Case Report, Analg Resusc Curr Res Vol: 12 Issue: 1
Decompressive Craniectomy Together with Blood Component Transfusion as a Life-Saving Treatment for a Severe Traumatic Brain Injury Patient with Coagulopathy: A Case Report
Yu Hao1, Guangshan Hao2, Jianxin Zhu2, Shubao Zhang2* and Suna Yin3
1Department of Clinical Laboratory, Liaocheng People’s Hospital, Shandong, China
2Department of Neurology, Liaocheng People's Hospital, Shandong, China
3Department of Operating Room, Liaocheng Veterans Hospital, Shandong, China
*Corresponding Author: Shubao Zhang
Department of Neurology, Liaocheng People's Hospital, Shandong, China
E-mail: zsbysn@163.com
Received date: 23 November, 2022, Manuscript No. ARCR-22-80844;
Editor assigned date: 28 November, 2022, PreQC No. ARCR-22-80844 (PQ);
Reviewed date: 12 December, 2022, QC No. ARCR-22-80844;
Revised date: 23 January, 2023, Manuscript No. ARCR-22-80844 (R);
Published date: 30 January, 2023, DOI: 10.3584/2324-903X.1000151
Citation: Hao Y, Hao G, Zhu J, Zhang S, Yin S (2023) Decompressive Craniectomy Together with Blood-Component Transfusion as a Life-Saving Treatment for a Severe Traumatic Brain Injury Patient with Coagulopathy: A Case Report. Analg Resusc: Curr Res 12:1.
Abstract
Severe Traumatic Brain Injury (TBI) accompanied by impaired hemostasis, is a devastating and challenging emergency, due to its complicated mechanisms and lack of specific guidelines. Adequate and timely treatment is thought to be linked to improved survival. Herein, we report a 28-year-old Chinese man presenting with severe TBI accompanied by coagulopathy on admission. After administration of tranexamic acid and simultaneous blood-component therapy, the patient underwent decompressive craniectomy and evacuation of hematoma together with extensive temporal lobectomy. The surgical procedure went smoothly without uncontrollable bleeding, and the patient made a successful postoperative recovery without unexpected, delayed intracranial hemorrhage.
Keywords: Traumatic brain injury; Decompressive craniectomy; Coagulopathy; Tranexamic acid; Blood-component therapy
Introduction
Decompressive craniectomy or hemicraniectomy is an effective surgical intervention for increased Intracranial Pressure (ICP) in severe Traumatic Brain Injury (TBI) and other neurological disorders that cause malignant cerebral edema and midline shift [1]. In that light, evacuation of intracranial hematoma and resection of the temporal lobe are integrative parts of an effective ICP control in severe TBI. Coagulopathy is a common but serious complication after severe TBI, not only influencing emergent surgical intervention but also accompanying a poorer prognosis [2]. However, there are still no specific guidelines for the treatment of TBI associated increase in ICP occurring along with coagulopathy. Herein, we present the successful management of a case with severe TBI and coagulopathy on admission [3].
Case Presentation
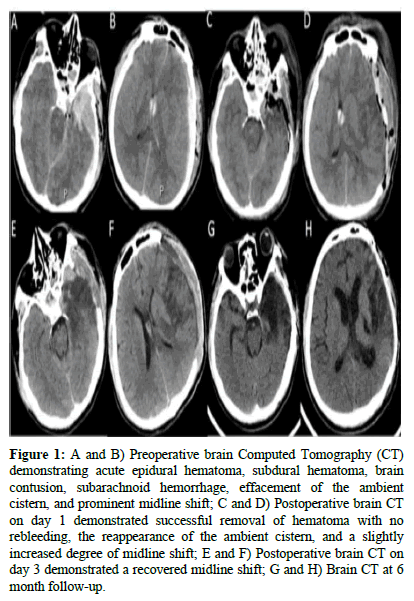
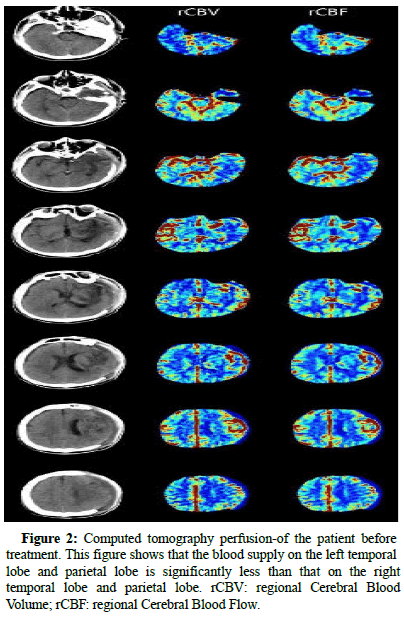
A 28-years-old Chinese man lost control of his fastmoving motorcycle and fell down the road. He was presented to our emergency department with endotracheal intubation performed in the ambulance. Upon admission, the patient was in a deep coma with a Glasgow Coma Scale score (GCS) of 4 and bilaterally fixed mid-size pupils. Computed Tomography (CT) of the head revealed acute epidural hematoma, subdural hematoma, brain contusion, subarachnoid hemorrhage, effacement of the ambient cistern, prominent midline shift, and severe secondary brain injury (Figure 1). No evidence of any other bone fractures and organ injuries was detected on further imaging tests. CT perfusion of the patient before treatment revealed that the blood supply on the left temporal and parietal lobes was significantly less than that on the right counterparts (Figure 2). As an emergent procedure for brain herniation, 25 grams of mannitol was immediately administrated to the patient [4]. The patient’s conventional coagulation tests are presented in Table 1. These tests demonstrated impaired hemostasis. After the administration of 1 gram of tranexamic acid, the patient underwent decompressive craniectomy for hematoma evacuation together with extensive temporal lobectomy. Four units of packed red blood cells and 600 ml of Fresh Frozen Plasma (FFP) were transfused at the same time. The operation went smoothly without uncontrollable bleeding. Five hours after the initial one, another test was performed demonstrating improved coagulation function. The patient was transferred to the intensive care unit and received standard care [5]. A postoperative brain CT scan demonstrated the successful removal of hematoma with no re-bleeding, the reappearance of the ambient cistern, and a slightly increased midline shift. No special treatment was prescribed given the gradually improving nature of the condition and the recovered midline shift indicated by further CT review. Two days after surgery, pupil diameter (left) decreased from 5 mm to 3 mm and GCS increased to 5. However, the light reflex started to recover on day 3. Two months after surgery, the patient underwent successful cranioplasty. At the 6 months follow-up, the patient needed assistance for daily activities with right-sided hemiparesis and broca's aphasia, corresponding to a Glasgow Outcome Scale (GOS) score of 3 (Figure 3).
Figure 1: A and B) Preoperative brain Computed Tomography (CT) demonstrating acute epidural hematoma, subdural hematoma, brain contusion, subarachnoid hemorrhage, effacement of the ambient cistern, and prominent midline shift; C and D) Postoperative brain CT on day 1 demonstrated successful removal of hematoma with no rebleeding, the reappearance of the ambient cistern, and a slightly increased degree of midline shift; E and F) Postoperative brain CT on day 3 demonstrated a recovered midline shift; G and H) Brain CT at 6-month follow-up.
Figure 2: Computed tomography perfusion-of the patient before treatment. This figure shows that the blood supply on the left temporal lobe and parietal lobe is significantly less than that on the right temporal lobe and parietal lobe. rCBV: regional Cerebral Blood Volume; rCBF: regional Cerebral Blood Flow.
| Time | Prothrombin time | Prothrombin time activity ratio | INR | Prothrombin time activity | aPTT | aPTT ratio | Fibrinogen | Thrombin time | D-dimer | Fibrinogen degradation product |
|---|---|---|---|---|---|---|---|---|---|---|
| 1st day evening | 15.1 | 1.4 | 1.41 | 65 | 72.2 | 2.33 | 0.41 | 27.6 | 67.1 | 182.7 |
| 4 hours later | 12.9 | 1.2 | 1.21 | 82 | 37.4 | 1.21 | 1 | 19.4 | 53.3 | 115.4 |
| 1 day later | 11.8 | 1.1 | 1.1 | 94 | 35.2 | 1.14 | 2.03 | 15.6 | 15.9 | 37.2 |
| 1 month later | 13.5 | 1.3 | 1.26 | 77 | 33.8 | 1.09 | 3.99 | 12.4 | 4.8 | 7.6 |
| 3 months later | 9.9 | 0.9 | 0.93 | 126 | 34.3 | 1.11 | 3 | 14.8 | 0.4 | 0.4 |
Table 1: Evolution of hemostatic profile of the patient through time in our center. INR: International Normalized Ratio; aPTT: activated Partial Thromboplastin Time.
Discussion
Decompressive craniectomy is considered an effective treatment for malignant intracranial hypertension in severe TBI, significantly decreasing mortality. However, poor outcome after the surgery is rather common [6]. Technically, the surgery includes frontotemporoparietal craniotomy and a wide opening of dura mater. Evacuation of intracranial hematoma and extensive resection of the temporal lobe up to 45 mm from its tip on the dominant side or 55 mm on the nondominant side are suggested for effective ICP control. In the current case, anterior temporal lobectomy, about 35 mm from the tip, was performed to provide effective ICP control [7].
Secure hemostasis is critical for achieving a favorable outcome in patients with severe TBI. Coagulopathy is a serious complication of TBI, occurring in about two-thirds of patients with severe TBI and causing secondary injury and high mortality. This includes a combination of hypocoagulopathy linked to hemorrhagic progression and hypercoagulop-athy associated with a prothrombotic state. Massively released cerebral tissue factors, platelet dysfunction, hyperfibrinolysis, shock, hypoperfusion, and iatrogenic factors may play a prominent role in TBI associated coagulopathy. Accordingly, timely correction of hemostasis disorder is independently linked to decreased mortality in TBI patients. In this regard, tranexamic acid has shown beneficial effects on the control of hemorrhagic growth and fatality when administrated during the first 3 hours after TBI. Also, blood component therapy is another option for the treatment of TBI associated coagulopathy with a suggested blood component ratio of 1:1:1 (packed red blood cell concentrates: fresh frozen plasma: platelet concentrates). In our case, the patient presented with no platelet deficiency. Thus only the packed red blood cell concentrates and an equal amount of FFP were transfused. There was no uncontrollable intraoperative bleeding, and the patient showed a good postoperative recovery without unexpected, delayed intracranial hemorrhage [8].
Conclusion
Sufficient de-compressive craniectomy, together with extensive temporal lobectomy, should be considered a lifesaving treatment strategy for cases with severe TBI, accompanied by malignant cerebral edema and apparent midline shift. Meanwhile, tranexamic acid together with blood component transfusion may serve as an effective treatment option in cases of TBI associated coagulopathy that occurs in previously healthy young patients.
Conflict of Interest
The authors declare no conflict of interest.
References
- Venturini S, Hutchinson P, Kolias AG (2021) Decompressive craniectomy in the management of traumatic brain injury. Traumatic Brain Injury, Springer, Cham, 205-214.
- Maegele M, Schochl H, Menovsky T, Marechal H, Marklund N, et al. (2017) Coagulopathy and haemorrhagic progression in traumatic brain injury: Advances in mechanisms, diagnosis, and management. Lancet Neurol 16:630-647.
[Crossref] [Google Scholar] [PubMed]
- Hutchinson PJ, Kolias AG, Tajsic T, Adeleye A, Aklilu AT, et al. (2019) Consensus statement from the international consensus meeting on the role of decompressive craniectomy in the management of traumatic brain injury: Consensus statement. Acta Neurochir (Wien) 161:1261-1274.
[Crossref] [Google Scholar] [PubMed]
- Al-Otaibi F, Baeesa SS, Parrent AG, Girvin JP, Steven D (2012) Surgical techniques for the treatment of temporal lobe epilepsy. Epilepsy Res Treat 2012:374848.
[Crossref] [Google Scholar] [PubMed]
- van Gent JAN, van Essen TA, Bos MHA, Cannegieter SC, van Dijck J, et al. (2020) Coagulopathy after hemorrhagic traumatic brain injury, an observational study of the incidence and prognosis. Acta Neurochir (Wien) 162:329-336.
[Crossref] [Google Scholar] [PubMed]
- Epstein DS, Mitra B, Cameron PA, Fitzgerald M, Rosenfeld JV (2016) Normalization of coagulopathy is associated with improved outcome after isolated traumatic brain injury. J Clin Neurosci 29:64-69.
[Crossref] [Google Scholar] [PubMed]
- Perel P, Al-Shahi Salman R, Kawahara T, Morris Z, Prieto-Merino D, et al. (2012) CRASH-2 (Clinical Randomisation of an Antifibrinolytic in Significant Haemorrhage) intracranial bleeding study: The effect of tranexamic acid in traumatic brain injury a nested randomised, placebo-controlled trial. Health Technol Assess 16:01-54.
[Crossref] [Google Scholar] [PubMed]
- Jokar TO, Khalil M, Rhee P, Kulvatunyou N, Pandit V, et al. (2016) Ratio based resuscitation in trauma patients with traumatic brain injury: Is there a similar effect? Am Surg 82:271-277.
[Google Scholar] [PubMed]
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi