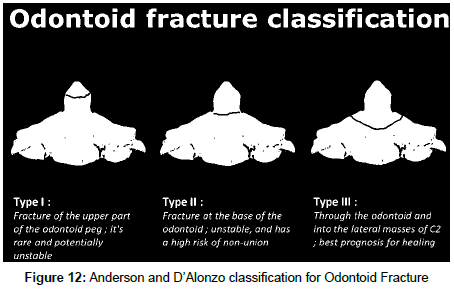
The most common symptom is high cervical pain as neurological deficits are infrequent. However, spinal cord compression may occur due to subluxation of the fracture dens. Maintenance of spinal alignment must be a primary goal of the evaluation and management of these fractures. Anderson and D’Alonzo introduced a classification for Odontoid PEG fracture in 1974.
According to their classification these fractures are divided into Three types. Anderson and D’Alonzo classification for Odontoid Fracture
Type I: are oblique fractures through the Tip of the odontoid above the synchondrosis (where dens fuses with the body). Although uncommon they may be the result of an avulsion fracture of the alar ligaments as part of an occipito-cervical dissociation. They represent less than 1% of odontoid fractures. These are treated in a Cervical Collar. There is a 100% fusion irrespective of the type of external immobilisation.
Type II: Majority of Odontoid Fractures fall in this category. The Fracture occurs at the junction of the dens with the body of axis (synchondrosis). Blood supply may be affected. There is a small area for fracture healing. This fracture has a high rate of non-union. The average fusion rate is about 57%. Treatment options for type II Odontoid fracture are 1) Halo. 2) Internal fixation (surgery) 3) Collar in patients who are not fit for surgery or halo or are very old i.e., over the age of 85 years rauer and colleagues 35 proposed an alternative modification to the Anderson and D’ Alonzo classification to better define suitability of treatment options such as anterior odontoid screw placements. This can be further subdivided into three subtypes according to the morphology of fracture.
Type IIA: Minimally or non-displaced type II fractures with no communition and less than 1.0mm displacement. Treatment: These fractures can be treated conservatively. Type IIB: displaced fractures extending either antero-superior to postero-inferior or transverse fractures. Treatment: These [22].
Fractures are suitable for anterior screw placement. Type IIC: Fractures extending from antero-inferior to postero-superior or a fracture with significant communition of the dens. Treatment: These fractures are treated with posterior atlanto axial stabilisation. Risk factors associated with non-union of type II odontoid fracture include
a) Displacement: Type II fracture with displacement of more than 6 mm had 67% non-union.
b) Age: more than 50 had 21 times higher rate of non-union than those <50years. Anderson and colleague noted poor union rates in elderly patients treated non-surgically and further noted that posterior approaches were superior in this age group c) Poor blood supply [36]. e) Failure to maintain adequate spinal alignment after traction and external immobilisation is also an indication of surgical intervention. Surgical options for type II Fractures are as follows: A. Posterior approach: If the fracture is Communited, and/or the Transverse Ligament is breached or the fracture orientated anteroinferior to postero-superior then Anterior Screw fixation is not possible. In that case a Posterior C1-C2 fixation is the best option.
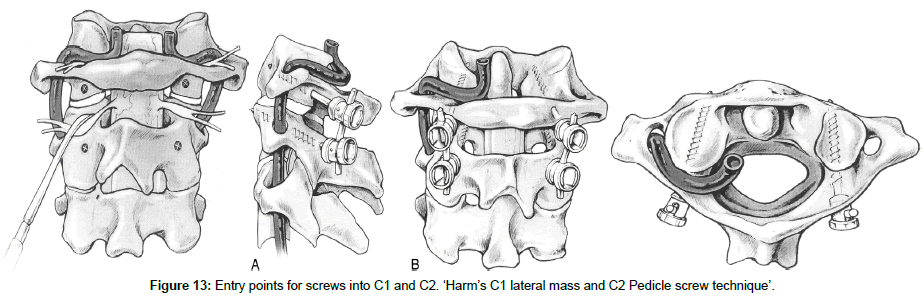
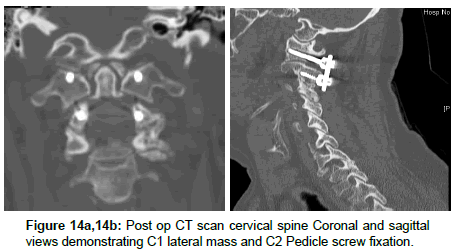
Any of the techniques of the Posterior approaches mentioned below could be used. a) Posterior atlanto axial wiring techniques such as C1-C2 ‘Galle fusion’ or ‘Sonntag’ methods. b) Magerl C1-C2 transarticular screws technique [37]. c) The ‘Harms’ C1 lateral mass- C2 pedicle screw technique [38]. d) Occipito-cervical fixation.
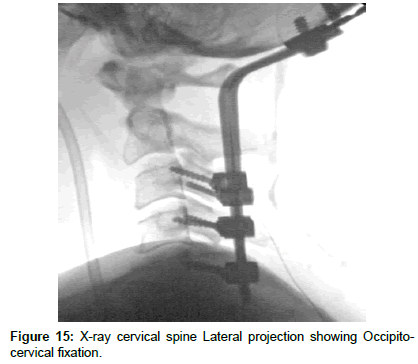
d) Occipito-cervical fixation. If the lateral masses of either C1 or C2 and/ or the body of C2 if also fractured then the only option is to fox the occiput to subaxial spine. X-ray cervical spine Lateral projection showing Occipito-cervical fixation [23].
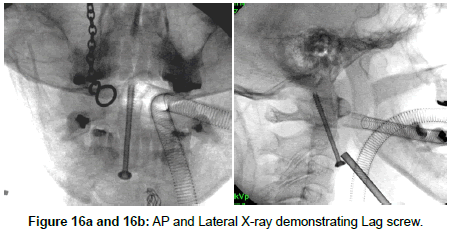
B. Anterior Approach: Trans-odontoid Lag Screw Indications: If the Transverse Ligament is intact and the fracture line is either transverse or antero-superior to postero-inferior then the best option is Anterior Screw fixation using a Lag screw
AP and Lateral X-ray demonstrating Lag screw
Type III: Fractures extend through the dens and into the body of C2 (axis). Anderson and D’Alonzo stated that type III odontoid fractures should be considered fractures of the body of C2. These fractures have a high fusion rate with external immobilisation. Majority are treated with a halo. Displacement of more than 5 mm may need early surgical fixation. Fusion rate is approximately 88%. Older age, initial non-surgical treatment, and male sex are associated with failure of treatment in patients with geriatric odontoid fractures [39]. The data suggests a significant 30-day survival advantage and a trend toward improved longer-term survival for operatively treated over non-operatively treated patients [40]. There may be a suggestion that even in the elderly age group surgery should be considered as a preferred option. This is certainly the opinion of the author.
Traumatic Spondylolisthesis of the Axis (Traumatic Hangman’s Fracture):
A hangman’s fracture is the colloquial name given to a fracture of the pedicles or pars inter-articularis (isthmus) of the axis (C2 vertebra). Scheider et al. coined the term ‘hangman’s fracture’ in 1965 in their series of eight patients whose injuries mimicked the fracture pattern of judicial hanging described by Wood-Jones in the first volume of Lancet in 1913 [41,42].
Hangman’s Fracture is essentially a traumatic bilateral spondylolisthesis of the pars interarticularis of the axis or C2 secondary to hyperextension and compression with axial loading that is often seen with motor vehicle accidents, falls and diving accidents [43].
The classic example are those of an unrestrained occupant in a motor vehicle accident who is thrown forward and hits the windshield, or a swimmer who dives and the hits the bottom of a shallow pool. In both instances the combined forces of hyperextension and axial compression occur. The fracture seen in trauma is similar to that induced by judicial hangings. However, the true judicial hangman’s fracture results from distraction and hyperextension and not compression and 24 hyperextension. These fractures involve anatomic disruption and bilateral pars inter-articularis fracture. Hangings produce injury to vertebral arteries and cervico-medullary junction. The fractures due to RTA are not associated with neurological deficit.
Classification: The most commonly used scheme is the Effendi classification modified by Levine and Edwards 44. Effendi and colleagues describe three types on the basis of mechanism of injury (Type I axial loading; Type II Hyperextension and rebound flexion and Type III hyper-flexion and rebound extension) [44].
Levine and Edwards modified this classification such as that type I injuries resulted from an initial hyperextension-axial-loading force, type II injuries from an initial hyperextension-axial loading force followed by severe flexion, type IIa injuries from flexion –distraction and type III injuries from flexioncompression [45]. This scheme is based on the morphology, presumed mechanism of injury, and the measured amount of angulation and translation between C2 and C3.
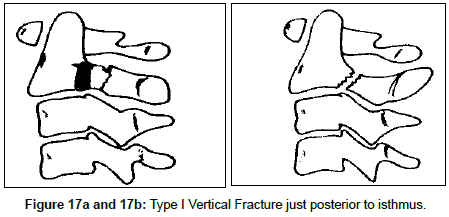
Type I: The fracture is through the isthmus just posterior to the body and the fracture line is vertical.
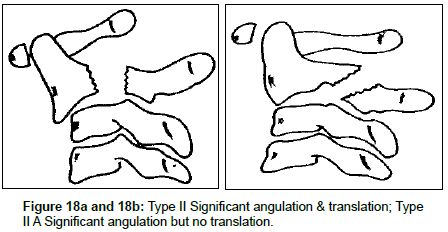
Type II: These injuries show significant angulation and more than 3 mm translation. Fracture lines are similar to type 1 and are predominantly vertical. Type IIA: there is little or no translation but a significant angulation. The direction of fracture line is oblique running from anterio-inferior to posterosuperior.
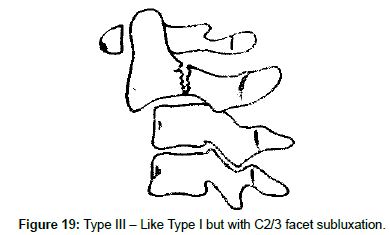
This injury is a result of flexion- distraction forces. Type III: Several configurations. a) Most common is Type I fracture with bilateral dislocation of C2- C3 facet joints. b) Another type is Unilateral facet dislocation and contralateral isthmus fracture.
Treatment: Class III evidence shows that almost all hangman’s fractures heal with traction and when necessary followed by 12 weeks of external cervical immobilisation with a rigid cervical collar or more commonly with a halo. Surgery for Hangman’s fractures is reserved for significant C2-C3 disc disruption, failure to induce or maintain reduction, or non-union following halo immobilisation. Surgical options are a) C2-C3 anterior cervical discectomy with fusion and b) C1-C3 posterior fusion techniques.
There is recent evidence to suggest that the anterior procedure seems to be superior to the posterior approach for unstable hangman’s fracture as it is a less invasive and simpler procedure with fewer complications, and is especially indicated for cases with no medullary canal in C2 pedicles and in cases with traumatic C2-3 disc herniation compressing the spinal cord [46].
In the posterior approaches, C2-C3 group showed better clinical and biomechanical results than C1-C3 group in terms of axial pain and disability of neck [47].
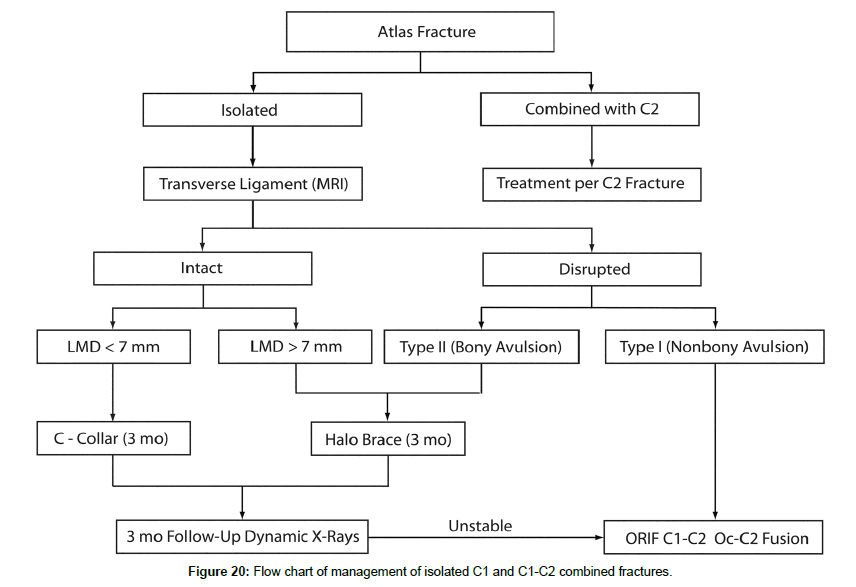
Management of combined C1-C2 fractures
Fractures of C1 occur in up to 53% of type II and Type III odontoid fractures. Similarly Odontoid fractures are noted in up to 50% of patients with C1 fractures. Combined C1-C2 injuries have higher rates of death and neurological deficit than isolated fractures of C1 and C2 consistent with the presumed higher degree of force necessary to precipitate combination fractures [48,49].
Stability of C1-C2 junction: ADI (Atlanto-Dens Interval) is the distance between posterior surface of anterior arch C1 and anterior surface of odontoid process normally is 3mm in adults or more than 4.5mm in children. If the ADI is more than 3mm in adults or 4.5mm in children then it indicates incompetence of the transverse ligament and C1-C2 junction is considered to be unstable. Factors which determine the treatment of Atlanto-axial instability are: a) Age b) Neurology. c) Degree of spinal deformity d) Reduction e) Presence of spinal cord compression and f) Overall medical condition
Treatment options
The management of combined fractures of C1-C2 is dictated in principle by characteristics of C2 fracture. Halo immobilisation: Most C1-C2 combination injuries can be treated with external immobilisation. Surgery for C1-C2 injuries is reserved for a) ADI of more than 5mm. b) Angulation of more than 11 degrees and c) non-union after non-surgical management. The surgical approach is again dictated by the appropriate approach for C2 injury.
Reducible instabilities are treated by any of the following options
1. Posterior fixation/fusion: Either by a) Tran-articular screw fixation. b) C1/C2 lateral mass screws with a rod.
Conclusion
The anatomy of the occipito-cervical junction involves very strong ligaments connecting the occiput to C1 and to C2. It therefore requires a very strong force to result in occipito-cervical bony or ligamentous injuries. Occipito-cervical injuries must be suspected in high velocity injuries like RTAs and also in the elderly with neck pain and stiffness following a fall. Conventional cervical spine plain films miss between 50- 93% of occipital condyle fractures, which are also the most common cervical spine fracture missed by radiology residents. There is a need to have a high index of suspicion of such injuries in patients with dangerous mechanism of injury as elaborated by NICE guidelines mentioned above. With routine CT scan in high energy trauma the spectrum of this disease has become much better elucidated. Recent trend seem to favour early surgical management of occipito-cervical injuries. Although most Jefferson’ fractures heal in a Halo, recent publications advocate surgical treatment (posterior osteosynthesis) for non-united Jefferson’s fractures. There are no established protocols for management of C2 fractures or even in the choice of surgical approaches. Although majority fractures would heal in a halo, it does have a significant morbidity.
There is recent evidence to suggest that surgical management of odontoid fractures has better outcome even in the elderly. Aim should be surgical fixation of Odontoid fractures wherever possible even in elderly patients if there is no significant co-morbidity or contraindication for surgery. Type II transverse fractures of Odontoid with intact transverse ligament should be offered Anterior lag screw fixation. Oblique odontoid fractures with doubtful integrity of transverse ligament but intact lateral masses and body of C2 should be treated with posterior C1 lateral mass- C2 pedicle screw fixation. Communited fractures of C2 involving the body or lateral mass or those combined with C1 fractures should be treated with Occipito-Cervical fixation.
References
- World Health Organization (2009) World Health Report 2009.
- Krug EG, Sharma GK, Lozano R (2010) The global burden of injuries. Am J Public Health 90: 523-526.
- Pirouzmand F. Epidemiological trends of spine and spinal cord injuries in the largest Canadian adult trauma center from 1986 to 2006. J Neurosurg Spine 12: 131-140.
- Lenehan B, Boran S, Street J, Higgins T, McCormack D, et al. (2009) Demographics of acute admissions to a National Spinal Injuries Unit. Eur Spine J 18: 938-942.
- Hu R, Mustard C, Burns C (1996) Epidemiology of incident spinal fracture in a complete population. Spine 21: 492-499.
- Hu R, Mustard CA, Burns C (1996) Epidemiology of incident spinal fracture in a complete population. Spine 21: 492-499.
- Dryden DM, Saunders LD, Rowe BH, May LA, Yiannakoulias N, et al. (2003) The epidemiology of traumatic spinal cord injury in Alberta, Canada. Can J Neurol Sci 30: 113-121.
- Jackson AB, Dijkers M, Devivo MJ, Poczatek RB (2004) A demographic profile of new traumatic spinal cordinjuries: change and stability over 30 years. Arch Phys Med Rehabil 85(11): 1740-1748.
- Pickett W, Simpson K, Walker J, Brison RJ (2003) Traumatic spinal cord injury in Ontario, Canada. J Trauma. 55(6): 1070-1076.
- Schinkel C, Frangen TM, Kmetic A, Andress HJ, Muhr G, et al. (2007) Spinal fractures in multiply injured patients: an analysis of the German Trauma Society’s Trauma Register. Unfallchirurg 110: 946-952.
- Hasler RM, Exadaktylos AK, Bouamra O, Benneker LM, Clancy M (2011) Epidemiology and predictors of spinal injury in adult major trauma patients: European cohort study. Eur Spine J 20: 2174-2180.
- De Vivo MJ, Rutt RD, Black KJ (1992) Trends in spinal cord injury demographics and treatment outcomes between 1973 and 1986. Arch Phys Med Rehabil 73: 424-430.
- Huelke DF, O’Day, Mendelsohn RA (1981) Cervical injuries suffered in autobobile crashes. J Neurosurg 54: 316-322.
- Cranio-vertebral Junction: Anatomy and Radiology
- Spinal injury: assessment and initial management.
- Bell C (1817) Surgical observations. Middlesex Hospital J 4: 469-470.
- Bucholz RW,Burkhead WZ (1979) The pathological anatomy of fatal atlanto-occipital dislocations. J Bone Joint Surg Am 61: 248-250.
- Hanson JA, Deliganis AV, Baxter AB (2002) Radiological and clinical spectrum of occipital condyle fractures: retrospective review of 107 consecutive fractures in 95 patients. AJR Am J Roentgenol 178: 1261-1268
- DiazJJ, Gillman C, Morris JA, May AK, Carrillo YM, et al. (2003) Are five-view plain films of the cervical spine unreliable? A prospective evaluation in blunt trauma patients with altered mental status. J Trauma 55: 658-663.
- Goradia D, Blackmore CC, Talner LB, Bittles M, Meshberg E (2005) Predicting radiology resident errors in diagnosis of cervical spine fractures. Acad Radiol 12: 888-893
- Anderson PA, Montesano PX (1988) Morphology and treatment of occipital condyle fractures. Spine 13: 731-736.
- Tuli S, Tator CH, Fehling MG, Mackay M (1997) Occipital condyle fractures. Neurosurgery 41: 368- 376.
- Alcelik I, Manik KS, Sian PS (2006) Occipital Condylar fractures review of the literature and case report. J Bone Joint Surg Br 88: 665-669.
- Fisher CG, Sun JC, Dvorak M (2001) Recognition and management of altalnto-occipital dislocation: improving survival from an often fatal condition. Can J Surg 44: 412-420.
- Weismann M, Linn J, Bruckmann H (2013) Atlas Klinische Neuroradiologie: Wirbelsaule und Spinalkanal. Springer-Verlag 30.
- Panjabi MM, White III AA (1980) Basoc biomechanics of the spine. Neurosurgery 7: 76-93.
- Spence KF, Decker S, Sell KW (1970) Bursting atlantal fracture associated with rupture of the transverse ligament. J Bone Joint Surg Am 52: 543-549.
- Oda T, Panjabi MM, Crisco JJ III, Oxland TR, Katz L (1991) Experimental study of atlas injuries: Relevance to clinical diagnosis and treatment. Spine 16: S466-S473.
- Abeloos L, Witte OD, Walsdorff M (2011) Posterior Osteosynthesis of the Atlas for Non-consolidated Jefferson Fractures. Spine 36: E1360-E1363
- Li L, Teng H, Pan J, Qian L (2011) Direct Posterior C1 lateral mass Screws Compression Reduction and Osteosynthesis in the Treatment of Unstable Jefferson Fractures. Spine Lippincott Williams and Wilkins 36: E1046-E1051.
- Harrop JS, Sharan AD, Przybylski GJ (2000) Epidemiology of spinal cord injury after acute odontoid fracture. Neurosurg Focus 8: E4.
- Maak TG, Grauer JN (2006) The contemporary treatment of odontoid injuries. Spine 31: 553-560.
- Tashjian RZ, Majercik S, Biffl WL, Palumbo MA, Cioffi WG (2006) Halo-west immobilisation increases early morbidity and mortality in elderly odontoid fractures. J Trauma 60: 199-203.
- Muller EJ, Wick M, Russe O, Muhr G (1999) Management of odontoid fractures in the elderly. Eur Spine J.
- Grauer JN, Shafi B, Hilibrand AS (2005) Proposal of a modified treatment-orientated classification of odontoid fractures. Spine J 5:123-129.
- Andersson S, Rodrigues M, Olerud C (2000) Odontoid fractures: high complication rate associated with anterior screw fixation in the elderly. Eur Spine J 9: 56-59.
- Magerl F, Seeman PS. Stable posterior fusion of the atlas and axis by transarticular screw fixation. In: Kher, ed. Cervical Spine. New York: Springer- Verlag: 1987.
- Harms J, Melcher RP (2001) Posterior C1-C2 fusion with polyaxial screw and rod fixation. Spine 26: 2467-2471.
- Fehlings MG, Arun R, Vaccaro AR, Arnold PM, Chapman JR, et al. (2013) Predictors of treatment outcomes in geriatric patients with odontoid fractures: A O Spine North America multi-centre prospective GOF study. Spine 38: 881-886.
- Chapman J1, Smith JS, Kopjar B, Vaccaro AR, Arnold P, et al. (2013) The A O Spine North America Geriatric Odontoid Fracture Mortality Study: a retrospective review of mortality outcomes for operative versus non-operative treatment of 322 patients with long-term follow-up. Spine 38:1098-1104.
- Schneider RC, Livingston KE, Cave AJ, Hamilton G (1965) “Hangman’s fracture” of the cervical spine. J Neurosurg 22: 141-154.
- Wood-Jones F (1913) The ideal lesion produced by judicial hanging Lancet 1: 53.
- Levine AM (1998) Traumatic Spondylolisthesis of the axis. “hangman’s fracture”. In: The Cervical Spine Research Society Editorial Committee (3rd edtn) Philadelphia: Lippincott-Raven 429-448.
- Effendi B, Roy D, Cornish B, Dussault RG, Laurin CA (1981) Fractures of the ring of the axis.: a classification based on the analysis of 131 cases. J Bone Joint Surg Br 63-B: 319-327.
- Levine AM, Edwards CC (1985) The management of traumatic spondylolisthesis of the axis. J Bone Joint Surg Am 67: 217-226.
- Ge C, Hao D, He B, Mi B (2014) Anterior Cervical Discectomy and Fusion Versus Posterior Fixation and Fusion of C2-3 for Unstable Hangman's Fracture. J Spinal Disord Tech.
- Park JH, Kim SH, Cho KH (2014) Clinical Outcomes of Posterior C2-C3 Fixation for Unstable Hangman's Fracture Compared with Posterior C1-C3 Fusion. Korean J Spine 11:33-38.
- Dickman CA, Haldey MN, Browner C, Sonntag VK (1989) Neurological management of acute atlas-axis combination fractures: a review of 25 cases. J Neurosurg 70: 45-49.
- Fujimura Y, Nishi Y, Chiba K, Kobayashi K (1995) Prognosis of neurological deficits associated with upper cervical spine injuries. Paraplegia 33: 195-202.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi